We continue our series of publications about laboratory blood tests. On our portal you can find useful information on how to independently decipher indicators in general and biochemical analyses, as well as in the lipid profile. This time Dr. Fedorov answers questions about platelet levels in the blood:
- What does a decrease in platelet levels in the blood indicate?
- What does an increase in platelet levels in the blood indicate?
- How does a blood clot form? Why is a test for induced platelet aggregation prescribed?
- Why is it important to order a blood test for platelet resistance to aspirin and clopidogrel?
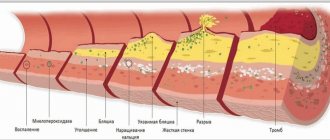
The ability of blood to clot is one of the foundations of life. After all, if this mechanism had not been laid down, any, even the most insignificant wound, would become mortally dangerous. A number of biochemical compounds, which are usually called factors, are responsible for the coagulation system, but the basis of the process is the smallest formed elements of blood - platelets. Unfortunately, disruption of this system can lead to consequences no less serious than bleeding.
An excess of platelets threatens to increase the risk of intravascular thrombus formation; low platelets in the blood are the cause of internal hemorrhages.
What does a decrease in platelet levels in the blood indicate?
The lower limit of normal blood platelet content is 150 thousand/μl. The reason for the decrease in PLT (platelet designation in a blood test) may be numerous but rare congenital thrombocytopenias (Fanconi syndrome, Wiskott-Aldrich, etc.), as well as acquired thrombocytopenias. The most common cause of acquired ones is the constant use of antiplatelet drugs, especially with two-component therapy (acetylsalicylic acid + clopidogrel); fortunately, the number of platelets in this case is usually not greatly reduced. Other causes of low blood platelets include bacterial and viral infections, anemia, splenomegaly, congestive heart failure, etc.
Clinical signs of platelet deficiency (bleeding gums, bruising, frequent hemorrhages in the sclera, etc.) appear when the platelet level drops below 50 thousand/µl - this is the indicator when you need to see a hematologist immediately.
What does an increase in platelet levels in the blood indicate?
The upper limit of normal platelets in a blood test is 400 thousand/µl. Increased platelet levels are much more likely to occur for physiological reasons. These are so-called reactive thrombocytosis. Their cause may be recent physical overexertion, past stress, dehydration, that is, physiological thickening of the blood. Pathological factors most often include those that also thicken the blood - anemia due to chronic blood loss or acute blood loss, dehydration as a result of intoxication. The reasons for an absolute increase in platelet levels include inflammatory diseases, tuberculosis, malignant neoplasms in general and the hematopoietic system in particular.
An increase in platelet levels above 500 thousand/µl significantly increases the risk of thrombosis and requires the selection of antiplatelet therapy - the use of special drugs.
B12 deficiency anemia - symptoms and treatment
To correctly diagnose B12DA, an examination by a hematologist is important. To clarify and correct problems associated with the gastrointestinal tract, you will need to consult a gastroenterologist. An examination by a neurologist may be necessary to evaluate neurological manifestations.
Patient examination
During examination, the doctor may notice pallor and slight jaundice of the skin, an increase in heart rate and expansion of the boundaries of the heart. It is necessary to examine the oral cavity, especially the tongue. A neurologist can assess muscle tone and the presence of pathological reflexes.
Laboratory diagnostics
One of the most important stages of diagnosis is the evaluation of a clinical blood test . The analysis shows:
- decreased hemoglobin - anemia;
- macrocytosis - the presence in the blood of a large number of abnormally large red blood cells (macrocytes);
- hyperchromia - intense staining of red blood cells caused by an increased amount of hemoglobin in the blood;
- a decrease in the number of leukocytes and platelets may be observed.
It is necessary to perform a blood smear , in which a morphologist can see pathological forms of red blood cells:
- ovalocytes (oval-shaped red blood cells) and degenerative forms;
- an increase in the difference in erythrocyte size (RDW parameter);
- specific pathological inclusions, such as Jolly bodies and Cabot rings;
- megalocytes and megaloblasts - in severe cases.
Pathological forms of neutrophils may also occur:
- giant neutrophils;
- neutrophils with nuclear hypersegmentation (5 or more segments);
- metamyelocytes are immature neutrophilic leukocytes.
The number of young forms of red blood cells (reticulocytes) is usually reduced. If laboratory capabilities are available, additional useful information can be provided by reticulocyte indices: the average volume of reticulocytes and the average hemoglobin content in reticulocytes increases, the fraction of immature reticulocytes increases [1][2][4][5].
In a biochemical blood test:
- decreased levels of vitamin B12;
- indirect bilirubin and lactate dehydrogenase may be increased - a sign of early destruction (hemolysis) of red blood cells in the blood and the breakdown of red blood cell precursors in the bone marrow [4];
- Iron and ferritin levels are normal.
It is imperative to evaluate folic acid levels , since changes in clinical analysis for B12 and folic acid deficiency are similar, but treatment is different. If B12DA is suspected, but vitamin B12 and folic acid levels are normal, serum holotranscobalamin (active vitamin B12) determination is recommended. In case of B12 deficiency, its content is reduced. Increases in serum homocysteine and methylmalonic acid levels may be detected [2][3].
