Tricuspid valve prolapse is a rare heart disease of organic origin. This defect is found in one person out of 10 thousand. Most often, it is diagnosed in males who have a history of coronary heart disease or coronary circulatory pathology.
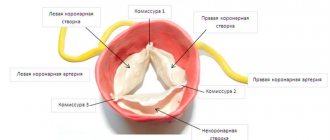
The tricuspid valve connects the right atrium and the right ventricle. Its function is to ensure the movement of blood towards the aorta and pulmonary artery and limit its flow back into the atrium.
The defect in the functioning of this heart valve is that it does not close completely or sag into the right atrium during diastole, which causes blood to flow in the opposite direction to normal blood flow (this process is called regurgitation). Pathological changes in the functioning of this valve are caused by processes of degeneration and dysplasia of its cells, so it loses its natural elasticity and seems to “fall in.”
Causes
The development of tricuspid valve prolapse is provoked by congenital or acquired factors.
- Disruption of normal intrauterine development, when the fetus can be affected by various toxic substances (with uncontrolled self-medication of the mother with pharmacological drugs, abuse of bad habits).
- Fetal hypoxia, insufficient oxygen supply.
- Toxicoses of a pregnant woman.
- Rhesus conflict between mother and fetus.
- Nutrient deficiency in a woman’s diet, fasting, strict diets.
- Genetic anomalies caused by the inheritance of defective chromosomes (Ehlers-Danlos syndrome, Marfan syndrome, congenital contractural arachnodactyly, elastic pseudoxanthoma).
- Rheumatism or rheumatoid arthritis.
- Cardiomyopathies.
- Pathologies of other heart valves (mitral and aortic).
- Complications after viral or bacterial diseases in early childhood (purulent tonsillitis, glomerulonephritis, pneumonia).
- Tumors in which the body produces a special substance that destroys myocytes (heart cells).
- Infectious heart diseases (myocarditis, pericarditis, endocarditis).
- Hyperthyroidism, thyrotoxicosis.
- Traumatic injuries to the chest (bruises, wounds, hematoma formation).
- Destruction of heart fibers due to the toxic effects of medications, drugs, ethyl alcohol.
- Bronchopulmonary diseases with impaired ventilation of organs.
- Cirrhosis of the liver.
- Autoimmune pathologies.
- Immunodeficiencies.
- Systemic diseases (scleroderma, lupus erythematosus, vasculitis).
- Hormonal or metabolic diseases.
- Arteritis.
- Exposure to ionizing radiation and poor ecology.
Publications in the media
Tricuspid regurgitation is the inability of the right atrioventricular valve to effectively prevent the backflow of blood from the right ventricle into the right atrium during ventricular systole.
Frequency • According to autopsies, tricuspid valve defects are found in 15–30% of patients with rheumatic heart disease • Tricuspid insufficiency makes up 85% of tricuspid valve defects • According to echocardiography, grade I tricuspid insufficiency can be detected in almost all healthy people.
Etiology • Primary tricuspid insufficiency with congenital anomalies (Ebstein anomalies, anomalies in the number of leaflets, in combination with an atrial septal defect or with corrected transposition of the main ones) - 50%, cardiac trauma, carcinoid syndrome (due to the formation of deforming fibrous plaques in the valve leaflets), myxomatous degeneration or rheumatic valve damage, endocarditis of drug addicts (isolated damage to the tricuspid valve - 40% of cases), connective tissue dysplasia syndromes (usually tricuspid valve prolapse with Marfan or Ehlers-Danlos syndrome) • Secondary tricuspid insufficiency due to dilatation of the fibrous ring with high pulmonary hypertension complicates 90% all mitral valve defects (of which 95% are mitral valve stenoses) and 90% of cases of dilated cardiomyopathy • Secondary tricuspid regurgitation due to ischemic dysfunction or rupture of papillary muscles during right ventricular infarction.
