Introduction
Approximately 1–2% of the adult population in developed countries have heart failure (HF), and in patients over the age of 70 years, the risk of developing HF is more than 10% [1–4]. Among people over 65 years of age with new-onset dyspnea on exertion, 1 in 6 people will have unrecognized HF, mostly HF with preserved ejection fraction (EF) [3, 4]. The risk of developing heart failure at age 55 years is 33% for men and 28% for women [5].
Over the past 25 years, since enalapril has been shown to reduce mortality in patients with HF with reduced EF while taking enalapril, inhibitors of the renin-angiotensin-aldosterone system (RAAS) have been the mainstay of treatment for HF. Subsequent studies found that triple neurohormonal blockade: angiotensin-converting enzyme inhibitors (ACEIs), beta-blockers and mineralocorticoid receptor antagonists reduced the risk of death from 30-35 to 22-30%.
In 2021, a new drug appeared in the arsenal of cardiologists - sacubitril/valsartan (Uperio), which is a complex of neprilysin inhibitor and angiotensin-2 receptor blocker. Neprilysin is a membrane enzyme involved in the degradation mainly of natriuretic peptides [1–3]. Inhibition of neprilysin, in turn, causes an increase in the level of these peptides, which counteracts maladaptive neurohormonal activation, which contributes to sodium and water retention in the body, maintaining vasoconstriction and tissue remodeling [6, 7]. Simultaneous inhibition of the RAAS and neprilysin allows one to achieve an optimal level of neurohormonal balance, stabilize and improve the clinical condition of patients with HF with systolic dysfunction, as was demonstrated in the prospective randomized clinical trial PARADIGM-HF.
According to modern recommendations for the diagnosis, prevention and treatment of HF, sacubitril/valsartan is recommended for patients with chronic HF (CHF) functional class II-III with systolic dysfunction, who do not require intravenous or doubling the dose of oral diuretics, and with systolic blood pressure (BP) more than 100 mmHg, if ACE inhibitors or angiotensin receptor antagonists are tolerated, to further reduce the risk of death and subsequent hospitalizations due to worsening CHF (class of recommendation I, level of evidence B) [8].
How to replace Lozap with high blood pressure
On the pharmaceutical market, analogues of Lozap tablets for blood pressure are presented in a wide range. Experts note that the price of a substitute does not determine its quality. Cheap analogues can be no less effective than the original. It is important to carefully study the composition and instructions for use of the drug before purchasing it and starting the therapeutic course!
Lozap Plus
The latest generation analogue of Lozap is the drug Lozap Plus, which includes not only losartan, but also hydrochlorothiazide. This substance activates the main ingredient, perfectly complements and enhances it, and also helps to increase the duration of action of the tablets.
The dosage regimen is completely identical to the rules for using the drug Lozap, as well as the clinical indications. Possible side effects include allergic reactions.
The cost of Lozap Plus tablets is about 900-1000 rubles.
Lozap Plus tablets are supplemented with another active substance
Amlodipine
The drug Amlodipine is a substitute for Lozapa, which has earned numerous positive reviews from patients and medical specialists. The main active ingredient is amlodipine.
Tablets are prescribed for pain localized in the chest area and elevated blood pressure.
In addition to the contraindications inherent in Lozap, the substitute Amlodipine is not recommended for use in patients suffering from hypotension (low blood pressure), aortic stenosis, left ventricular failure, or collapse. Unlike Lozap, Amlodipine affects the central nervous system and the speed of reactions.
Used in a daily dose of 5 mg. To increase the effectiveness of the therapeutic course, it is recommended to combine taking pills with a salt-free diet.
If the drug is abruptly discontinued, there is a risk of developing angina. The estimated cost of Amlodipine tablets (30 pieces) is about 100 rubles.
Concor
A modern substitute for the high blood pressure drug Lozap is Concor, the main active ingredient of which is bisoprolol.
The tablets have a wider range of indications and are successfully used to treat not only high blood pressure, but also coronary artery disease and a chronic form of heart failure.
However, Concor has more contraindications. It is not recommended to use this substitute for the treatment of patients with psoriasis, respiratory tract pathologies, or weakened sinus nodes.
Tablets are taken 5 mg or 10 mg 1 time per day. If taking Lozap is in no way connected with your meal schedule, then Concor is recommended to be taken in the morning during breakfast.
The price of the analogue is about 220 rubles or more, depending on the dosage and number of tablets in the package.
Concor is an analogue of Lozap in terms of therapeutic action
Lorista
A complete analogue of the drug Lozap, which has an identical active substance, is the drug Lorista. In addition to the ability to lower blood pressure, the substitute is also characterized by the presence of moderate diuretic properties.
The average cost of the drug (30 tablets) is about 200 rubles.
