Neck veins, swelling
To assess the filling of the external jugular veins, the patient should be placed on his back, with the torso bent at an angle of 45°. Normally, the veins in this position look sunken or fill to a level of no more than 1–2 cm above the manubrium of the sternum, and the filling of the veins during inhalation is less than during exhalation.
Pathomechanism and causes
Vein swelling is a consequence of increased venous pressure. If, in a standing position, the filling of the jugular veins reaches the angle of the mandible, then the venous pressure is ≥25 cmH2O. The causes of swelling of the jugular veins are as follows:
1) bilateral - right ventricular heart failure, a large amount of fluid in the heart sac (including cardiac tamponade), constrictive pericarditis (in this case, swelling increases during inspiration - unusual [paradoxical] venous pulse [symptom] of Kussmaul [sometimes observed with severe right ventricular failure]), impaired patency of the superior vena cava (superior vena cava syndrome (320; causes - lung tumor and enlarged lymph nodes of the upper mediastinum, less often - thrombophlebitis of the superior vena cava, mediastinal fibrosis, thoracic aortic aneurysm, very large goiter), stenosis or tricuspid valve insufficiency (with insufficiency, a positive venous pulse is observed - filling increases during cardiac systole), pulmonary hypertension, pulmonary embolism, tension pneumothorax;
2) unilateral - large goiter; on the left - compression of the left brachiocephalic vein by an aortic aneurysm.
Diagnostics
1. Assess vital signs (respirations, pulse, blood pressure), as there may be an immediate threat to life (especially in the case of cardiac tamponade, tension pneumothorax, or pulmonary embolism).
2. It is necessary to collect anamnesis and conduct an objective examination. Examine the hepatojugular drainage to locate the obstruction that is causing the jugular veins to distend. Place the patient on his back. In this case, his torso should be in such a position that the jugular veins do not fill more than 1–2 cm above the level of the jugular notch of the sternum. For 30–60 s, apply pressure to the area of the right hypochondrium with your hand, and if there is increased sensitivity in this place, to another area of the abdominal cavity; Make sure that the patient is breathing freely and observe the jugular veins. Their bulging above the level of the sternocleidomastoid muscle (positive hepatojugular reflux) is characteristic of congestive heart failure (compression of the liver area increases pressure in the inferior vena cava and right atrium, which is transmitted to the superior vena cava and jugular veins). In healthy individuals or in cases where circulatory impairment is present above the right atrium, compression of the liver does not cause a significant increase in atrial pressure or transmission of increased pressure from the right atrium to the superior vena cava is impossible. Holding your breath during the study of the hepatojugular outflow creates an effect similar to the Valsalva maneuver and swelling of the jugular veins in this case has no diagnostic value.
3. Additional research methods: X-ray of the chest; if heart failure, cardiac tamponade, pericarditis or valvular defects are suspected - echocardiography; for large goiters - ultrasound of the neck plus a study of TSH and thyroid hormones; for superior vena cava syndrome (it is accompanied by swelling of the face and neck, as well as dilatation of the veins of the upper half of the chest) - CT scan of the chest, if lung cancer is suspected - bronchoscopy; if pulmonary embolism is suspected, angio-CT of the chest, possibly ultrasound of the veins of the lower extremities.
Paragangliomas are true neoplasms, the source of growth of which is paraganglionic chemoreceptor cells. In the temporal bone, these cells are located in the region of the jugular vein bulb and on the promontorial wall of the tympanic cavity, originating from the branch of the glossopharyngeal nerve - the tympanic nerve [1].
The prevalence of this pathology is 1:1,300,000, however, among benign tumors of the middle ear, glomus tumors occupy 2nd place after neuroma of the vestibular-cochlear nerve [1-3].
Glomus tumors are characterized by tissue atypia, that is, they are benign, and relatively slow growth, but their localization causes significant medical problems, such as serious pathological manifestations when tumors are localized at the base of the skull in the area of the internal carotid artery, as well as the cranial nerves that provide including coordination, swallowing, vocal production, and difficult surgical access [1–3]. The mortality rate of patients due to local progression of glomus tumor is 6% [4].