Pathophysiology • With primary failure, the load on the volume of the right parts of the heart increases, the size of their cavities increases, and blood stagnates in the systemic circulation • In some cases, with dilatation of the right atrium, thrombosis occurs, as well as supraventricular cardiac arrhythmias (Ebstein’s anomaly is often combined with Wolff’s syndrome -Parkinson-White) • The addition of secondary insufficiency in mitral defects complicated by high pulmonary hypertension is usually accompanied by unloading of the pulmonary circulation and some improvement in hemodynamics without significant stagnation in the systemic circulation and a decrease in stroke volume • As the defect progresses, cardiac output decreases more significantly • When the pressure in the right atrium increases by more than 10 mm Hg. stagnation develops in the systemic circulation • There are four degrees of defect: I - a barely detectable reverse flow of blood, II - a reverse flow is determined at a distance of 2 cm from the valve, III - a regurgitant stream is determined at a distance of more than 2 cm from the valve, IV - regurgitation is determined at a large extent of the cavity of the right atrium.
Clinical picture and diagnosis • Complaints •• In infants, severe heart failure and cyanosis are usually detected, at older ages - shortness of breath, increased fatigue, cyanosis and symptoms of right ventricular failure • In 25% of cases, the initial manifestation is supraventricular tachycardia as a manifestation of Wolff-Parkinson syndrome –White or atrial fibrillation during their dilatation • Complaints caused by concomitant conditions in secondary insufficiency (pain syndrome during right ventricular infarction, symptoms of mitral valve defects, etc.).
• Peripheral symptoms •• Pulsation of the jugular veins •• Pulsation along the left edge of the sternum, increasing with inspiration •• Palpable pulsation of the right atrium and pulmonary artery in ventricular systole •• Pulsation of the liver.
• Valve symptoms •• Systolic tremor •• Weakening of the 1st tone •• Strengthening of the pulmonary component of the 2nd tone •• 3rd tone •• Sounds of flapping sail with valve prolapse •• Pansystolic murmur (especially with increased afterload of the right ventricle) above the xiphoid process of the sternum, often musical or resembling a horn, the intensity of which increases with inspiration (Rivero-Corvalho sign) or with pressure on the liver •• In severe tricuspid regurgitation, a low-frequency protodiastolic or mesodiastolic murmur is sometimes heard.
• Symptoms of insufficiency in the systemic circulation •• Expansion of the size of the heart to the right •• Swelling of the neck veins •• Enlargement of the liver •• Plesch's symptom - swelling of the neck veins with slight compression of the liver during palpation •• Edema •• Ascites.
• Symptoms of the underlying disease (Marfan syndrome, infective endocarditis, MI, PE).
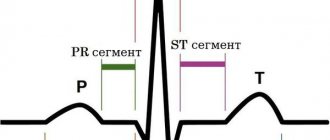
Special studies • ECG •• Signs of hypertrophy and overload of the right heart •• -Wave and paroxysms of tachycardia from the AV node in Wolff–Parkinson–White syndrome •• Atrial fibrillation and flutter •• AV block with Ebstein anomaly or cleft septal cusp valve • Jugular venogram : pronounced V waves, the height of which correlates with the severity of tricuspid regurgitation. • X-ray of the chest organs •• Bulging of the arches of the right ventricle and right atrium •• Expansion of the shadows of the vena cava •• In case of secondary insufficiency - strengthening of the pulmonary pattern, expansion and lack of structure of the roots of the lungs, Kerley B lines, bulging of the arches of the left parts of the heart and pulmonary artery.
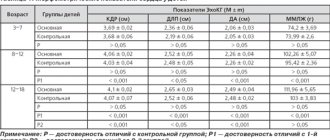
• EchoCG •• Increase in the size of the cavities and hypertrophy of the walls of the right heart •• Expansion of the superior vena cava •• Expansion of the diameter of the fibrous annulus of the valve with a secondary defect •• Deformation of the valvular apparatus in rheumatism •• Signs of other valvular or congenital anomalies •• Displacement of the fibrous annulus of the valve and “atrialization” of the right ventricle, as well as an increase in the amplitude of movement of the leaflets with Ebstein’s anomaly •• Thickening and deformation of the leaflets with carcinoid syndrome •• The presence of vegetations or leaflet defects with infective endocarditis •• Registration of the regurgitant flow in Doppler mode and determination of the severity of regurgitation in relation to the area jet to the area of the right atrium (I degree - the ratio does not exceed 1:3, II degree - 2:3, III degree - exceeds 2:3) •• Based on the maximum speed of the regurgitant jet (v), the systolic pressure in the pulmonary artery (SPAP) is calculated : SDPA = SDPV (in the absence of pulmonary stenosis); SDPV = 4v2 + CVP, where SDPV is the systolic pressure in the right ventricle •• Transesophageal echocardiography is performed in all patients to exclude right atrial thrombosis and vegetations, even with normal heart rhythm.