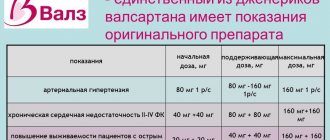
Valsartan
The drug Valsartan is a domestically produced analogue of Lozap. Used to lower blood pressure and treat heart failure. Contraindications are identical to the restrictions on use characteristic of Lozap.
Take tablets once a day in a dosage ranging from 80 mg to 230 mg.
The Russian substitute Lozapa is quite affordable and affordable - from 150 rubles for 30 tablets.
Clinical case
Patient B.
, 62 years old, was hospitalized from 08/29/18 to 09/09/18. She was admitted through emergency medical care with decompensated CHF. Upon admission, she complained of shortness of breath at rest, a feeling of lack of air, severe swelling of the lower extremities, general weakness, and pain in the lower extremities.
From the anamnesis it is known that the patient has been suffering from hypertension for a long time with maximum blood pressure values of 200/110 mm Hg, the usual blood pressure figures are 120-130/90 mm Hg. On an outpatient basis I took daily: bisoprolol 5 mg, losartan 50 mg, furosemide 20 mg, clopidogrel 75 mg, aspirin 100 mg. The patient had a history of myocardial infarction (of unknown duration) and a long-term persistent form of atrial fibrillation. I have type 2 diabetes mellitus, insulin dependent. Denies any history of cerebrovascular accident. About 2 years ago, atherosclerosis of peripheral arteries and occlusion of the arteries of the lower extremities were detected. She was repeatedly hospitalized due to S.N.’s decompensation. The condition worsened over the course of a week, when the above complaints began to increase.
The condition at admission was of moderate severity. The patient is conscious, the position is forced - orthopnea. The physique is normosthenic, body weight 60 kg, height 155 cm, BMI 25 kg/m2. The skin and mucous membranes are pale in color and clean. Symmetrical pronounced dense swelling of the legs and feet. The right lower limb is cold to the touch. Trophic ulcers of the right leg. In the lungs, breathing is harsh, fine wheezing on both sides, breathing is not audible in the lower sections. Heart sounds are muffled, irregular, there is no noise. Heart rate (HR) 117 beats/min, blood pressure 120/78 mm Hg. The abdomen is not enlarged, soft, painless. Stool and diuresis are not disturbed.
Data from clinical tests upon admission: hemoglobin 100 g/l, leukocytes 11.5·109/l; ESR 40 mm/h, neutrophils 9.4%. General urine test - without significant pathology, biochemical blood test: creatinine 203.66 mmol/l, urea 17.8, glucose 11.5 mmol/l, AST 33 U/l, ALT 60 U/l, potassium 5.6 mmol /l, sodium 137 mmol/l, natriuretic peptide BNP 3568 pg/ml, cholesterol 3.5 mmol/l. LDL 2.1 mmol/l, HDL 0.56 mmol/l.
Instrumental research data: electrocardiography (ECG) dated 08/29/18 - atrial fibrillation rhythm, heart rate 117 beats/min. The electrical axis of the heart is deviated to the left.
On the chest x-ray dated 08/30/18: bilateral hydrothorax.
Echocardiographic examination of the heart (EchoCG) dated 08/30/18
— aorta: sinus of Valsalva 3.5 cm. Left atrium 4.5×5.0×5.5 cm (4.0×4.0×6.0 cm), interventricular septum 1.0 cm (0.7— 1.1 cm); posterior wall of the left ventricle 0.9 cm (0.7-1.1 cm), end-systolic size 4.4 cm (2.5-4.1 cm), end-diastolic size 5.5 cm (3.5-5 .6 cm). The contractility of the left ventricular (LV) myocardium is diffusely reduced. Pronounced hypokinesia of the septum, anterior wall, akinesia of the apex. LVEF 40%, right atrium 5.0×5.0 cm (4.4×6.0 cm), right ventricle 2.5×4.0 cm (3.0×4.3 cm), additional formations: parietal thrombus 3.0×1.5 cm in the apex of the left vein. Contractility of the right ventricle is not impaired. The aortic valve is tricuspid, the leaflets are thickened, the leaflets are fully opened, the maximum pressure gradient is 3 mm Hg, degree I regurgitation. Mitral valve - multidirectional movement, regurgitation of the second degree. The tricuspid valve is not changed, regurgitation of II-III degree. The average pressure in the pulmonary artery is 50 mm Hg. There is 1.0 cm of fluid in the pericardial cavity. Bilateral hydrothorax.
Clinical diagnosis made:
Basic:
IHD. Post-infarction cardiosclerosis. Atherosclerosis of the aorta and coronary arteries. Atherosclerosis of the arteries of the lower extremities. Chronic arterial insufficiency of the 4th degree according to Fontaine-Pokrovsky. Occlusion of the tibial arteries on the right. Trophic ulcers of the right leg, I, II toes of the right foot. Forming gangrene of the right leg and foot.
Background disease:
stage III hypertension, stage 3 arterial hypertension, the risk of cardiovascular complications is very high.
Complication:
NK 2B, 3rd functional class according to NYHA. Chronic kidney disease - C4 (glomerular filtration rate - GFR - according to CKD-EPI 22 ml/min). Bilateral hydrothorax. Hydropericardium. Permanent form of atrial fibrillation. The risk of thromboembolic complications according to the CHADS2VASC scale is 6 points. The risk of bleeding on the HASBLED scale is 3 points.
Related:
diabetes mellitus type 2, insulin-requiring. Duodenal ulcer, without exacerbation. Chronic mixed gastritis.
Treatment in hospital: due to the presence of tachyform atrial fibrillation, the dose of bisoprolol was increased to 7.5 mg/day; For the first few days, intravenous furosemide was prescribed at a dose of 40 mg/day, followed by a transition to oral torsemide 10 mg/day. There was no significant decrease in creatinine levels after the administration of intravenous furosemide; creatinine clearance according to CKD-EPI was 24 ml/min (creatinine from 08/01/19 - 190 mlmol/l). After transferring the patient to an oral diuretic, it became possible to prescribe the drug sacubitril/valsartan (Uperio) 100 mg/day. Antiplatelet therapy was carried out with rivaroxaban 15 mg/day and clopidogrel 75 mg/day. The patient also received omeprazole 40 mg/day for gastroprotection and amoxiclav 3 g/day due to the presence of trophic ulcers.
After 7 days of therapy
Complaints of general weakness persist, shortness of breath at rest does not bother him, pain in the legs, mainly at night.
Objective status:
the condition is relatively satisfactory. The patient is conscious and moves around within the ward. The skin and mucous membranes are pale in color and clean. Edema of the lower extremities has regressed, some pastiness remains. Breathing in the lungs is harsh, somewhat weakened in the lower sections. Heart sounds are muffled, irregular, there is no noise. Heart rate 80 beats/min. Blood pressure 110/70 mm Hg. The abdomen is not enlarged, soft, painless. Stool and diuresis are not disturbed.
Laboratory tests indicate a decrease in creatinine to 120 mmol/l, urea 15.0, natriuretic peptide BNP 2000.2 pg/ml, glucose 10 mmol/l, potassium 4.9 mmol/l, ALT 9 mmol/l, AST 25 mmol/l.
Instrumental studies: ECG dated 09/05/18 - atrial fibrillation, heart rate 80 beats/min. On a repeat X-ray of the chest organs dated 09/07/18: positive dynamics of stagnant changes. Positive dynamics on EchoCG: improvement in LV myocardial contractility, increase in EF up to 50%, decrease in pressure in the pulmonary artery, resolution of hydropericardium and hydrothorax on the left.
Due to the stabilization of the patient’s condition and a decrease in creatinine levels during treatment, it became possible to conduct angiography of the vessels of the lower extremities. The patient was transferred to the surgery department, where recanalization, balloon angioplasty and stenting of the right superficial femoral artery were performed, Abbott SUPERA 5.0×200 mm stents were implanted distally, Abbott SUPERA 6.0×150 mm proximally. After the operation, the patient noted a decrease in pain.
Discussion
One subanalysis of the PARADIGM-HF study assessed the effect of sacubitril/valsartan (Uperio) therapy on measures of renal function in patients with HF, particularly creatinine clearance and urinary albumin-to-creatinine ratio. Compared with enalapril, sacubitril/valsartan was found to slow the rate of decline in GFR and have beneficial effects on both cardiovascular and renal outcomes [9]. A slower decline in GFR was observed in a wide range of patients regardless of blood pressure levels, low levels of which are known to worsen kidney function.
Similar nephroprotective effects of sacubitril/valsartan (Uperio) were previously noted in the small 36-week PARAMAUNT-HF trial in patients with preserved EF, in which sacubitril/valsartan (Uperio) also delayed the decline in GFR compared with valsartan [10].
The exact mechanism of preservation of renal function when taking sacubitril/valsartan (Uperio) is unknown, and is currently interpreted as a consequence of restoration of normal perfusion of renal tissue against the background of improved neurohormonal balance due to the protective effect of natriuretic peptides.
Experts' opinion
If Lozap does not help, there is a need to replace it with another drug. When choosing an analogue, according to experts, it is necessary to take into account the results of a medical examination, the patient’s exact diagnosis, his general health, as well as the presence of possible intolerance to certain substances.
You should not risk your health by independently replacing Lozap tablets prescribed by your doctor with other antihypertensive drugs. Consultation with a qualified specialist will allow you to choose the most effective and safe analogue of Lozap.