Coronary artery bypass surgery is a surgical intervention that is performed when the blood flow of the coronary arteries is reduced by more than 50%, and consists of creating a bypass anastomosis (shunt) of the affected area. The purpose of the operation is to restore blood circulation to the heart muscle. This is the only radical way to treat angina syndrome in coronary artery disease.
Bypass anastomosis is performed by transplanting a section of vein from the lower limb, forearm or pectoral muscle. In many countries, the operation is performed under general anesthesia using artificial circulation. For coronary artery bypass grafting in Germany, only innovative cardiac surgery techniques are used, which allows such operations to be performed on a “working” heart.
These minimally invasive techniques allow surgery to be performed through a small incision in the chest. The manipulation is performed without a heart-lung machine, which eliminates the risk of developing vascular complications, infection and shortens the recovery period.
Coronary artery bypass surgery eliminates chest pain in moderate and severe forms of angina. This is the most effective method that allows patients to perform physical activity without pain and shortness of breath and continue to lead an active lifestyle.
Indications for surgical treatment of coronary vessels
Coronary artery bypass surgery - the formation of bypass blood flow in stenotic vessels - is performed according to specific indications:
- narrowing of the left coronary artery by more than 50%;
- resistance to therapeutic methods for treating angina pectoris;
- violation of myocardial contraction;
- extensive area of ischemia;
- atherosclerotic damage to several vessels;
- arterial damage in patients with concomitant pathologies;
- narrowing of coronary vessels more than 70%.
2.Preparation for bypass surgery
Before undergoing brain bypass surgery, it is necessary to conduct a medical examination and some standard tests: ECG, general and clinical blood and urine tests, fluorography. Special examinations before brain bypass surgery include the following:
- MR, CT or intra-arterial angiography;
- Balloon examination of arterial occlusion;
- Dopplerography of cerebral arteries.
2 weeks before surgery, the patient should not smoke, drink or take drugs. It is also necessary to stop taking non-steroidal anti-inflammatory drugs.
Visit our Neurosurgery page
Heart bypass surgery in German clinics: examination plan
The study of the functional state of the myocardium consists of the following procedures:
- examination by a cardiac surgeon (drawing up treatment tactics, explaining the essence of the operation);
- electrocardiographic (ECG) recording of heart condition;
- determination of heart function under load conditions (ECG recording after bicycle ergometry);
- daily monitoring of myocardial function (Holter monitoring);
- Ultrasound of the heart;
- Doppler examination of peripheral vessels;
- 24-hour blood pressure monitoring.
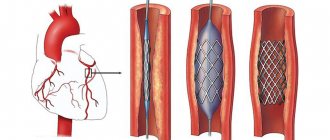
Then coronary angiography is performed, which determines the condition of each vessel of the heart muscle. In German clinics, coronary angiography is most often performed with simultaneous vascular bypass surgery. In Russia, these manipulations are carried out sequentially, which requires repeated surgical intervention on the body.
Coronary angiography is performed by inserting a plastic tube with a camera into the damaged vessel. The level of patency of the coronary artery is visually determined on the monitor. The procedure can be performed with simultaneous medical manipulations. Detection of ischemic myocardial disease is an indication for heart bypass surgery.
Expected effects
The effectiveness of the procedure varies and depends on the initial data. As a rule, after surgical treatment, the patient can expect a significant improvement in his condition.
- The number of angina attacks after coronary artery bypass surgery drops to zero. There is no pain or other symptoms. This has a serious impact on living standards. In a positive way.
- The likelihood of a heart attack also becomes significantly less. According to various estimates, successful bypass surgery of the heart vessels reduces the likelihood of acute circulatory disorders in the myocardium by 3-4 times. The risks level out and become approximately the same as in healthy people.
- Increases physical endurance and load tolerance. This is the result of adequate nutrition of the myocardium itself, muscle, and nervous tissue. The patient can walk independently, including climbing stairs without problems.