• Catheterization of the right heart •• On the pressure curve in the right atrium - a pronounced wave V and a steep Y-decline •• In severe failure - wave A and the X-decline are smoothed, so the pressure curve in the right atrium is similar to that in the right ventricle •• In case of isolated insufficiency - acceleration of AV blood flow during early diastolic filling •• The presence of a high end-diastolic AV pressure gradient indicates concomitant tricuspid valve stenosis •• Measurement of pressure in the right ventricle, right atrium and pulmonary artery at rest and against the background of tests with oxygen and aminophylline to determine the reversibility of pulmonary arterial hypertension and the prognosis of surgical treatment •• With an increase in systolic pressure in the right ventricle more than 60 mm Hg. Tricuspid insufficiency is almost always caused by mitral valve defects.
• Right ventriculography •• Registration of regurgitant flow •• Assessment of the topography of the right parts of the heart in Ebstein anomaly and exclusion of associated anomalies (transposition of the great vessels, ASD, etc.).
• Coronary angiography •• Performed in the presence of episodes of angina and positive results of stress testing, as well as in all women over 45 years of age, men over 40 years of age, and all candidates for multivalve reconstruction •• 14% of patients with tricuspid valve disease are diagnosed with CAD.
TREATMENT • Conservative treatment •• In the absence of pulmonary hypertension, even severe insufficiency can usually be treated with diuretics and venous vasodilators (nitrates orally and in the form of patches, for severe refractory tricuspid insufficiency - ACE inhibitors) •• The dose is selected depending on CVP, diuresis and the severity of edema •• The effectiveness of cardiac glycosides in sinus rhythm is low •• For refractory tricuspid regurgitation and severe right ventricular dysfunction, IV inotropes are indicated (preferably dobutamine) •• For pulmonary hypertension, the most beneficial effect is a decrease in pressure in the pulmonary artery: in some cases, diuretics are effective and vasodilators, but they should be used with caution because the range of acceptable values of cardiac filling is narrowed, and the ability to increase cardiac output in response to a decrease in peripheral vascular resistance is limited •• Prevention of infective endocarditis is recommended in all cases of primary tricuspid regurgitation, and in cases of secondary tricuspid regurgitation, the need for prophylaxis , apparently not •• With infective endocarditis, hemodynamic complications and embolism are better tolerated than with endocarditis of the left heart, so antibiotic therapy before surgery can be carried out longer (in some cases, it is possible to do without surgery at all).
• Surgical treatment •• Indications ••• III–IV degree of tricuspid insufficiency with pronounced clinical manifestations ••• Hemodynamically significant defects in combination with II or greater degree of relative tricuspid insufficiency ••• III–IV degree of asymptomatic defect with gross deformation of the leaflets or valve device •• Contraindications ••• Severe concomitant pathology that threatens the patient’s life ••• Terminal stage of circulatory failure ••• Negative results of tests with aminophylline and oxygen ••• The activity of the rheumatic process is not considered a contraindication to surgical treatment •• Methods of surgical treatment •• • The Kay-Boyd and DeVega suture methods or the support-ring Carpentier method of annuloplasty are used for primary defects and intact valve apparatus ••• In case of gross morphological changes in the valve, infective endocarditis, Ebstein’s anomaly and the ineffectiveness of previous annuloplasty, valve replacement is performed with biological artificial valves (30% operations on the tricuspid valve) ••• An ambiguous attitude towards mechanical valves in the tricuspid position is caused by increased thrombus formation in the right parts of the heart, apparently due to the low concentration of PgI2, which has an antithrombotic effect (this Pg is synthesized in the lungs and enters the bloodstream only in left side of the heart).
Specific complications • PE • Secondary infective endocarditis • Thrombosis of the prosthesis • Degenerative changes in the biological prosthesis and the need for re-prosthesis • AV block.
Prognosis • In the natural course of the defect, the prognosis is almost entirely determined by concomitant conditions, for example, the severity of damage to the mitral and aortic valves •• The addition of a secondary tricuspid defect worsens the prognosis •• With traumatic insufficiency, patients who survive the acute period usually tolerate the defect relatively easily for 5–10 years, after which rapid progression of symptoms occurs •• Among patients with moderate tricuspid regurgitation after surgical correction of concomitant severe mitral valve disease, 66% of patients subsequently require correction of progressive tricuspid regurgitation • Prognosis for surgical treatment •• Hospital mortality - 14.1%.
