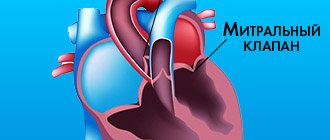
Pathology is recorded in children and adult patients and is detected by listening to the heart or during a targeted laboratory diagnostic examination. Violation of the elasticity of the leaflets in the mitral valve of the left atrium is called prolapse; deviation is observed during the contractile mechanism of the left ventricle.
Types of disease
Experts distinguish primary and secondary forms of mitral valve prolapse; the lesion can affect the anterior, posterior or both leaflets. Three degrees of pathology are observed:
- the first - with sagging of the valves from 3 to 6 mm;
- the second – from 6 to 9 mm;
- the third is more than 9 mm.
The disease is divided according to the rate of blood return:
- first degree – in the area of the valves;
- the second - in the middle of the left atrium;
- the third is at the opposite end of the atrium.
The initial lesion includes grade 1 mitral valve prolapse.
Mitral valve prolapse
Mitral valve prolapse has several forms: congenital and acquired, primary (idiopathic), which is most often detected during a comprehensive examination, but it is not associated with any disease, as well as secondary, which develops as a complication or one of the manifestations of the primary disease ( rheumatism, non-rheumatic carditis, infective endocarditis, cardiomyopathy, hereditary connective tissue diseases - Marfan syndrome, Ehlers-Danlos syndrome, myocardial infarction, myocardial dystrophy, myocardiosclerosis, etc.). Primary mitral valve prolapse has “auscultatory” forms, which are characterized by pronounced symptoms, and “silent” forms - scanty symptoms appear, revealed only by echocardiographic examination.
The cause of prolapse of the mitral valve leaflets is myxomatous degeneration of both the valvular structures of the heart and the intracardiac nerve fibers of the conduction system of the heart. Myxomatous degeneration manifests itself in the form of diffuse damage to the fibrous layer, destruction and fragmentation of collagen and elastic fibers, and increased accumulation of glycosaminoglycans in the extracellular matrix. Excessive accumulation of type III collagen is found in the affected valves. These factors reduce the density of myxomatous tissue. Myxomatous degeneration increases with age and is considered one of the causes of leaflet perforation and mitral valve chord rupture in people over 40 years of age.
Prolapse can also be caused by functional phenomena: regional impairment of contractility and relaxation of the left ventricular myocardium - lower basal hypokinesia, abnormal contraction - inadequate contraction of the long axis of the left ventricle, premature relaxation of the anterior wall of the left ventricle, etc. The cause of such disorders is inflammatory and degenerative changes (myocarditis, asynchronism of excitation and conduction of impulses, heart rhythm disturbances, etc.), disturbances of the autonomic innervation of subvalvular structures and psycho-emotional deviations. Left ventricular dysfunction in adolescents may appear due to impaired blood flow as a result of the development of fibromuscular dysplasia of the small coronary arteries and topographic abnormalities of the left circumflex artery.
The development of MVP is also influenced by electrolyte disorders, which include: interstitial magnesium deficiency, which has severe clinical manifestations. Interstitial magnesium deficiency affects the production of defective collagen by fibroblasts in the mitral valve leaflets.
But most often the cause of MVP is considered to be congenital connective tissue insufficiency of its structures and minor anatomical anomalies of the valve apparatus, as well as disorders of the neurovegetative regulation of mitral valve function.
Primary MVP refers to an independent hereditary syndrome, which was formed as a result of a congenital disorder of fibrillogenesis. It is part of a group of isolated anomalies that arise against the background of congenital connective tissue disorders.
Secondary mitral valve prolapse is a rare phenomenon, but occurs with rheumatic damage to the mitral valve, Ebstein's anomaly, which is caused by both direct damage to the valve and the development of valvular-ventricular disproportion and hemodynamic abnormalities.
Prolapse of the mitral valve leaflets occurs for three reasons:
- defectiveness of the frame function of the connective tissue structures of the valve, due to which, when loaded with pressure, the valve structures are excessively bent, stretched or bulge;
- violations of the ratio of area, thickness, length and correct location relative to each other of all components of the valve;
- disorders of neuroendocrine regulation of the functioning of all components of the valve structure.
In patients diagnosed with MVP, there is a defect in the connective tissue structures of the valve, which include: expansion of the valve fibrous ring, an increase in the area of the valve leaflets, their “redundancy”, pronounced scalloping (“shaggyness”) of the posterolateral valve leaflet, which explains its more frequent prolapse. If the valves become longer or the chords become thinner, they may come off. With MVP, there is a shift in localization and a decrease in contractility of the papillary muscles, a violation of the coordinated functioning of valve structures, therefore, mitral valve prolapse often manifests against the background of neurocirculatory dystonia and psychoemotional disorders.
Prolapse depends on the degree of filling of the left ventricle with blood and its end-diastolic volume. The convergence of the components of the left ventricle occurs due to the rapid heart rate, severe hyperkinesia, and small filling of the ventricle. This explains the high intensity of “clicks”. Also, with MVP, hemodynamic disorders, shifts, volume overload of the left atrium and left ventricular failure are observed.
Doctors identify a “silent” form. It may be detected incidentally during echocardiographic examination. There is also an auscultatory form, which is characterized by auscultatory and phonocardiographic “clicks” and noises. The etiology includes: primary prolapse (familial, non-familial, Marfan syndrome, etc.) and secondary prolapse (rheumatism, ischemic heart disease, cardiomyopathy). MVP is graded according to the severity (in mm) of leaflet flexion and the degree of mitral regurgitation. From all of the above, the following changes in the heart can be distinguished:
Localization of prolapse: anterior, posterior or both leaflets. There are 3 degrees of prolapse: I degree – 3–6 mm. II degree – 6–9 mm. III degree – more than 9 mm.
