Choroid plexus cyst in fetus and adult: causes, symptoms
Choroid plexus cyst (CPC) in the fetus and newborn is an ultrasound term formed due to excess accumulations of cerebrospinal fluid along the vessels. In most cases, as the baby grows, the formations go away on their own. If the structures are preserved, they do not pose a danger to the child's health. If the structures are preserved, they do not pose a danger to the child's health. Only in rare cases is surgery required to remove an overgrown cystic cavity.
The optimal period for diagnosing formations is the fetus at 18-22 weeks, when the structure of the brain is formed. Repeated ultrasound at 24-28 weeks notes a decrease in the number of cystic cavities.
Choroid plexus cyst in the fetus - what is it?
CSS is dangerous in children with chromosomal abnormalities such as Edwards disease (trisomy 18). The nosology is characterized by multiple malformations, so intracerebral cavities with cerebrospinal fluid are a minimal problem in treatment.
Down's disease is not characterized by the formation of the cerebral coronary artery system.
Interesting facts about choroid plexus cysts in children:
- Spontaneous disappearance in 90% of fetuses by 28 weeks of development;
- The prevalence rate of nosology among pregnant women is 2%;
- The shape, size, number of cavities varies;
- Found in adults and healthy people;
- The frequency of villous and choroid plexus cysts is about 3%.
It is impossible to determine the initial type of formations in the fetus due to physiological degradation. The absence of pronounced symptoms does not allow doctors to accumulate enough information about the pathology.
Morphological structure of choroid cystic cavities in a child
The accumulation of cerebrospinal fluid inside the choroidal formations does not pose a threat to the health of the baby. Morphologically, the cavity is represented by a thin wall, capable of changing size and shape.
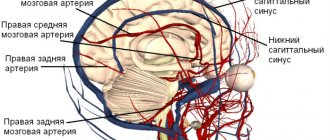
Vascular plexuses are early structures in the formation of the central nervous system of the fetus. Bilateral localization is due to the presence of two hemispheres that require the content of cerebrospinal fluid. Scientists were unable to explain the need for the formation of limited cavities around the plexuses. Presumably, the structures are part of the formation of the central nervous system, and therefore disappear by 28 weeks. If development slows down, CSS can be observed in newborns, infants 3 months and somewhat older.
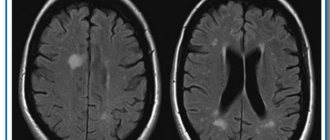
Cystic cavities of the brain are sometimes observed in adults. The pathology does not produce clinical symptoms, so they are detected by chance on an MRI performed due to the verification of another etiology.
Practice shows that there is no health hazard in the persistence of choroid plexus cysts after 30 weeks, with the exception of Edwards disease.
Screening for detection of congenital fetal diseases during pregnancy
Category: Reminders for the public.
Screening during pregnancy is a whole range of studies that allows parents and doctors to obtain the most complete information about the health of their unborn baby. Screening reveals many congenital and physical characteristics. How and when is screening done during pregnancy?
What is screening during pregnancy and why is it done?
Screening during pregnancy is a set of examinations that includes ultrasound and biochemical analysis of venous blood for hormones. As a rule, screening is carried out three times - in the first, second and third trimester.
Early detection of pathologies is very important. This makes it possible to begin treatment of genetic diseases as early as possible and, if not completely cure them, then at least relieve the symptoms as much as possible. If during the examination the doctor notices any abnormalities, the pregnancy is monitored especially carefully, which makes it possible to prevent the development of complications or premature birth. If the detected pathologies turn out to be too severe and incompatible with life, the doctor will refer the patient to terminate the pregnancy for medical reasons.
Screening during pregnancy is harmless for both mother and baby. This is a fairly accurate study, although it should be clearly understood that it does not provide a 100% guarantee. The accuracy of screening depends on many factors - the professionalism of the researchers, the woman’s compliance with the rules for preparing for the examination, and other factors.
First screening during pregnancy
The first screening during pregnancy is carried out between the 11th and 13th weeks. There is no point in undergoing this examination earlier - until the 11th week of pregnancy, many indicators are practically impossible to determine.
The study includes two medical tests - an ultrasound and a blood test.
