Have you ever encountered cases of “miraculous healing” of your patient or “unexpected deterioration” of his condition according to a general blood test? Or when the real clinical situation completely does not correspond to the laboratory data? “The laboratory is lying again,” you thought. However, in fact, much in the overall analysis depends on how the patient was prepared, how the blood was drawn and how it was delivered to the laboratory, i.e., on the preanalytical stage. Let us consider separately each factor of the preanalytical stage that can distort the result of the OAC.
Our expert:
Irina Petrovna Tereshchenko
Candidate of Medical Sciences, Clinical Laboratory Diagnostics Doctor, Lecturer at State Autonomous Educational Institution NSO “Center for Advanced Training of Healthcare Workers”
In developed countries, about 70% of errors in laboratory medicine are associated with the non-laboratory part of the preanalytical stage. The structure of errors is as follows: taking blood from a vein for infusion - 20.6%, omission of analytes in the application - 18.1%, patient name - 2.6%, wrong tube (anticoagulant) was used - 2.6%, collection conditions were violated blood - 2.1%.
Moshkin A.V., Dolgov V.V. Quality assurance in clinical laboratory diagnostics, 2004
The KLA evaluates not only the number of blood cells, but also other indicators: size, shape, volume, surface properties. Unfortunately, it is impossible to completely avoid changes in cells when they are placed in artificial conditions. Blood cells not only have different structures and functions, but also different resistance to factors affecting the processes of taking a blood sample and preparing it for research. Errors in the CBC have serious consequences: incorrect or “missed” diagnosis, untimely correction or unnecessary drug intervention.
Factor #1: Finger or Vein?
Comparisons of two CBCs collected under different conditions/from different sources (from a vein and from a finger) should be done with caution. Indicators of capillary and venous blood may differ.
The ulnar vein is the optimal place for blood collection for general analysis, taking into account the requirements of standardization and the exclusion of preanalytical influences. However, the choice of material for testing the CBC remains with the laboratory. The only way to reduce the occurrence of interpretation errors associated with the selection of study material is to adhere to a uniform preanalytical methodological framework offered by the laboratory.
When taking blood from a finger, a number of features are possible that are difficult to standardize: cold, cyanotic, swollen fingers, the need to dilute the blood being tested, and others. Tissue fluid, which inevitably ends up in capillary blood, contains thromboplastin, which promotes the formation of microclots.
If the laboratory works with venous blood to study the cellular composition, then it is recommended to take capillary blood in the following cases:
- the need for daily monitoring of blood counts, for example in cancer patients undergoing chemotherapy;
- for burns of a large surface area of the body;
- in the presence of hard-to-reach veins;
- with severe obesity;
- with an established tendency to venous thrombosis;
- in newborns.
How it affects: There may be a significant scatter in the results obtained, which are leveled out in repeated samples. The number of erythrocytes, hematocrit, qualitative composition of the leukocyte formula and ESR in an analysis performed under different conditions in the same patient may change regardless of the course of the underlying pathological condition. Capillary blood contains a higher content of leukocytes and a lower content of platelets compared to venous blood.
Non-pathological origin of hematoma
A bruise after a blood test from a vein may appear due to an incorrectly performed medical procedure or due to the fault of the patient himself. Medical errors in collecting biofluids include:
- Dull needle. It is not common, since taking biomaterial with a syringe is gradually becoming a thing of the past. Most hospitals and clinics use modern vacutainers to take blood for analysis, which minimally injure tissue.
- Low qualification of personnel. In the absence of experience or crude manipulation, the nurse can puncture both walls of the vein (through and through). Another reason for a bruise associated with unprofessionalism is the inability of a medical worker to cope with a difficult patient. Individual characteristics are expressed in the presence of so-called floating veins, excess weight, and naturally too thin veins. Insufficient qualifications include improper treatment of the intended puncture site with an alcohol solution.
- Incorrectly selected area from which the blood was taken. Before the procedure, the medical professional must carefully examine the patient’s veins and make a puncture in the most convenient place (from the point of view of collecting biofluid).
Vacuum blood sampling system reduces the risk of complications after the procedure
The bruise that appears may be the result of a puncture of an existing blood clot in the vein. This condition is observed:
- after prolonged injection therapy for a particular disease;
- if the instructions for use of the medicine are not followed (some drugs require administration at a certain speed);
- in people suffering from drug addiction, with punctured veins.
Clots form due to regular injury to the venous walls. The most common cause of hematoma is the patient's failure to comply with medical recommendations. Before donating blood, you should not take drugs from the pharmacological group of anticoagulants that thin the blood (Aspirin, Thrombo ACC, Heparin, Warfarin, etc.).