However, patients with a shunt are still not recommended to exceed the permissible, recommended norm. It is better to check with your cardiac surgeon how often and with what intensity you can engage in physical activity.
- The number of drugs is gradually decreasing. There is no need to take the same amount of medication. Although a certain minimum still remains. This is a supportive measure.
- The risk of sudden death also becomes lower.
- The patient can work. Carry out chores around the house.
The operation eliminates all possible risks. Allows you to return to a healthy life.
Advantages of coronary surgery in Germany
Surgical intervention for ischemia in German clinics is performed using a minimally invasive method on a beating heart without the use of artificial circulation. Access is made through the anterolateral surface of the chest wall. An incision up to 10 cm long is made in the third or fourth intercostal space, then coronary artery bypass grafting is performed.
The surgical technique without disconnecting the heart from the circulatory system involves separating a section of the thoracic artery. Then a section of the vessel for implantation is cut off and the cut ends are sutured. After this, they proceed to the application of anastomoses. Benefits of heart bypass surgery:
- absence of risks that occur when using artificial blood circulation;
- minimal damage to the heart muscle;
- small volumes of blood transfused;
- short treatment and recovery period;
- absence of cerebral vascular complications and infection of the postoperative wound.
Coronary artery bypass surgery, performed in German cardiology clinics, allows the patient to begin work and active life within 7-10 days. The development of cardiac surgery in Germany gives seriously ill patients a chance of recovery. After many years of suffering from attacks of angina and shortness of breath with minor exertion, patients are relieved of pain the day after bypass surgery.
Postoperative complications
Complications after surgery can develop both from the cardiovascular system and from other organs and systems. The latter, as a rule, depend on the patient’s age and the presence of chronic diseases. These include: decompensation of diabetes mellitus, exacerbation of bronchial asthma, stroke and so on. Heart failure, acute myocardial infarction and myocardial necrosis are postoperative consequences of the heart. If you are interested in the question of how long they live after surgery, then the answer will be ambiguous. The length of life after surgery depends on many factors - the age of the patient, the presence of chronic diseases, lifestyle after surgery, and so on.
At the appointment, the cardiologist will tell you how to avoid complications and what disability group the patient will receive after bypass surgery.
Cardiac surgeries without infrared apparatus
Coronary artery bypass surgery without cardiac arrest is performed only with special equipment that reduces myocardial contractions to a minimum. The anastomosis is made from the thoracic artery or vein. The use of an innovative technique in Germany makes it possible to reduce the risks associated with cardiac arrest and the passage of blood through the infrared apparatus.
However, there are cases in German practice when, for medical reasons, doctors are forced to perform bypass surgery on patients using a heart-lung machine.
Rehabilitation
{banner_banstat10}
At the early stage of recovery, the patient is in intensive care for 2 to 10 days. Plus or minus as needed. All this time, doctors are treating the stitches.
- For a period of up to six months, the patient is prohibited from heavy physical activity. Maximum 3-4 kg without bending, distributing the weight on both hands. Because the bones of the sternum are only fused. You shouldn't create additional problems for yourself. To alleviate the condition, you can wear special bandages.
- You need to walk, but overworking is prohibited. Slow step. At the same time, in order to avoid venous-lymphatic stagnation, it is recommended to wear special compression stockings.
- For a couple of months, you need a diet high in iron, vitamins and protein, but overeating is excluded, as this will put an increased burden on the heart.
Attention:
While a person is in the hospital and cannot move normally, breathing exercises are recommended. This will prevent the patient from getting pneumonia.
- After discharge, physical activity is increased gradually. As soon as the bones of the sternum have fused, you can engage in exercise therapy.
Rehabilitation continues after discharge in a special center. Once a year the patient is recommended to visit the sanatorium.
Cardiac surgeries with cardiopulmonary bypass (CPB)
Access with the traditional method is performed along the midline of the sternum. The heart is turned off from the blood circulation. Life functions are supported using an infrared apparatus, which is connected to the aorta and vena cava. The blood is saturated with oxygen and enters the body. The gas exchange process occurs in the IR apparatus itself, where the blood also maintains the required temperature and is filtered.