Surgical removal is the gold standard treatment for paragangliomas. This treatment method is especially relevant in the early stages of the tumor process, when it is possible not only to completely remove the tumor, but also to improve the patient’s quality of life by restoring hearing. Another treatment option for glomus tumors is radiation therapy (gamma knife). The above method is used when the patient refuses surgery, there is a concomitant somatic pathology that is a contraindication to prolonged surgery under anesthesia, as well as when it is impossible to surgically remove the tumor (growth into the internal carotid artery). If it is not possible to completely remove the tumor, a combination of surgery and radiation methods is possible to slow down its growth. If there are contraindications to surgery, only radiation therapy is performed [2, 5, 6].
In the case when the glomus tumor is closely adjacent to certain cranial nerves, its removal may lead to their damage, with the development of the corresponding clinical picture [7, 8]. For example, according to the literature, worsening of existing clinical manifestations (dysphagia and/or hoarseness) or their appearance was noted in 33% of cases after removal of the jugular glomus [9]. Other complications of surgical treatment are hearing loss/deafness (19%) [9], liquorrhea (8.3%), aspiration (5.5%), infection of the postoperative area (5.5%), pneumonia (2.3%) , meningitis (2.1%) [10].
We present a clinical observation.
Patient G.
, 29 years old, entered the otolaryngological department of Clinical Hospital No. 1 of the Federal State Autonomous Institution V.O. First Moscow State Medical University named after. THEM. Sechenov Ministry of Health of Russia (Sechenov University) with complaints of constant noise in the left ear, pulsating in nature, coinciding with the rhythm of the heartbeat, decreased hearing in this ear, nagging pain in the left temporal region.
The above complaints bothered the patient for 2 years, the symptoms increased over time. At the place of residence, after repeated ineffective courses of antibacterial therapy, a CT scan of the temporal bones and an MRI of the brain were performed, where a neoplasm of the temporal bone was detected on the left.
Otoscopy of AS revealed a typical picture of a glomus tumor: in the lower parts, the membrane was bulging due to a bright red pulsating neoplasm located behind it. The results of the audiological examination are presented in Fig. 1.
Rice. 1. Data from audiological examination.
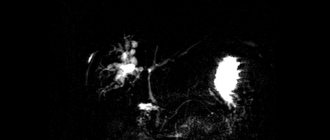
According to contrast-enhanced MRI, in the projection of the apex of the temporal bone pyramid extending to the area of the bulb of the left jugular vein, an inhomogeneous structure of irregularly rounded shape, measuring about 15x17x21 mm, intimately adjacent to the left internal carotid artery, as well as to the dura mater, was determined membrane of the posterior cranial fossa. The tumor actively accumulated contrast agent (Fig. 2).
Rice. 2. MRI of the skull base. In the area of the apex of the temporal bone pyramid on the left there is a glomus tumor (indicated by an arrow), adjacent to the internal carotid artery.
Based on the results of the examination, the tactics for managing the patient were determined - surgical treatment with preliminary selective embolization of the vessels feeding the tumor. During the operation, after performing a mastoidectomy, exposing the facial nerve along the tympanal and mastoid parts and transposing it anteriorly, the tumor was removed along with the jugular vein bulb and the sigmoid sinus. The tumor occupied the area of the jugular vein bulb, spread into the posterior cranial fossa, into the area of the internal carotid artery, as well as the neurovascular bundle of the jugular notch. Intact n. have been identified. vagus, n. hypoglossus, n. glossopharyngeus. A small defect in the dura mater is closed with fascia, the resulting cavity is obliterated with adipose tissue taken from the anterior abdominal wall, and the external auditory canal is sutured tightly. After the operation and recovery from anesthesia, the patient was transferred to the intensive care unit, where she was planned to be extubated after 6 hours due to a long surgical procedure. On the first day after surgery, liquorrhea was noted, which required the installation of a lumbar drainage. Antibacterial therapy was carried out (ceftriaxone 2 g 2 times a day). After 7 days, the liquorrhea was relieved and the patient was transferred to the otorhinolaryngology department.