After the test, a cotton swab soaked in an alcohol solution is applied to the damaged area. It must be pressed firmly with your finger and your arm bent at the elbow. The tampon must not be removed until the bleeding has stopped completely! The blood that has not had time to clot flows under the skin, forming a hematoma. In addition, after the procedure, it is forbidden to load the injured limb for several hours (lifting weights, playing sports, etc.).
Important! To avoid unpleasant consequences of donating biomaterial, the patient must follow the doctor’s recommendations.
Factor No. 2. Tourniquet/not tourniquet
When collecting blood from the cubital vein, you do not need to squeeze your hand. The hand should be relaxed. When using a tourniquet, the optimal application time is no more than 2 minutes.
How it affects: A tourniquet applied for 4 minutes will increase the hemoglobin level by an average of 4 g/l, and for 6 minutes - by another 4 g/l. These differences can be very significant for people with anemia.
A widespread mistake in the preanalytical stage is “mixed-up tests.” Therefore, the basic rule of the nurse is to identify the patient before each blood draw!
Causes
Hemorrhage usually occurs after injury. This could be a bruise of the skin, internal organs, a concussion or bruise of the brain, an injection with thin (sharp) objects. Sometimes blood leaves the vessels and pours into the skin and internal organs as a result of infections, autoimmune diseases, and poisoning. The occurrence of hemorrhages and bruises is promoted by increased fragility of blood vessels, fasting, lack of vitamins in food, high blood pressure, and congenital bleeding disorders.
At CELT you can get a consultation with a traumatologist-orthopedic specialist.
- Initial consultation – 3,000
- Repeated consultation – 2,000
Make an appointment
Factor No. 5. It's in vitro...
For blood collection, it is better to use vacuum tubes of a standardized volume, since this will avoid damage to the formed elements, especially red blood cells. In practice, when a laboratory switches from one type of tube to another, the CBC results may be distorted, which does not depend on the patient’s underlying disease.
How it affects: It is possible to change the hemoglobin amount indicator (both towards overestimation and towards underestimation), as well as the associated calculated indices (MCH, MCHC).
Three reasons for patient-related variability in CBC results:
- Biological variation: interindividual (race, gender, age) and intraindividual (biorhythms, pregnancy, diet, physical activity, alcohol consumption, smoking);
- External conditions (climate, atmospheric pressure, stress, drugs, medications);
- A change in body position (transition from a lying position to a sitting or standing position) leads to hydrostatic penetration of water and filtered substances from the intravascular space into the interstitial space. It is possible to increase the concentration of hemoglobin, hematocrit, and the number of leukocytes.
Treatment process
There are several methods for treating a hematoma on the arm. To do this, you can use a pharmaceutical drug or a folk remedy. Among the most effective methods of therapy are:
- Cold treatment. If a bruise appears on your arm, you should immediately apply ice cubes to the injured area. Thanks to the cold, blood vessels narrow. It is not advisable to keep the bruise cold for a long time, as hypothermia may occur. The entire process should last no more than 15 minutes.
- An elastic bandage will effectively solve the problem. To do this you need to bandage your hand. This will prevent the process of hemorrhage into the tissue. Thanks to this, the hematoma will not grow to a large size.
- Using a heating pad can help relieve pain. The heat dilates the blood vessels and the fluid is quickly absorbed. To do this, you can use either a heating pad or a bath.
An iodine mesh will help get rid of a bruise. To do this, you need to draw a mesh on the hematoma. With this simple method you can quickly get rid of a hematoma.
Factor No. 6. “Easy”
It is recommended that blood collection be done early in the morning after a 12-hour fast and no changes in diet for 24 hours. The patient should go to bed at the usual time the day before and get up no later than an hour before blood collection (baseline).
How it affects: Important for hemoglobin levels. Sample turbidity, even slight, distorts photometric data. Hemoglobin is likely to be elevated, which will affect the control of anemic patients. The MCHC indicator can serve as a control over the correctness of hemoglobin measurement.
Mechanism of occurrence
A hematoma is formed due to a puncture of the skin and vein. Blood flows out and flows to the injured area. Therefore, after taking the test, you are asked to press your hand tightly to your forearm to stop the bleeding.
The bruise forms in the hypodermis. The layer above, the dermis, contains nerve endings that allow you to feel pain and discomfort. Damage is reflected on the top layer of skin in the form of a blue spot.
The intensity of the resulting bruise depends on the condition of the vessels, their structure, and the thickness of the adipose tissue.