Coronary artery bypass surgery is performed on a non-functioning heart. The surgeon makes an anastomosis between a healthy area of the coronary vessels and a vein. The minimum time to complete the operation is three to five hours. The heart is included in the blood circulation after completion of surgery on all affected vessels.
Coronary artery bypass surgery has varying degrees of complexity. This depends on the number of arteries affected and the general condition of the patient. Therefore, the duration of the procedure is determined individually. The more anastomoses that need to be implanted, the longer the procedure takes.
results
experimental part
Tympanic shunts were used, produced by ZAO MedSil (Mytishchi, Russia) from silicone rubber impregnated with silver nanoparticles (1-3%). This composition makes it possible to supplement the hydrophobic properties of the material with bactericidal ones, which is important when the tympanic cavity is “open” for a long time [11].
Two types of functional tympanic shunts (FTS) have been developed, differing in the type of slot valve on the closed flange of the ventilation tube facing the external auditory canal. Type I slot valve had the form of a vertical cut passing through the center of a silicone membrane that tightly sealed the shunt flange. Type II consisted of two incomplete membranes overlapping each other like a “closed camera diaphragm” (Fig. 1). In our opinion, in a static situation, the valve flaps should be closed, and during barometric changes they should allow air to pass through, balancing the difference in air pressure between the tympanic cavity and the external environment.
Rice. 1. Diagram of slot valves. a - type I valve, b - type II valve.
To objectively evaluate the operation of the slot valve mechanisms of the FTS, an experimental model was developed. The external auditory canal with PD was represented by a silicone tube 1.3 cm long. A shunt was sealed into the closed distal end of the tube. Depending on the type of FTS used, two types of models were obtained. The operation of a conventional slot valve was studied on experimental model No. 1, and the diaphragmatic valve was studied on model No. 2. The models were tightly connected to an earmold attached to the probe of the AT 235 h computer analyzer (Interacustics, Denmark), and the test was carried out in ETF2 mode (Fig. 2). The device pumped air and recorded the barometric indicator at which pressure was released. The experiment was repeated 10 times and the average value of the barometric indicator was calculated.
Rice. 2. Preparation for the experiment (the model is fixed on the probe of the AT 235 h computer analyzer).
As a result of the experiments, it was noted that when air is pumped into model No. 1 (ETF2 mode), there is no pressure rise - the studied indicator is constantly equal to 0 daPa. This indirectly indicates that this slot valve design does not have a barometric resistance threshold. A similar experiment with model No. 2 led to a rise in pressure to 123.06 daPa, after which there was a sharp drop to the initial “zero” threshold (Fig. 3). Our results indicate that model No. 2 operates as a barometric valve. The diaphragm-slit valve opens when the pressure difference is 123.06 daPa. Taking into account the results obtained in the experiment and the peculiarities of the physiological mechanisms of passive opening of the CT, in the clinical part of the work, a FTS equipped with a diaphragm-slit valve (type II valve) was used.
Rice. 3. Experiment results in ETF2 mode. a - model No. 1; b - model No. 2.
Clinical part
Preoperative examination of patients ( n
=104) showed that all patients complained of unilateral hearing loss and a feeling of fullness in the ear.
In 86 (82.7%) patients, inflammation of the middle ear was recurrent. The duration of the last episode of the disease was 67.85±8.27 days ( p
<0.05).
At the same time, the conservative treatment carried out (catheterization of the CT with the introduction of anti-inflammatory drugs, pneumomassage of the BP, decongestants and targeted anemization of the mucous membrane of the CT orifice, intramyocardial compresses and physiotherapeutic effects) was not effective. An endoscopic examination of the nasal cavity revealed a pronounced deformation of the nasal septum and enlarged posterior ends of the inferior nasal conchae, which reached the orifice of the S.T. During diagnostic anemia, the posterior parts of the inferior turbinates did not contract. Using PARM, a pronounced disturbance of nasal breathing was detected in 100% of patients: a decrease in the total volumetric flow - 280.22±11.03 cm3/s and an increase in the total resistance - 0.58±0.03 Pa ( p
<0.05).