Synonyms • Right atrioventricular valve insufficiency • Tricuspid valve insufficiency. Abbreviations • PSPA - systolic pressure in the pulmonary artery • SDPV - systolic pressure in the right ventricle.
ICD-10 • I07.1 Tricuspid insufficiency
Degrees of tricuspid valve prolapse
- The first is the appearance of moderate regurgitation at the level of the leaflets, which can be detected by ultrasound. Patients have no health complaints and maintain an active lifestyle.
- The second is that the reverse flow of blood increases and reaches the middle of the right atrium. Patients begin to feel interruptions in the work of the heart, their health worsens.
- Third, regurgitation reaches large volumes and is observed throughout the atrium; patients present characteristic complaints of disturbances in the functioning of the heart (rhythm changes, increased pressure, dizziness, chest pain, shortness of breath on exertion or at rest).
- Fourth, up to 40% of the blood enters the right atrium in diastole. The condition of the patients is extremely serious, signs of heart failure are clearly expressed.
In medicine, primary prolapse of the TC (tricuspid valve) and secondary are also distinguished. The first option is easier and is most often caused by pathologies in the functioning of the heart and its vessels. The second is a consequence of pulmonary hypertension, which occurs due to serious pathologies of the lungs or pulmonary artery.
Types of disease
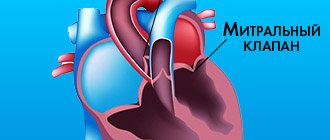
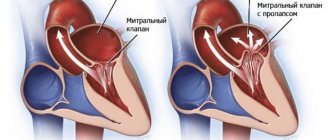
Experts distinguish primary and secondary forms of mitral valve prolapse; the lesion can affect the anterior, posterior or both leaflets. Three degrees of pathology are observed:
- the first - with sagging of the valves from 3 to 6 mm;
- the second – from 6 to 9 mm;
- the third is more than 9 mm.
The disease is divided according to the rate of blood return:
- first degree – in the area of the valves;
- the second - in the middle of the left atrium;
- the third is at the opposite end of the atrium.
The initial lesion includes grade 1 mitral valve prolapse.
Clinic
Symptoms of the disease increase in direct proportion to the increase in regurgitation.
At the initial stages, the defect can manifest itself by indirect signs:
- rapid fatigue when performing household or professional chores;
- migraine-like headaches;
- nausea combined with slight dizziness;
- sleep disturbances, excessive anxiety.
The following symptoms are characteristic of the height of the disease:
- severe fatigue, weakness even with little physical activity;
- excessive sweating, trembling in the limbs;
- severe swelling in the legs and abdomen;
- palpable and visible pulsation of the veins in the neck;
- decrease in the volume of urine excreted;
- heart rhythm disturbances (tachycardia, arrhythmia, extrasystoles);
- heart pain;
- severe shortness of breath;
- hemoptysis (sometimes);
- pain and discomfort in the right hypochondrium, significant enlargement of the liver;
- rises in blood pressure;
- dyspeptic symptoms: nausea, vomiting (not always);
- dizziness, fainting.
Objective diagnostic signs of the disease (detected by listening, beating the heart, on ultrasound images, x-rays).
- Enlargement of the cardiac borders on the right.
- Myocardial hypertrophy.
- Heart murmurs, especially when inhaling.
- Recording the degree of regurgitation and flexion of valve leaflets during ultrasound examination.
1.What is mitral valve regurgitation?
Mitral valve regurgitation
characterized by an unnatural flow of blood from the left ventricle into the left atrium during
systole
- contraction of the heart muscle.
When the heart valve is working properly, blood moves from the atrium to the ventricle. Against the background of rheumatic fever, dilation of the mitral valve ring, ischemic dysfunction of the papillary muscles and other unfavorable factors, the direction of blood flow changes in the opposite direction.
According to statistics, about 70% of the world's population is affected by mitral regurgitation. Minor manifestations of this pathological process can occur even in absolutely healthy people.
A must read! Help with treatment and hospitalization!
Treatment
Treatment of tricuspid valve prolapse is based on conservative or surgical measures. The choice of treatment method depends on the degree of damage and the course of the disease.
At the initial stages of the disease, doctors prescribe diuretics, ACE inhibitors, potassium supplements, vitamins, cardiac glycosides, and anticoagulants. The goal of therapy for stage 1 PTC is to stop the weakening of valve contractility and restore normal functioning of the heart muscle.
In the later stages of the disease, drug treatment is considered ineffective and patients are offered surgical intervention. It consists of reconstruction of the fibrinous ring of the affected valve or its prosthetics (complete replacement with an implant).
Unique operations performed by famous cardiac surgeons - only in Top Ikhilov
Among the main pathologies of the tricuspid valve are a narrowing of its diameter, or stenosis, insufficiency (the valves do not close tightly) and congenital defects (atresia - the ventricles are developed unequally, Ebstein's anomaly - displacement of the valves).
Treatment of tricuspid heart valve disease in Israel involves the use of medications and surgical intervention.
- Drug therapy . The Top Ichilov Medical Center uses modern drugs that are effective against pathology and safe for the body. In the treatment of tricuspid valve defects, angiotensin-converting enzyme (ACE) inhibitors, beta blockers, calcium channel blockers, glycosides, etc. are prescribed. The purpose of using medications is to lower blood pressure, improve blood circulation, reduce the frequency and strength of heart contractions, spasm of the coronary arteries and etc. Individual selection of drugs allows you to achieve maximum effect and reduce the development of side effects.
- Surgical intervention . Cardiac surgeons at Top Ikhilov in most cases prefer low-traumatic operations performed on the beating heart. Annuloplasty is an operation to strengthen the base of the valve and fix the valve flaps in the desired position by applying a ring or sutures. Thanks to annuloplasty, complete closure of the valves and normalization of blood circulation are achieved. When correcting the leaflets, the cardiac surgeon separates the fused leaflets, restores their shape, and stitches the tears. That is, defects in their structure are corrected. Valve replacement with an artificial prosthesis is performed using a transcatheter approach. Biological or mechanical implants (made of composite materials) are used, which are safe, hypoallergenic, and take root well. Percutaneous balloon valvuloplasty is used to increase the lumen of stenosis using a balloon, which is brought to the site of stenosis and inflated primarily with fluid to avoid embolism, thereby increasing the lumen of the valve. After achieving normal values, the liquid from the balloon is released and the balloon is removed along with the catheter.
Prevention and prognosis
- Normalization of the daily routine, rational distribution of loads, adequate sleep.
- Timely treatment of infectious and degenerative diseases of the body.
- Proper nutrition.
- Rejection of bad habits.
- Active lifestyle.
- Pregnant women need to treat gestosis, as well as eliminate harmful effects on the fetus.
Is tricuspid valve prolapse dangerous? Minor TC prolapse has a favorable prognosis. Such patients are monitored by cardiologists and are prescribed diagnostic examinations once a year. Women with this defect can become pregnant and give birth to a healthy child. Of course, subject to constant monitoring at the cardiology center.
If the disease progresses, it is important to promptly perform surgical intervention and restore the functions of the tricuspid valve.
Romanovskaya Tatyana Vladimirovna
Diagnostics
The main diagnostic method is conventional auscultation of the heart (listening). When prolapse occurs, the doctor hears specific noises and clicks.
An ECG is not advisable because it does not show any abnormalities. The key test is echocardiography. If necessary, angiocardiography, left-sided ventriculography, and radionuclide testing are additionally performed.
Differential diagnosis is carried out with aneurysm of the interatrial septum, mitral valve insufficiency, acquired heart defects.
Symptoms
These include the so-called stigmas - signs of imperfection of the connective tissue framework: joint hypermobility, winged shoulder blades, myopia, Gothic (high) palate, malocclusion, flat feet, tall stature and asthenic physique, scoliosis, hernias, varicose veins. There is also a violation of the architectonics of the atrioventricular ring with displacement of the valves and additional chords in the valve apparatus.
Later, by the age of 7, additional symptoms appear: short-term stabbing pains in the heart area of a psycho-emotional nature, and not due to damage to the heart muscle, attacks of rapid heartbeat, interruptions.
Symptoms of vascular dystonia include dizziness, cephalgia in the morning, worsening after overwork, decreased performance and increased fatigue. Children are tearful, often have fears, depression, irritability, and poor sleep. In fact, this is a mass of microanomalies combined with vegetative-vascular instability.
A pediatrician or cardiologist listens to the murmur over the heart area and determines its nature - late systolic or in the form of a systolic click.