Ultrasound
Using an ultrasound, the doctor determines the exact duration of pregnancy, evaluates the child’s physique, its size (head circumference, length of limbs, height), the functioning of the heart muscle, the symmetry of the brain, the volume of amniotic fluid, the structure and size of the placenta, as well as the condition and tone of the uterus. For each of these parameters there are normal indicators with which the doctor will compare the results. For an 11-13 week pregnancy these norms are:
- CTP (coccygeal-parietal size, that is, the length of the fetus from the crown to the coccyx) is 43–65 mm. If this figure is higher than normal, it means the child will be large. A deviation to the smaller side indicates slow development (the reason for this state of affairs is often a hormonal imbalance or infectious diseases suffered by the expectant mother), genetic pathologies or fetal death (in this case the heart will not be heard). However, this may also be due to a banal error in determining the timing of pregnancy.
- BDP (biparietal size, that is, the distance from temple to temple) - 17–24 mm. A high BDP means a large fetus, but only if all other indicators indicate the same. Otherwise, we may be talking about a brain hernia or hydrocephalus. A low BDP indicates slow brain development.
- TVP (thickness of the collar space) - 1.6–1.7 mm. Deviation from this norm (TVP above 3 mm) is considered a sign of some severe chromosomal pathologies - Down syndrome, Edwards syndrome, etc. However, one should not panic ahead of time - no one will make such a serious diagnosis only on the basis of TVP. To confirm, you need to take a blood test for hormones and do a biopsy of the outer dense membrane of the embryo for subsequent research.
The length of the nasal bone is 2–4.2 mm. A nasal bone that is too small may indicate a pathology or simply that the baby will have a snub nose. HR (heart rate) - 140–160 beats per minute. A slight (up to 40 beats per minute) deviation in one direction or another is considered normal.
The size of the chorion, amnion and yolk sac. The chorion is the outer membrane of the fetus, which will eventually become the placenta. If it is located on the lower wall of the uterus, they speak of chorion presentation. This is a potentially dangerous situation that can lead to miscarriage, in which case bed rest is recommended for the pregnant woman.
Amnion is the inner membrane that holds amniotic fluid. The normal volume of amniotic fluid at 11–13 weeks is 50–100 ml.
The yolk sac is an embryonic organ that, in the first weeks of the fetus’s life, plays the role of some internal organs that will be formed later. By the time of the first screening, the yolk sac should practically disappear (then the examination form will indicate “not visualized”). If its size is about 6 mm, then the fetus may have certain pathologies.
Cervix. Normally, its length at the time of the first screening is 35–40 mm. A shorter cervix means a risk of premature birth.
Ultrasound is performed in two ways - transabdominal, in which the ultrasound machine sensor is located on the abdomen, and transvaginal, in which it is inserted into the vagina. Transvaginal ultrasound provides more complete and accurate information, but is usually performed only in the first trimester. This method is usually used when examining overweight women, since the fat layer in the abdominal area does not allow a detailed examination of the fetus and uterus.
It is necessary to prepare accordingly for an ultrasound. Before a transabdominal ultrasound, it is advised to drink about a liter of water so that at the time of the examination the bladder is full - then the uterus will shift slightly towards the abdomen and the picture will be clearer. With a transvaginal ultrasound, the degree of bladder fullness does not matter at all, but before the examination it is better to go to the toilet - it will be more comfortable. Before the examination, you need to take a shower or freshen up with wet wipes. The accumulation of gases can distort the results of ultrasound, no matter what method it is performed. Therefore, expectant mothers suffering from flatulence are advised to take anti-flatulence medications the day before the examination and not eat anything that produces gas.
Blood analysis
Biochemical screening, also called a dual test, is done to determine the level of two hormones (hence the name) - free b-hCG and PAPP-A.
- b-hCG (human chorionic gonadotropin) begins to be produced from the first days of pregnancy. Its amount gradually increases until about the 9th week, and then begins to gradually decrease. On average, for a period of 11–13 weeks, 50,000–55,000 mIU/ml is considered normal. An elevated level of hCG may indicate a multiple pregnancy, or, in the worst case, genetic pathologies of the fetus or the presence of diabetes mellitus in the mother. Reduced hCG is typical for frozen pregnancy, ectopic pregnancy, fetal death, or certain malformations (Patau syndrome and Edwards syndrome).
- PAPP-A is plasma protein A. The maintenance norm for a period of 11–13 weeks is 0.79–6.01 mU/l. Low PAPP-A is a sign of chromosomal pathologies such as Down syndrome and Edwards syndrome, fetal death and miscarriage, fetal malnutrition (underweight) and preeclampsia.
- High PAPP-A is a sign of multiple pregnancy, large fetal size or low placenta.