Otomicroscopy revealed retraction and thinning of the PD in 52 (50%) patients (52 ears), and the presence of isolated petrification with areas of atrophy. In 52 (50%) patients (52 ears), the contours of exudate in the tympanic cavity were observed. In all patients, Rinne's tuning fork test (C128) was negative. In Weber's experience, lateralization into the affected ear occurred in 82.7% of patients, without clear displacement in 17.3%. The results of Federici's experiment (C128, 512) were doubtful in 93 (89.4%) patients, and positive in 11 (10.6%). According to TPA data, 61 (58.7%) patients were diagnosed with low-frequency conductive hearing loss, and 43 (41.3%) with mixed hearing loss, while the air-bone interval (ABI) was 29.84 ± 4.56 dB. During acoustic tympanometry, changes in gradient and compliance parameters were observed. In 52 (50%) patients (52 ears), the computer analyzer of the middle ear ATF 235 h recorded type C sympathogram, in 52 (50%) patients (52 ears) - type B. At the same time, the pressure in the tympanic cavity was - 266.37 ± 11.08 daPA ( p
<0.05). When studying the function of the CT using functional tests in the ETF1 mode, in 100% of studies (104 ears), no positive dynamics in the values of intratympanic compression were detected. Thus, in 52 (50%) patients (52 ears) catarrhal otitis media was detected, in 52 (50%) patients (52 ears) - exudative. The pathological process in 100% of cases (104 ears) was associated with severe long-term DST.
To consistently solve our problems and in accordance with the principle of randomization, all patients were divided into two clinical groups, differing in the method of treating long-term DST (type of tympanic shunt). In the 1st clinical group ( n
=52) in case of catarrhal and exudative forms of otitis media, BP shunting was performed with standard shunts (SS).
In the 2nd clinical group ( n
= 52), for exudative otitis, a SS was used; in the stage of catarrh or when the exudation process stopped, a FTS, equipped with a diaphragm-slit valve, was used. The types of tympanic shunts that were used in the clinical part of the work are presented in Fig. 4.
Rice.
4. Silicone tympanic shunts. (on the left - FTSh, on the right - S.Sh. In the background is the “foot” of tweezers). Depending on the form of the inflammatory process in the middle ear, two subgroups were divided into each clinical group (26 people/ears each): subgroup A consisted of patients with catarrhal otitis media; subgroup B - with an exudative form of inflammation in the middle ear. The effectiveness of the treatment was assessed by local clinical manifestations, recovery time of the ventilation function of the CT and hearing acuity, and the nature and frequency of complications.
Risks of using an IR device
Vascular bypass with open access and cardiac arrest is associated with the risk of developing the following complications:
- possibility of bleeding;
- necrosis of a portion of the heart muscle;
- incomplete fusion of the thoracic incision;
- renal failure;
- venous thromboembolism;
- cerebral artery stroke;
- amnesia (memory loss);
- large scars on the chest;
- pronounced pain symptom.
After the operation, until the postoperative wound has completely healed, you should not take a bath, use gels, or rub in the suture area. You should not take a hot shower or use lotions.
Forecasts and service life of shunts
The prospects are generally favorable. The likelihood of a heart attack is reduced by 2-4 times, the same applies to sudden death.
If the heart is not changed, you can return to a full life with minor restrictions in physical activity. The operation does not affect its duration in any way, but reduces the risks of emergency conditions.
The shunt, under ideal conditions, lasts about 10-15 years. But there are errors. Therefore, you should count on a time frame of 7-8 years or so.
Afterwards, indications for cardiac bypass surgery arise again and auxiliary therapy is needed.