Factor No. 7. I worked hard and got nervous
Physical activity, especially intense or unusual for the patient, can increase the CBC indicators, namely the number of red blood cells, white blood cells and hematocrit. Psycho-emotional stress will also affect the number of leukocytes. In this case, chronic severe stress is considered as a basic pathological condition, and acute stress is taken into account, for example, with sensitivity to service in municipal institutions.
How it affects: For biological variation, the most sensitive indicator is leukocytes. Physical overexertion in combination with deviations in the time of sampling can change the number of leukocytes by ± 4 × 109/l.
Prevention
In order to avoid the formation of a bruise or bump after an injection into a vein or taking tests, you must:
| Preventive actions | Description |
| Relaxation of arm muscles | During the procedure, you need to relax your hand as much as possible, since when the muscles are tense, the likelihood of tissue damage increases significantly |
| Choosing the right needle size | To administer the medicine, you must use a syringe with the appropriate needle diameter. If a large volume of fluid is injected with a thin needle, the likelihood of bruising at the injection site increases. |
| Rate of drug administration | The medicine must be injected smoothly and slowly to avoid leakage of the solution into the tissue surrounding the vein |
| Measures after the end of the procedure | After the injection, cotton wool soaked in alcohol is pressed firmly against the vein puncture site for 5–7 minutes. |
If the hematoma at the injection site reaches a large size and quite severe pain or cramps occur, you should consult a doctor.
This may mean that the vein is seriously damaged and may require the help of a surgeon.
Factor No. 8. “Casual” smoking
A mandatory point that must be taken into account by the clinician is smoking. The condition where the patient is a chronic smoker is regarded as the basic condition. If a person was forced to quit smoking and this fact is unknown to the attending physician, then the number of erythrocytes, platelets and hematocrit are subject to changes in the CBC, and the changes can be of a different nature. Particular attention should be paid to adolescents - a group of patients who smoke rarely and irregularly.
How it affects: “Sudden” smoking before taking a blood test can overestimate the number of red blood cells by 10%.
Diagnostics
A hematoma is diagnosed by visual examination. If the hemorrhage is located deep under the skin, in internal organs, or in a joint, it is often very difficult to assess its size and possible consequences.
Patients are prescribed an examination, which may include:
- Ultrasound of internal organs, joints;
- computed tomography and magnetic resonance imaging;
- puncture (puncture with a needle): for example, a puncture of the knee joint is often done if there is a suspicion that blood has accumulated in it after an injury.
Factor No. 9. Drugs/medicines
Medicines and their metabolites can change OAC parameters due to a physicochemical effect on the procedure or due to their interaction with the device and reagents.
If the patient takes medications, especially in large dosages, such as antipyretics, analgesics, antibiotics, antispasmodics, it is necessary to take into account the effect of their metabolites on blood pH. The more medications a patient takes immediately before donating blood, the higher the likelihood of distorting the result. In addition, the presence of active metabolites significantly reduces the standardized time available for analysis. For UAC, the optimal execution time is considered to be 2 hours, within which the material remains as stable as possible. For CBC calculated on a hematology analyzer, this time is 6 hours. For OAC, if the patient has taken a large amount of medications, the time can be reduced to 30 minutes for any type of study.
Life-saving medications should be taken as usual! Their presence in the blood is the basic state from which dynamics are assessed.
How it affects: When a blood test with drug metabolites is carried out later than the established time interval, the volume of leukocytes changes, the volume of erythrocytes increases, which leads to errors in the morphological differentiation of leukocytes and calculated erythrocyte indices.
The platelet count when taking antiplatelet agents (NSAIDs, acetylsalicylic acid) may be underestimated by the analyzer. Falsely elevated MCV index can occur with hyperglycemia and ketoacidosis due to plasma hyperosmolarity.
If there is an excess of medicinal metabolites in the blood, the morphological characteristics of neutrophils and monocytes will change, the volumes will decrease and the form of other elements of the blood test will change. In practically healthy people, changing the basic parameters of cells will not cause significant changes in the count. The state of pathological elements in severe diseases cannot be standardized; the only requirement is to minimize the time before starting the analysis.
Pharmacy products
- Healing ointment – Troxevasin. Relieves swelling, relieves pain, improves tissue nutrition. Apply three times a day.
- Heparin ointment resolves the formed hematomas and relieves pain. Use 2-4 times a day. The frequency of application depends on the degree of damage to the integument. Treatment can be continued for 2–5 days.
- Hirudoven contains leech extract. He quickly copes with the resulting bruises. Apply up to 3 times a day.