In order for the blood test to provide the most accurate information, it must be taken on an empty stomach, at least 8 hours after the last meal. 2-3 days before the test, you should refrain from fried, fatty, spicy, smoked foods, chocolate, nuts, and seafood. It is also recommended not to have sexual intercourse. All this is not so significant, but it can affect the result in one way or another.
Second screening during pregnancy
The second screening during pregnancy is carried out at 16–20 weeks. Like the first one, it consists of the same two stages - ultrasound and blood tests.
Ultrasound
This time, the doctor determines not only the size, but also the position of the fetus and its bone structure, the condition of the internal organs and the place of attachment of the umbilical cord, as well as the volume of amniotic fluid. Here are the approximate basic indicators of the norm for a period of 16–20 weeks:
- BPR - 26–56 mm.
- DBC (femur length) - 13–38 mm.
- KDP (humerus length) - 13–36 mm.
- OG (head circumference) - 112–186 mm.
AFI (amniotic fluid index, that is, the volume of amniotic fluid) - 73–230 mm. Oligohydramnios can negatively affect the condition of the child’s bone structure and the development of his nervous system.
Localization of the placenta. There is some risk only when the placenta is located on the anterior wall of the uterus - with such a localization, placental abruption is possible.
Umbilical cord. One of the most important parameters is the location of the umbilical cord attachment. Marginal, split or membrane attachment is fraught with fetal hypoxia and difficulties during childbirth; it often becomes an indication for cesarean section. The umbilical cord is supplied by 2 arteries and 1 vein, although sometimes only one artery is present. This can cause fetal hypoxia, heart defects, disturbances in the child’s cardiovascular system, and cause low body weight in the baby. However, if all other tests and examinations do not show deviations from the norm, there is no need to worry.
Cervix. The length of the cervix at this stage should be 40–45 mm. A short cervix means a risk of miscarriage.
Visualization. Unsatisfactory visualization can be caused both by the position of the fetus or the excess weight of the expectant mother, as well as by edema or hypertonicity of the uterus.
Blood analysis
As during the first screening, during the second a blood test is taken for b-hCG, and the level of free estriol and AFP is also checked. Here are the norms for their maintenance at 16-20 weeks of pregnancy:
- b-hCG - 4.67-5-27 ng/ml.
- Free estriol is a hormone, the level of which can be used to judge the condition of the placenta. The normal range is 1.17–3.8 ng/ml. Elevated estriol is typical for multiple pregnancies or a large fetus. Reduced - for the threat of miscarriage, placental insufficiency, anencephaly and Down syndrome.
- AFP is a protein produced in the fetal gastrointestinal tract. The norm is 15–27 U/ml. A slightly lower AFP may mean that the gestational age was determined incorrectly (slightly underestimated). If the AFP is very low, the cause may be Edwards or Down syndrome, the threat of miscarriage or fetal death. High AFP is characteristic of neural tube pathologies, esophageal atresia, and Meckel's syndrome. High AFP is also possible in women who have had an infectious disease during pregnancy.
Third screening during pregnancy
The third screening during pregnancy is carried out at 30-43 weeks. Based on the results of this screening, the doctor decides on the need for a cesarean section or the possibility of a natural birth. The basis of the third screening is the same ultrasound. Sometimes Doppler sonography is prescribed - a study of the functioning of blood vessels. Here are the approximate norms for this stage of pregnancy:
Ultrasound
- BPR - 67–91 mm
- DBK - 47–71 mm
- WPC - 44–63 mm
- Exhaust gas - 238–336 mm
- IAZh - 82-278 mm
The thickness of the placenta is 23.9–43.8. A placenta that is too thin is not a particularly dangerous deviation from the norm. The reason may be the woman’s miniature physique, infectious diseases she has suffered, or hypertension. An excessively thick placenta is a sign of anemia, diabetes, and Rh conflict. An indicator such as the degree of maturity of the placenta is also taken into account - at a period of 30–35 weeks, the 1st degree of maturity is considered normal. If the placenta thickens and ages too quickly, premature birth, fetal hypoxia and slow development are possible.
Prenatal screening is very important and should not be neglected. Timely identified pathologies and deviations from the norm can save the life and health of your child. This is worth remembering, especially for those parents who refuse an examination for fear of finding out that the baby’s development is not going according to plan.
Causes of CSS
The etiology has not been established. It is considered likely that cystic cavities will persist for a long time against the background of viral infections, herpes, or complicated pregnancy. The absence of clinical manifestations until the end of a person’s life indicates the absence of harm from the pathology. The formations require dynamic monitoring. Blind fontanelles in a child allow an ultrasound of the skull to be performed, and periodic MRI is recommended for adults.