Mitral regurgitation has 4 degrees: I degree - regurgitant flow is less than 4 cm² or penetrates into the cavity of the left atrium by more than 20 mm. II degree - regurgitant flow from 4 to 8 cm² or penetrates no more than half the length of the atrium. III degree - regurgitant flow more than 8 cm² or penetrates more than half the length of the atrium, but does not reach its “roof”. IV degree - the regurgitant flow reaches the posterior wall, extends beyond the left atrial appendage or into the pulmonary veins.
With mitral prolapse, complications may occur, which include: cardiac arrhythmias, infective endocarditis, heart failure, chord avulsion or perforation of the valve leaflet, sudden cardiac death, progressive mitral regurgitation with transformation into cerebrovascular accident.
Sources of development
The pathological condition is more often registered in women and is observed in almost 10% of patients. The primary form of the disease refers to congenital diseases and is combined with other genetic abnormalities in connective tissues:
- with a differentiated form of congenital connective tissue deficiency - Marfan's disease;
- imperfect desmogenesis - Chernogubov-Ehlers-Danlos syndrome;
- elastic pseudoxanthoma;
- osteogenesis imperfecta;
- polycystic kidney disease in adults.
The secondary form is formed as complications:
- impaired blood supply to the papillary muscles;
- rheumatic fever;
- Besnier–Beck–Schaumann disease;
- HCM with pathological thickening of the left ventricle.
In most patients, the disease is detected during a preventive examination - it occurs without severe symptoms.
Clinical symptoms
With mitral valve prolapse, the symptoms resemble those of VSD, especially at a young age. The main features are presented:
- feeling of insufficient air supply;
- chills, frequent or rare urination, as a response to psycho-emotional stress;
- cephalgia in the mornings and evenings, frequent mood swings;
- dizziness, short-term fainting.
Additional symptoms include palpitations and arrhythmias - the severity depends on the severity of the pathology. Patients may complain of discomfort on the left side of the chest, which is not associated with hard work, sports or psycho-emotional state.
Diagnostic examination
When visiting a local clinic, the patient is referred for a consultation with a cardiologist. The doctor reviews the medical history and asks questions about the patient's symptoms and general condition. During examination, a preliminary diagnosis is made based on indirect signs while listening to the heart.
When the ventricles contract, an extraneous sound may be observed, resembling a click and a slight noise that occurs when the blood flows back. A mild degree of damage does not show these symptoms.
Laboratory testing does not allow establishing a diagnosis; instrumental examination is considered the main one. During the test, the patient undergoes:
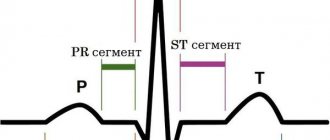
- ECG - mitral valve prolapse does not show specific changes. In some cases, blockade of conductive lines, extrasystoles, and signs of atrial fibrillation may be observed.
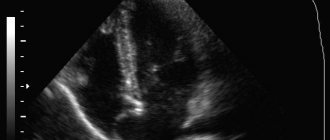
- Ultrasound of the heart muscle - echocardiography is considered an accurate technique that allows you to identify the presence of the disease, assess the degree of damage and valve dysfunction.
After confirming the presumptive diagnosis, the cardiologist begins to calculate a treatment regimen.
Diagnostics
If signs of cardiac dysfunction appear, you should consult a cardiologist. Patients with suspected MVP are prescribed:
- Ultrasound, which helps assess the degree of valve deflection;
- echocardiographic examination to assess heart function and rhythm changes during the day;
- x-ray to determine the size of the heart;
- bicycle ergometry to assess exercise tolerance.
MVP may be accompanied by other cardiovascular diseases. Complex diagnostics allows us to identify them and objectively evaluate each clinical case.
Features of treatment
Mitral valve prolapse does not have specific signs that make it possible to accurately determine the pathology. The symptoms are similar to many diseases, which does not give the right to independent therapy according to the textbook. Treatment should be carried out by a doctor, based on the data of a diagnostic examination.
Therapy is not carried out for prolapse that does not have signs of mitral valve insufficiency or with a normal ECG, without visible disturbances in the rhythm of heart contractions. The patient is monitored, with regular ultrasound examinations every year.
The patient is advised to reduce the amount or completely stop drinking alcoholic beverages, tea or coffee. The patient must quit smoking. As a preventative measure, a multivitamin complex with magnesium is prescribed. It has been scientifically proven that with this pathology the content of the element in the blood decreases.
Drug therapy for prolapse is irrelevant and is aimed at suppressing the present clinical symptoms. To treat the disease when there is a strong reflux of blood into the atrium, surgical intervention is used, with the installation of a prosthesis or plastic surgery of the affected valve.
Reasons for development
With this pathology, a small part of the blood returns to the atrium, that is, it does not enter the aorta. This condition is often asymptomatic and is usually diagnosed “accidentally” during a routine preventive examination or in connection with examinations for other problems of the cardiovascular system.
In the same way, the causes of prolapse of the anterior valve leaflet are not known for certain; some experts argue that the pathology is associated with hereditary diseases of the connective tissue - for example, it could be osteogenesis imperfecta or Marfan syndrome.