In a general urine test, persistent proteinuria may be observed - the appearance of protein in the urine. In some cases, there is an increase in the level of methylmalonic acid and homocysteine.
Additional laboratory tests that may help identify the cause of vitamin B12 deficiency:
- study of antibodies to internal Castle factor (IgG) and gastric parietal cells in blood serum;
- examination of gastric juice to identify internal Castle factor and antibodies to this factor (IgA, synthesized by parietal cells of the stomach);
- Schilling test - determines the activity of the intrinsic factor of Castle and the absorption of vitamin B12 in the intestines;
- tests for malabsorption (impaired absorption of nutrients) [5].
Prenatal diagnosis of genetically determined deficiency of the transport protein transcobalamin II is possible
Instrumental diagnostics
Ultrasound examination of the abdominal organs can detect minor hepatosplenomegaly - enlargement of the liver and spleen.
To identify diseases of the gastrointestinal tract that may interfere with the absorption of vitamin B12, all patients with newly diagnosed B12DA are recommended to undergo endoscopic examinations - fibrogastroduodenoscopy (EGD) and colonoscopy . FGDS may reveal chronic atrophic gastritis, duodenitis, and a decrease in gastric secretion may be observed. In the presence of pathological changes, it is necessary to perform a biopsy of the gastric mucosa with further histological examination [3][4].
Differential diagnosis
Differential diagnosis for B12-deficiency anemia, especially with a decrease in leukocytes and platelets, is carried out with the following diseases of the blood system:
- Myelodysplastic syndrome is a group of hematological diseases in which the bone marrow does not produce enough of one or more types of blood cells: platelets, white blood cells, red blood cells.
- Aplastic anemia is anemia that occurs due to insufficient production of red blood cells due to a decrease in the number of hematopoietic stem cells.
To clarify the diagnosis, it may be necessary to perform a bone marrow puncture and its morphological examination. If B12DA is present, a morphologist describes characteristic changes in stem progenitor cells in the bone marrow:
- hyperplasia (proliferation) of the erythroid germ - stem progenitor cells from which red blood cells are formed;
- megaloblastic type of hematopoiesis, in which large cells with granular nuclei, pathological mitoses, and Jolly bodies are formed;
- impaired maturation of myeloid cells and platelet precursors: giant metamyelocytes, hypersegmentation of neutrophils, multinucleated megakaryocytes [1][2][3][4].
How does a blood clot form? Why is a test for induced platelet aggregation prescribed?
Normally, platelets in the blood are in an inactive state; the cells have a discoid, slightly elongated shape, which is why in old textbooks they are called “blood plates.” When bleeding begins, platelets are activated: they acquire a spherical shape and form special outgrowths - pseudopodia. With their help, they can connect with each other (aggregate) and stick to the site of damage to the vascular wall (adhere). These two processes provide the basis for thrombus formation.
To assess the quality of platelet aggregation and find out whether it is reduced or, conversely, does not occur too intensely, an analysis for induced platelet aggregation is prescribed. To do this, they take blood from a vein, add special substances (activation inducers) to it and evaluate the process.
When preparing for the study, it is important to comply with certain conditions - for 3 days, follow a special diet prepared by a doctor, 24 hours before, avoid taking stimulants (coffee, alcohol, nicotine, garlic) and immunostimulant drugs, 8 hours before, stop taking medications and fatty foods.
Low platelet activity occurs in diseases of the hematopoietic system, constant use of antiplatelet drugs, in this case the duration of bleeding increases. Increased aggregation, on the contrary, increases the risk of thrombosis: venous thrombosis, heart attack, stroke. You may ask, why order an induced activation test if the risk of bleeding/thrombosis can be assessed by the total platelet count? Alas. Even with normal numbers, most of the cells may turn out to be “defective”, so we are talking about severe platelet deficiency with their normal concentration in the blood.
Normal indicators
The PCT indicator, which is nothing more than thrombocrit, cannot be determined without special modern equipment, since platelets, being outside the bloodstream, are able to “overgrow” with pseudo-similarities.
At the same time, they still manage to increase in size at least ten times. It is for this reason that a laboratory technician cannot do without an automatic analyzer when determining the thrombocrit index. Determination of thrombocrit level in blood
The norm for this indicator ranges from 0.15 to 0.4. In some medical publications you can find information in which the thrombocrit norm differs slightly from that indicated, but only slightly. The norm for this indicator in an adult, an infant or in children of different ages is proportionally different from each other. At the same time, a proportional change in the indicator is not observed due to physiological fluctuations.
In particular:
- during the day or at different times of the year, the thrombocrit indicator may deviate by 10% (in particular, when depression occurs at night or in early spring);
- in women, thrombocrit is reduced by 50% during menstruation, as well as during pregnancy (this is a kind of protective reaction of the body that prevents the formation of blood clots);
- Thrombocrit indicators will be doubled if the patient was subjected to significant physical activity before the analysis.