Viral cysts can change: they grow, they degenerate. Dynamic observation determines the prognosis of consequences for a person with CSS.
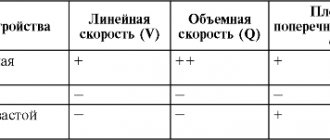
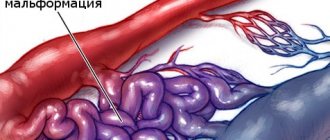
Two different diagnoses should be distinguished: “fetal choroid plexus cyst” and “cerebral vascular cyst”. The first nosology is harmless, goes away on its own or persists without dynamics for many years. The second type is dangerous, as it sometimes provokes symptoms.
There is a definition of “pseudocyst”. On the screen of an ultrasound monitor, doctors can detect a cavity formed by physiological structures.
The exclusion of pathological conditions after the diagnosis of “choroid plexus cyst” in a newborn and fetus is ensured by an additional comprehensive examination. Genetic counseling rules out Edwards disease. Magnetic resonance imaging shows the structure of the soft tissues of the brain with high resolution, three-dimensional modeling of the area under study.
Detection of a choroid plexus cyst in a child requires verification of provoking factors: viral and bacterial infections, changes in the composition of the cerebrospinal fluid, increased intracranial pressure. If there are no additional changes, it can be argued that there are no conditions for the negative development of a vascular cyst.
Treatment
Not required in 95-98% of cases. Only monitoring of the child's condition is indicated.
If clinical manifestations occur, medications may be prescribed:
- Antiviral agents – for laboratory-confirmed herpes virus (Acyclovir).
- Drugs that reduce intracranial pressure (diuretics) – if signs of hydrocephalus occur (Spironolactone).
- Anticonvulsants - they are prescribed not only when an epileptic focus has formed in the brain, but also when there is pronounced activity of the neural network (pre-epileptic state).
- Weak sedatives – for increased excitability (Glycine).
- Antioxidant complexes and nootropics - to restore metabolic processes in the brain and normalize blood circulation.
All these groups of drugs are used only to eliminate symptoms.
Choroid plexus cysts of a newborn baby
Detection of CSS after birth is not a dangerous condition, but requires examination of the newborn baby. Herpetic infection is activated when the immune system is weakened and can cause changes in the choroid plexus. As the baby grows, the immune system strengthens, so after 3 months, active development of immunity is observed. A decrease in viral activity stabilizes the condition. Cystic cavities can be observed in infants in the absence of clinical pathology. According to the standard scheme, children are examined three times:
- 3 months;
- 6 months;
- 12 months.
The absence of progression indicates the absence of changes that will contribute to the development of dangerous conditions.
Left choroid plexus cyst in a child
The choroid plexus is formed in the fetal body quite early. Education takes part in the formation of cerebrospinal fluid, which provides nutrition to the brain.
The diagnosis of left plexus cyst is common in newborns, although bilateral localization is more common. Pathology develops before the age of 1 year, when intrauterine infections are present. Cystic cavities are equally likely to form in any part of the brain.
Choroid plexus cyst of the right lateral ventricle
The nosology is considered the most benign, since most variants disappear on their own. Found after 22 weeks. An ultrasound scan after 28 weeks shows no pathology. The cystic cavity of the right ventricle can resolve. If there is no associated pathology (with damage to other ventricular spaces), this location of the cyst will not cause complications throughout life, even if the nosology persists in the child after 1 year. In adults, the nosology is rare.
Bilateral choroid plexus cysts
The pathology can persist into adulthood. Some cavities disappear, some remain. Despite the bilateral location, no clinical symptoms occur. Dynamic observation can reveal an increase in size and a change in shape. Only then is conservative treatment carried out. Chromosome mutations are preliminarily excluded. Geneticists can identify a genetic predisposition to Edwards disease. True, pathology can be determined without consulting on the external symptoms of the nosology, characterized by multiple malformations.
Ultrasound examination every 3 months allows you to monitor the condition of the brain parenchyma in infants. The procedure is sufficient to obtain information about the degradation or progression of cystic cavities.
Small cystic cavities in a child's brain
The nature of the CSS has not been reliably established. The pathology is an incidental finding. Small lesions do not affect the human psyche or metabolic reactions. There is no metabolic disorder, so there is no danger.
Small plexus and vascular cysts should be differentiated. The latter option provokes some symptoms. There is no threat to life or health. In adults, minor hemorrhages may occur, soaking into surrounding tissues.