After extubation, the patient noted difficulty swallowing, choking, wheezing during inspiration, and lack of voice. When performing fiberoscopy, bilateral laryngeal paresis was revealed, the fixed vocal folds were in the paramedian position, the lumen of the glottis was 4-5 mm (Fig. 3).
Rice. 3. Video laryngoscopy data on the 1st day after surgery. Phonation. The vocal folds are in a paramedian position. In the postoperative period, laryngeal paresis was treated, which included injections of proserin, milgamma, and glucocorticosteroid therapy. On the 8th day after surgery, reflexology, acupuncture, and novocaine blockade of the Zakharyin-Ged zones were additionally prescribed. There were no local postoperative complications noted.
On the 11th day after surgery, against the background of the treatment, positive dynamics in the larynx were noted. During stroboscopy, microoscillations of the vocal folds were recorded, movements of the arytenoid folds appeared, and an expansion of the glottis to 6-7 mm was noted.
However, on the 12th day the patient developed a dry cough and general weakness. Based on clinical data and chest CT results, the pulmonologist diagnosed bilateral polysegmental (aspiration) pneumonia of moderate severity. Antibacterial therapy was prescribed - Avelox 400 mg per day for 10 days, then Thiene 500 mg intravenously for 10 days. The patient was under dynamic supervision of an otorhinolaryngologist, pulmonologist, and clinical pharmacologist; treatment was adjusted according to bacteriological and clinical data. After 18 days, a control CT scan of the chest organs was performed, and resolution of the pneumonia was noted. During control stroboscopy on the 18th day, limited movements of the right half of the larynx and micro-oscillations of the left vocal fold were visualized. The clearance of the glottis in the posterior third was 6-7 mm.
After 6 months, the mobility of the right half of the larynx was restored, the left vocal fold remained motionless. The patient still has slight hoarseness, which does not cause concern to the patient.
This clinical case demonstrates the difficulties of postoperative management of patients after removal of a glomus tumor of the jugular vein. Despite a certain risk of complications, surgical treatment in this case was chosen due to the rather large size of the tumor, its proximity to the cranial nerves, and the young age of the patient. Further growth of the tumor would lead to neurological deficits.
The peculiarity of this clinical case is that in the postoperative period, the patient, not excluding the traumatic etiology of paresis on the left, developed idiopathic paresis of the right half of the larynx, which in turn led to such a serious complication as aspiration pneumonia.
The authors declare no conflict of interest.
*e-mail; https://orcid.org/0000-0001-7414-1293
Venous malformation (venous angioma).
It occurs relatively frequently and is not a true malformation; it is more a variant of the structure of the venous outflow.
The course is usually asymptomatic. Convulsions rarely occur.
Venous malformation. Scheme. Small dilated venules in the form of an “umbrella”, “jellyfish head” are identified, draining into a large transcortical vein, which, in turn, flows into the superior sagittal sinus.
a) T1 with intravenous contrast. Arrows indicate dilated deep white matter veins draining into the dilated transcortical vein; b) Contrast-enhanced MR venography shows venous dysplasia draining into a dilated internal cerebral vein. Venous malformation.
Combination of glomus tumor of the jugular vein bulb with epitympanitis complicated by cholesteatoma
For citation.
Shevchik E.A., Svistushkin V.M., Mukhamedov I.T., Pshonkina D.M., Zolotova A.V. Combination of glomus tumor of the jugular vein bulb with epitympanitis complicated by cholesteatoma // RMJ. 2015. No. 23. pp. 1420–1421. Summary
: The article presents a clinical case of a combination of a glomus tumor of the jugular vein with chronic purulent otitis media, complicated by cholesteatoma. A classification of glomus neoplasms of the temporal bone is given. Particular attention is paid to the difficulty of timely diagnosis of glomus neoplasms of this localization.