- Dimexide relieves inflammation, accelerates skin renewal and kills germs. Used as a solution with water in the following proportion: 1 part dimexide to 4 parts water. It is applied to gauze or cotton wool and applied to the damaged area.
- Additionally, ointments and gels containing arnica or badyagi, Lyoton gel will help.
Factor #10: Time
The general rule for transporting any biological material is delivery to the laboratory as soon as possible.
How it affects: In addition to changing the morphology of cells, the delivery time can change quantitative indicators, especially if the temperature regime has been violated: an increase in blood viscosity when it is cooled during storage or transportation, the presence of microclots due to poor mixing with the anticoagulant immediately after blood collection. The most sensitive indicator is red blood cells: their number will be falsely underestimated.
Clinical guidelines
Errors of health workers when working on the analysis amount to 0.5–10%. This is often due to improper blood sampling.
Blood sampling must take place in a sterile room, using sterile instruments.
Step-by-step instruction:
- The container for collecting biomaterial is prepared in advance. It is marked, and the patient’s data is entered into a journal.
- The patient is seated on a chair, his hand is placed on the manipulation table.
- The limb is extended as much as possible, relaxed and placed on the cushion.
- The rubber band is fixed in the middle of the shoulder.
- The elbow bend is wiped with a cotton swab dipped in medical alcohol.
- The subject is asked to clench and unclench his fist several times.
- The vein is pierced with a syringe at an acute angle. Blood sampling occurs up to a certain point.
- Even before a complete analysis is taken, the tourniquet on the arm is unfastened. The syringe is removed.
- The subject is given a cotton ball soaked in alcohol.
- To prevent the formation of a bruise, the patient presses the hand with the cotton wool firmly against the shoulder.
The patient is prohibited from lifting weights, washing in hot water, or getting the damaged area wet on the first day.
The puncture is treated with an antiseptic until it is completely healed.
Doctors will find it useful
If you see that “the laboratory is lying,” check: where the material was taken from, by whom and under what conditions. Comparison of indicators performed under the same conditions (laboratory, personnel, methodology) is considered correct.
Find out from the patient what happened before the analysis: physical activity, stress, taking medications, smoking. Warn patients that before the test, if there is no urgent need, it is better to postpone taking medications. It is ideal to withhold medication for 12 hours - this is the standard half-life for most medications. Warn the patient to maintain a state of psycho-emotional and physical rest before the blood collection procedure.
And only by eliminating factors that could influence the preanalytical stage can the obtained changes be compared with the patient’s clinical indicators in order to provide him with quality medical care.
Patient errors
After drawing blood, the arm is bent and the puncture is covered with cotton wool. This must be done to give the blood time to clot and the puncture to heal. If you straighten your arm prematurely, a bruise will appear.
Blood thinners or pills with the same side effect cause a blue spot to form on the skin. The thinned blood moves faster through the tissues, thereby creating a hematoma.
Basic methods of treating veins
After introducing the cytostatic into the cells, all that remains is to wait for the completion of the side process and help recovery.
The pathophysiology of drug-induced toxic phlebitis has been little studied, no clinical studies have been conducted on the problem, all recommendations are based only on the personal experience of medical personnel. In each case and after each administration, it is necessary to consult with the attending physician who knows the specifics of the local interaction of the cytostatic and the range of local adverse reactions.
To relieve pain and reduce inflammation, NSAIDs are best suited - non-steroidal anti-inflammatory drugs, but the benefits of any one drug have not been proven; it is better to rely on the patient’s “everyday” preferences, because sensitivity to pain is different, and the analgesic effect is also individual.
If there is a high risk of pulmonary thromboembolism, the patient is prescribed a special “blood thinning” therapy, usually long-term - at least a week and with regular monitoring of coagulation.
You can use ointments with heparin to rub into the area of the damaged vessel. Hepatrombin™ gel consists of heparin and prednisolone, the latter has an anti-inflammatory effect, the drug is not officially certified for use in peripheral phlebitis and thrombophlebitis.
Troxevasin™ ointment has a good reputation , which simultaneously reduces inflammation and swelling of tissues, changing the rheological properties of blood towards dilution, but less than is typical for heparin. However, studies have shown that the drug is capable of dissolving microthrombi.
Indovazin™ gel is a mixture of troxerutin and the NSAID indomethacin, therefore it reduces the severity of pain and does everything that is inherent in Troxevasin™. It is not advisable to combine both ointments, since the spectrum of action of the combined drug is greater, but with Indovazin™ it is quite possible to alternate the application of Hepatrombin™. The absorption of ointments is microscopic; they do not replace NSAIDs and anticoagulants taken orally, but they help to endure the unpleasant consequences of treatment.