Intrauterine infection provokes inflammatory damage to the walls of the cavity. Detection of infection requires the prescription of antibacterial drugs.
Detection of a plexus cyst at 19 or 20 weeks is not a reason for parents to worry. A repeat examination at week 29 will show no cavities.
Most scientists consider a cystic plexus of intracerebral vessels to be normal. The absence of a clinic suggests that the nosology is a variant of the norm. Improvements in diagnostic methods have made it possible to detect the disease in fetuses and infants more often.
You should pay attention to late cyst formation, which is the result of infection with herpes and a number of other viruses.
Prevention measures
Since the reasons for the formation of CSS are not known for certain, and such a cyst itself is not considered a pathology, there are no specific preventive measures. A woman is recommended to lead a healthy lifestyle, eat properly and nutritiously, walk in the fresh air, do gymnastics for pregnant women and do breathing exercises, and take complex vitamin preparations as prescribed by a doctor.
Particular attention should be paid to protection against all kinds of infections. You should not visit crowded places, especially during the seasonal rise in the incidence of ARVI and influenza. In intimate life, it makes sense to use a condom.
Symptoms of choroid plexus cysts
A brain cyst in adults can be a consequence of a hematoma. Limited accumulation of blood (subdural, epidural) with penetration into the ventricles of the brain contributes to ventricular cyst formation.
Pathology contributes to the appearance of clinical symptoms:
- Dizziness, headache;
- Movement coordination disorder;
- Muscle cramps, epilepsy;
- Hypertonicity in newborns.
Localization of manifestations near important nerve centers contributes to the emergence of specific symptoms.
The presence of cytomegalovirus or herpetic infection complicates the course of the disease. Detection of a pathogen and CSS in an adult with a high degree of probability indicates a viral etiology of cystic cavities.
Microcyst of the choroid plexus of the right lateral ventricle rarely causes neurological disorders.
In children, vascular microcysts and larger formations are not accompanied by pathological symptoms. The International Classification of Diseases (ICD 10) does not classify nosology as a number of pathological conditions.
Complications
According to statistics, plexus cysts, as a rule, do not cause problems associated with the development of the child. However, cases have been identified indicating serious genetic abnormalities due to the formation of cystic growths. It could be Edwards or Down syndrome.
Pseudocysts with these syndromes do not have a constant relationship. In addition, such a phenomenon does not always indicate the presence of deviations.
After birth, the presence of a cyst may sometimes cause the baby to experience headaches.
If, under the influence of certain processes, degeneration into cancer occurs, then there may be more serious consequences.
Consequences of choroid plexus cysts
Complicated cystic formations cause specific manifestations:
- Hypertonicity of newborns;
- Neurological symptoms due to compression of brain structures;
- Epilepsy (muscle cramps);
- Slight loss of vision and hearing.
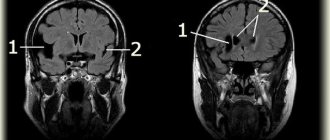
Magnetic resonance imaging will need to distinguish a true vascular cyst from a pseudocyst. The latter type is a variant of the physiological development of the brain, but the anatomical structure when examined by ultrasound resembles a cavity. Magnetic resonance imaging is an accurate study (informativeness is about 96%). The three-dimensional modeling mode will allow you to correctly verify the nosology.
Edwards syndrome can be detected by ultrasound by identifying abnormalities of the limbs and changes in internal organs. Additional diagnostic tests:
- Determination of the concentration of human chorionic gonadotropin;
- Blood chemistry;
- Analysis of amniotic fluid.
A special risk group is women aged 32 years and older with hormonal disorders.
Diagnostic measures
Today, a vascular cyst is not a sign of the disease, but it can increase the risk of developing other pathologies.
For early detection of abnormalities in fetal development, all pregnant women must undergo ultrasound diagnostics
Diagnosis of cystic formation using special research methods:
- Ultrasound diagnostics. It is carried out during the intrauterine life of the fetus, which makes it possible to identify the formation at an early stage of its development.
- Biopsy of the placenta. At high risk of developing trisomy 18.
- Amniocentesis. It is highly accurate and is performed up to 22 weeks of pregnancy. The technique consists of studying the skin cells of the embryo.
- Neurosonography. It is carried out in children under one year of age. The procedure allows you to identify a tumor on both sides, but before the anterior fontanelle closes.
- Magnetic resonance imaging. It is used in adults to determine possible neurological disorders, during which cysts can be detected.