Keywords
: glomus tumor, jugular glomus, cholesteatoma.
Glomus tumor is a benign, slow-growing, highly vascularized, locally invasive neoplasm that develops from paraganglion cells associated with the sympathetic and parasympathetic ganglia.
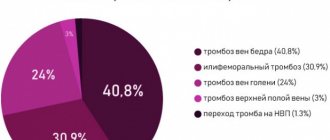
Thus, glomus tumors can be classified as paragangliomas. In the area of the temporal bone, glomus tumors are most often localized in the region of the jugular vein bulb, as well as on the promontorial wall, based on the tympanic plexus. Despite the low prevalence of this pathology (1:300,000), among benign tumors of the middle ear, glomus tumors occupy 2nd place after neuroma of the vestibulocochlear nerve [1–3]. Due to slow growth and asymptomatic course, clinical manifestations manifest at the age of 40–60 years, while in women the incidence of this pathology is 3 times higher than in men. There is a genetic predisposition to this disease. If this pathology is present in close relatives, the risk of developing a neoplasm is 30%. Currently, a number of genes have been identified whose mutations lead to an increased risk of developing paragangliomas [2–4]. Glomus tumors are locally invasive, and therefore the classification of this pathology is based on the degree of invasion of the tumor into surrounding structures. In type A, the paraganglioma is located within the tympanic cavity; type B involves invasion of the neoplasm into the cells of the mastoid process. In type C, the tumor affects the infralabyrinthine space and spreads to the apex of the temporal bone. In this case, the most important is the relationship of the neoplasm with the wall of the internal carotid artery. In type D, intracranial distribution is noted [5]. The method of choice in the treatment of this pathology is surgical removal of the tumor. An alternative method is radiation therapy (g-knife), which is indicated for elderly people and patients who have contraindications for major surgery; according to the literature, it can slow down or even stop the growth of a glomus tumor [6]. Clinical part
Patient T., 55 years old, was admitted to the clinic of ear, nose and throat diseases of the First Moscow State Medical University named after I.M. Sechenov on September 8, 2015, with complaints of an almost complete lack of hearing in the left ear, a constant hissing noise in this ear of a pulsating nature with a changing timbre, intensifying during physical activity, periodic suppuration from the left ear. The patient noticed a noise in the left ear about 6 years ago, but did not consult a doctor; after 3 years, the hearing in this ear began to decrease, suppuration periodically appeared, which forced the patient to consult an ENT doctor at the clinic at his place of residence. Due to suppuration and absence of pain, a diagnosis of “Left-sided chronic suppurative otitis media” was made, and conservative treatment and observation were carried out. It should be noted that at this stage the patient was not recommended to perform a CT scan of the temporal bones and surgical treatment. Observation was carried out for 5 years, despite periodic suppuration from the left ear. A year ago, the patient independently noted the appearance of a tumor in the external auditory canal while performing an ear toilet, and again consulted a doctor. Only at this stage was additional examination performed including CT and MRI of the temporal bones. According to the results of radiological diagnostics, a CT scan of the temporal bones (dated December 15, 2014) revealed signs of a neoplasm of the left temporal bone with osteolytic destruction (Fig. 1); Based on the results of an MRI of cerebral vessels dated April 10, 2015, MRI signs of a pathological site of a vascular neoplasm in the area of the pyramid of the left temporal bone were revealed, most likely a glomus tumor of the bulb of the left jugular vein.
At the local clinic, a biopsy of the external auditory canal tumor was performed; the result of histological examination was angiofibroma. The patient was referred to the clinic of ear, nose and throat diseases of the First Moscow State Medical University named after I.M. Sechenov. Upon admission, otomicroscopy was performed: a subtotal defect of the tympanic membrane was noted on the left, the tympanic cavity was filled with a bright pink, pulsating formation. Audiologically: left-sided mixed hearing loss. A repeat MRI of the brain with contrast was performed on September 4, 2015: the MRI picture most likely corresponds to a glomus tumor on the left. No MRI data were obtained for focal lesions of the brain substance and cerebellum. The patient was consulted by a neurologist and a neurosurgeon to exclude damage to the cranial nerves; however, there were no signs of damage to the vagus, facial, accessory, or hypoglossal nerves, which can occur with a glomus tumor of this localization. The decision was made to undergo surgery. Taking into account the genesis of the formation, preliminary 09.09.2015 in the X-ray diagnostic angiography department of the First Moscow State Medical University named after I.M. Sechenov, under local anesthesia, arteriography of the left external carotid artery was performed in 2 projections with selective embolization of the glomus tumor. The blood supply to the formation was provided by the occipital and branches of the maxillary arteries.
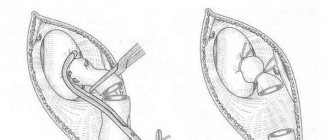
On May 10, 2015, under endotracheal anesthesia in the otorhinolaryngology department, a glomus tumor of the left middle ear was removed with the postoperative cavity being closed with fatty tissue from the anterior abdominal wall. During the intervention, it was noted that the formation filled all the cavities of the middle ear, enveloping the auditory ossicles; also a feature of this case was that inclusions of cholesteatoma were found in the epitympanum in the masses of the formation, which, as a rule, is not a concomitant pathology for glomus tumors (Fig. .2). A mastoidectomy was performed (all cells of the mastoid process were opened, exposing the sigmoid sinus, emissary, and dura mater of the middle cranial fossa), and the apex of the mastoid process was removed. The formation also extended into the retrofacial cells. Highlighted n. facialis from the geniculate ganglion to the stylomastoid foramen, its transposition anteriorly. The formation also spread to the area of the internal carotid artery. On the lateral surface of the neck, the jugular vein was identified up to the bulbus jugularis, from where the growth of the neoplasm originated. The sigmoid sinus is ligated and dissected. The tumor was removed along with part of the jugular vein, including the bulbus jugularis, and part of the sigmoid sinus. The cavity formed during the operation was filled with adipose tissue taken from the anterior abdominal wall (Fig. 3). In the postoperative period, active drainage was installed in the area of the bed of the neurovascular bundle on the 1st day, antibacterial, desensitizing, hormonal therapy, and local treatment (treatment and toilet of postoperative sutures) were carried out. During the treatment, the patient noted the absence of noise in the ear in the early postoperative period. Dizziness and spontaneous vestibular symptoms were also not noted. There was paresis of n. facialis grade III on the House-Brackman scale, resulting from transposition of the facial nerve. According to the results of a histological examination of intraoperative biopsy material: the morphological picture is characteristic of a paraganglioma (syn.: glomus tumor, chemodectoma) of the middle ear. The patient was discharged in satisfactory condition. In the postoperative period, positive dynamics were observed in terms of paresis of the facial nerve, which indicates a gradual restoration of its function. This clinical case is interesting due to the combination of two pathologies: a glomus tumor arising from the jugular vein bulb and chronic purulent otitis media complicated by cholesteatoma. In such a situation, symptoms such as suppuration and hearing loss can mask the clinical manifestations of a glomus tumor for a long time. It is worth noting that outpatient doctors often continue to observe patients diagnosed with “Chronic suppurative otitis media” in the presence of a glomus tumor of the middle ear, even in the absence of an inflammatory process. In such a situation, I would like to emphasize the importance of CT examination of the temporal bones, which must be performed on patients to clarify the degree of bone destruction and prepare for surgical intervention. CT results allow early suspicion of the presence of a glomus tumor. The doctor must conduct the necessary additional examination and refer the patient for surgical treatment, which will help avoid complications and reduce the volume of surgical intervention.