How to prevent a bruise
- The cotton wool should cover the site of blood sampling well, and the hand should be pressed firmly against the forearm for 5–10 minutes. Then the blood will not actively spread through the tissues, forming a hematoma.
- During blood sampling, you should relax, paying attention to the muscles of your arm. If they are overexerted, the tension will increase, which contributes to injury and the rapid spread of blood.
- Do not move, fidget in your chair, or nervously jerk your hand. Such movements will only cause additional damage.
- After the procedure, you should not lift heavy objects or actively use the injured arm for the next 1–2 days. This will cause discomfort and may cause hematoma formation.
- Find a qualified employee. The healthcare provider bears most of the responsibility for the successful completion of the procedure.
Stool examination
The state of a person’s digestive tract can be revealed by their feces. When analyzing this biomaterial, the following matters: color, smell, hardness and even weight. Most often, excrement consists primarily of water, food debris, bacteria and removed mucosal cells. The color of feces comes from decomposed bile pigments.
A stool examination is necessary if complaints from the digestive tract occur over a long period of time. For example, cramping, pain, diarrhea or constipation. Regular stool testing is especially recommended for people aged 50 years and older. To detect cancer at an early stage if necessary.
Collection conditions:
- Collect the stool in a designated container;
- Label and date the container.
Stool analysis allows you to diagnose various diseases. Stool is often tested for the presence of blood adjuvants as part of colorectal cancer screening or for early detection of cancer precursors. However, stool testing can also detect the presence of worm eggs or bacteria in the stool.
How veins are restored after IVs: useful procedures
They try to reduce local irritation of the mucous membrane lining the inner wall of the vein by large dilutions and slow administration in droppers, literally over hours. Not all cytostatics can withstand high dilution and long administration; some lose their properties, so they are administered as a bolus using a syringe. In this case, immediately after chemotherapy, the vein is “washed” with saline, trying to reduce its damage.
Be sure to check the patency of the vessel and the possibility of extravasation - the spread of cytostatics in the tissue during microscopic ruptures of the vascular wall - before administration and during the drip.
It is recommended not to administer chemotherapy to the same vein; it is better to alternate hands, giving the vessel more time to restore its mucous membrane. The prophylactic use of ointments with heparin or troxerutin before chemotherapy has no pathomorphological basis, that is, it is useless.
When planning multi-month chemotherapy, it is advisable to think about installing a venous port; its service life is at least five years. The device completely eliminates such a side effect as drug phlebitis, but only taking anticoagulants can save you from thrombosis.
Possible complications
A hematoma does not pose a danger to humans, but sometimes it is accompanied by other complications:
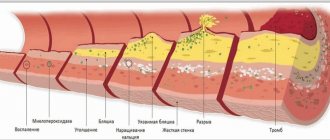
- Phlebitis. This is an inflammation of the venous wall that can occur due to damage. The site of the fence begins to swell, turn red, and hurt. The temperature is rising.
- Thrombophlebitis. This is phlebitis complicated by a blood clot. Usually, a compaction appears at the site of the blood clot. The hand becomes swollen and constantly hurts. In some cases, surgery is prescribed.
- Thromboembolism. A serious complication that, without treatment, can lead to gangrene. Natural blood circulation is disrupted, and the hand changes its natural color and swells.
- Abscess. Occurs when dirt gets into the puncture site. Inflammation begins and pus accumulates.
- Phlegmon. Inflammation of soft tissues, which does not have a clear localization, is accompanied by purulent discharge. Causes pain, inflammation, fever.
Preventing complications
- Avoid taking hot showers and baths for 2-3 days. Use moderate water temperature.
- Avoid heavy lifting until your arm stops hurting.
- For the first 2–4 days, you need to monitor hand hygiene and use antibacterial soap. An infection can develop from the slightest ingress of dirt or germs.
- Stop drinking coffee for a while, it increases blood pressure and provokes hemorrhage in the damaged area.
- Take a course of vitamins that strengthen the walls of blood vessels. For example, Ascorutin, it simultaneously improves immunity due to the concentrated content of vitamin C.
- A healthcare professional should be monitored during the test. He must print new gloves and a syringe with the patient. The entire inside of the elbow bend is wiped with an antiseptic solution. Otherwise, there is a risk of infection, which will lead to an abscess, phlebitis or thrombophlebitis.
- Until the puncture is completely healed, it must be treated and covered from moisture and dirt. When drawing blood, you should follow your doctor's instructions and press your hand firmly for a few minutes. If all recommendations are followed, the patient can independently minimize the risk of hematoma formation.
Video on the topic: