Dysplastic cardiopathy (DCP), an abnormal or accessory chord in the left ventricle - when faced with these terms, many parents begin to think that the child has a heart defect. The KinderKlinik pediatrician will tell you whether this condition poses any threat to the child’s life, whether the child needs to be limited in the level of physical activity and how often it is necessary to undergo preventive examinations.
What is a chord: location and functions
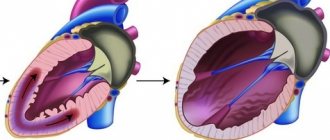
For normal heart function, it is important that during ventricular systole the communication with the atria is completely blocked. This is ensured by two valves:
- right tricuspid;
- left (also called mitral) - bicuspid.
Fleshy trabeculae are attached to the valve flaps, as well as chordae tendineae (cords, heart strings) , formed by dense connective tissue and extending from the papillary muscles. Nature “invented” these structures in order to hold the valve flaps:
- when the cords contract, the valves open;
- at the moment of relaxation of the strings, the valves close tightly, creating a barrier to blood entering the atria.
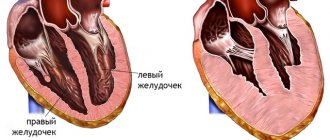
Sometimes during intrauterine development additional, “extra” fibers are formed. They can be found on both the right and left, but in 90% of cases the left ventricle “suffers.” If such a string goes from the papillary muscles to the walls of the heart or sags freely, cardiologists call it a false chord of the left ventricle (LVF). If it is directed from one wall of the ventricle to another, then such a fiber is called an abnormal cord (ATLV).
The LVDC differs from the mitral valve support string:
- shorter length and thickness;
- structural organization.
A normal, typical fiber is characterized by one central core, in which up to 5 main blood vessels pass. The false chord of the left ventricle is formed by 2–3 rods, separated by connective tissue, inside of which there are microvasculature vessels.
You can also find the following formulation: “additional trabecula of the left ventricle.” Doctors often mean LVDC in this case, although, from an anatomical point of view, the trabecula is a separate structure that continues the cardiac string.
In the English-language medical literature, the term falshe-chordae is used - “false chord”. Some authors recommend replacing the literal translation with “ectopically attached notochord”, as it more accurately reflects the essence of the changes.
Reasons for the development of the anomaly
The main etiological factor in the occurrence of such an anomaly as an additional chord in the heart of a child is genetic predisposition. The risk increases if the mother has cardiac pathology. But experts do not exclude other reasons for the development of small cardiac anomalies:
- consumption of alcoholic beverages;
- smoking;
- viral and bacterial infections;
- stress;
- excessive physical activity;
- malnutrition;
- environmental pollution;
- radiation.
An abnormality of connective tissue is closely related to its dysplasia. The formation of the fetal cardiovascular system ends by the eighth week of intrauterine development. Obstetricians and gynecologists know that the blood of the unborn child circulates independently already on the 26th day of pregnancy, heart valves are formed at the 6th week, therefore it is in the first trimester that a woman needs to be especially careful about adverse effects.
Lifestyle with pathology
A child diagnosed with LVDC is not sick. He can lead a normal life according to his age. The disease prohibits professional participation in sports that involve heavy physical activity. To avoid complications, you must adhere to the following rules:
- A clear daily routine that balances work and rest time.
- Sleep at least eight hours a day.
- Adhere to the principles of proper nutrition.
- Eliminate fatty, fried foods, spices, spices, and fast food from your diet.
- Regularly perform therapeutic exercises and harden.
- Avoid psycho-emotional overload.
- Do not do heavy physical work.
- Take a course of restorative massage annually.
- Do not self-medicate.
- Visit a cardiologist regularly.
For sports activities, a child who has an additional chord in the left ventricle of the heart is allowed to:
- Left ventricular hypertrophy on the ECG: recommendations from a cardiologist
- athletics (amateur sports);
- exercises using the Swedish wall;
- ballroom dancing;
- medium-long distance hiking trips.
Children with LVDC are prohibited from:
- skydive;
- go diving;
- visit the panic room;
- any extreme entertainment.
Attention!
The presence of an additional chord in the left ventricle cannot be a medical disqualification from military service. Young people who have been diagnosed with serious complications of the disease will not be subject to conscription. During the physiological course of pregnancy, a woman can give birth on her own.
Symptoms and indications for visiting a doctor
Pediatric cardiologists divide LVDC into those that are hemodynamically significant and those that do not affect health and quality of life. In the vast majority of cases, parents are unaware of the existing anomaly - the child develops absolutely normally.
The clinical picture of LVDC does not have specific signs. Sometimes, even in the neonatal period, a murmur is diagnosed - an acoustic phenomenon in the form of a whistle or creaking, which the doctor hears when listening to the heart. The cause of the noise is the sounds of turbulence as blood moves in the left ventricle or the vibration of an additional heart string.
The manifestation of LVAC is determined by its intracardiac topography and the period of a person’s life. During the so-called growth spurts, when there is an increased increase in body length, children have complaints about:
- excessive fatigue;
- unmotivated fatigue;
- pale skin;
- periodic increased heart rate;
- pain in the area of the projection of the apex of the heart;
- feeling of lack of air.
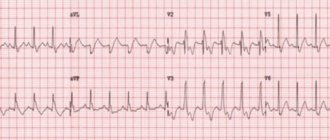
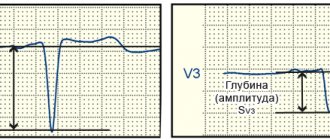
An electrocardiographic examination can reveal the presence of extrasystoles, conduction disturbances, and signs of left ventricular myocardial hypertrophy. If the occurrence of a minor cardiac anomaly is caused by connective tissue dysplasia syndrome, LVDC is accompanied by the following symptoms:
- asthenic physique;
- low body mass index;
- joint hypermobility;
- history of dislocations;
- deformation of the chest bones;
- poor posture;
- structural changes in internal organs.
Symptoms of LVDC often appear during adolescence. Parents may attribute the teenager’s complaints to the difficulties of the school curriculum, overwork with tutors, overload in the sports section, and prolonged sitting at the computer.
Symptoms
As is clear from the general situation, the clinical picture of an additional chord is absent in most cases.
The patient is unaware of the problem in 90% of situations or even more. That's why he doesn't go to doctors.
Deviations can be detected only by echocardiography results, and that is, by taking a closer look. Only in 10% of situations are there any signs of impairment.
Among them:
- Chest pain. Weak or medium in intensity. They are localized on the left side and can radiate to the shoulder blade, arm, or face. However, not always.
As a rule, they occur after physical activity. They pass at rest. The character is burning, pressing, bursting.
The sign indicates the onset of ischemic processes and becomes more and more distinct as cardiac dysfunction progresses.
- Arrhythmias. Like sudden onset tachycardia. The disturbance is especially noticeable when the load on the body increases. For example, after a brisk walk, climbing stairs, playing sports, even eating.
Suddenly the contraction frequency increases, reaching more than 90 beats per minute.
There may be a feeling of interruptions. Patients describe the condition as “the heart suddenly stops and starts beating again” or “misses contractions.”
These are the phenomena of extrasystole. In some cases, the arrhythmia is represented by paroxysmal (attack-like) tachycardia. There are many options.
- Shortness of breath due to physical activity. For many years, the deviation manifests itself externally as exercise intolerance. The patient cannot walk quickly or play sports. Sometimes the threshold when a symptom arises is so great that a person simply does not reach it. This means that the sign goes unnoticed. Unless the athlete has an extra chord.
- Weakness, drowsiness. Unreasonable lethargy and low performance. As cardiac dysfunction progresses, signs of asthenia become more pronounced. But this takes years.
- Headache, inability to navigate in space. The result of insufficient blood circulation in the brain. Fortunately, the sign does not support critical processes. In addition, other neurological deficits are also detected: problems with intelligence, thinking, memory, decreased visual acuity, and hearing. There are many options.
Clinically, an extra chord corresponds to heart failure and provokes it.
The rate of disease progression is low, extremely insignificant in the majority of cases.
At some point, decompensation may occur. The body will not be able to maintain acceptable functional activity of the heart. The process will begin to develop like an avalanche and lead to disaster.
Fortunately, this is unlikely. Because symptoms will force a person to see a doctor much earlier. In childhood, there are usually no signs.
Manifestation occurs at ages over 15-16 years. It is during this period that subcompensation occurs. The body still supports and stabilizes the functioning of the muscular organ, but it is no longer fully capable.
Diagnostics: how to determine LVHL
When the doctor tells you that your baby has a heart murmur, there is no reason to panic. The condition does not require emergency resuscitation measures or intensive treatment. The main diagnostic method is ultrasound examination. It will help clarify the location and number of additional strands. There are the following types of LVDC:
- according to location in the ventricle - apical, middle, basal;
- in relation to the axis of the heart - diagonal, longitudinal, transverse;
- by number - singular and plural.
If echocardiography has revealed an additional chord in the cavity of the left ventricle in a child of any age, I advise parents to undergo the following examinations:
- A general blood test is not important in terms of diagnosing LVHL, but it will reveal anemia or an existing inflammatory process in the body, which can aggravate the condition of a child with a minor cardiac anomaly.
- Electrocardiography. It is advisable to conduct Holter monitoring, which will exclude arrhythmia with greater diagnostic accuracy.
- ECG tests with physical activity will show how well the child’s heart “copes” with its function.
- Consultations with specialized specialists (orthopedist, endocrinologist, otolaryngologist).
I always explain to parents of infants that sometimes the abnormal chord can lengthen and “grow” into the valve, so during subsequent ultrasounds the doctor does not detect LVDC. In such cases, they say that the baby has “outgrown” this pathology.
Is it possible to recognize the pathology on your own?
In the absence of abnormal development of the right ventricle, the additional chord of the left ventricle does not produce significant clinical symptoms and for a long time proceeds without any pronounced signs and symptoms. During the first year of life, pathology is detected by chance during an electrocardiogram and ultrasound of the heart in children who are at risk for the development of cardiovascular diseases, as well as those who have signs of cyanosis - blue discoloration of the nasolabial triangle .
Blue lips in a child
Signs of LVDC in children of the younger age group (from 3 to 6-7 years) may include:
- tall height and thin physique (subject to a balanced and regular diet);
- deformation of bone tissue (hip dysplasia, scoliosis);
- increased mobility of the knee and elbow joints;
- myopia of varying degrees and other types of ametropia (the child squints, trying to see objects located at a great distance from him);
- pathological mobility of the kidneys against the background of their displacement or prolapse (nephroptosis);
- poor digestion.
Older children attending educational institutions may complain of increased fatigue, drowsiness, poor memory, and decreased concentration. During physical education they may experience shortness of breath or mild tachycardia.
Drowsiness is one of the possible symptoms
Note! Children with LVDC at any age are characterized by emotional lability, so frequent changes in mood during the day, which last for a long time, should be a reason to contact a specialist.
Doctor's advice: how often to do echocardiography with false chord
For a standard check-up for a minor cardiac anomaly, it is enough to undergo an echocardiography once a year. The examination is scheduled unscheduled if:
- the patient has complaints, including those not directly related to cardiology;
- you notice that the child is growing rapidly;
- there was a sharp weight loss;
- a chronic disease has been diagnosed, such as asthma, gastritis, nephritis;
- the child goes to kindergarten, school, university;
- there is a question about the sports section;
- stress occurred: an exam, the loss of one of the family members, conflict in the children's team and at home;
- pregnancy is planned or determined.
Single LVDC is not considered a pathology. Experts consider them as an anatomical feature of a person. The presence of an additional chord is not a contraindication to attending physical education classes. Young men with abnormal cords can be drafted into the army if they do not have complications or concomitant pathologies. It is only important to clearly tell the child about his condition and warn him that he needs to be attentive to his health.
What complications can occur with a false chord?
The prognosis for single abnormal chords is favorable. Complications are rare, but multiple transverse and diagonal chordae can act as a trigger for the development of diastolic dysfunction of the heart, increasing the risk of thrombus formation, bacterial endocarditis, and can also be combined with other congenital anomalies.
Sometimes LVHL can cause:
- extrasystoles;
- paroxysmal ventricular tachycardia;
- WPW syndrome;
- atrial fibrillation;
- TELA;
- thrombotic lesions of veins;
- ischemic stroke;
- cardiac arrest.
These disorders are observed in adulthood, but a teenager with LVDC should be informed about them. An unfavorable prognosis is characteristic only of non-compact left ventricular myocardium syndrome (LVSM), which is characterized by the presence of numerous additional trabeculae and chordae, combined with changes in the structure of the heart muscle.
Despite these complications, statistics claim: repeated clinical observations have not revealed a relationship between the presence of additional strands in the left ventricle and the risk of cardiovascular mortality.
Treatment
As a rule, single LVDC without clinical manifestations do not require treatment. Medicines are prescribed for the development of complications and concomitant heart pathologies. Symptomatic therapy - antiarrhythmic drugs and substances that correct hemodynamics: diuretics, antihypertensives, antioxidants, potassium and magnesium preparations.
Surgical treatment methods (local cryodestruction and excision of left ventricular ventricle) are rarely used: if an abnormal cord causes arrhythmia that threatens the patient’s life.
Lifestyle recommendations:
- give up fast food and sugary carbonated drinks;
- spend at least an hour a day in the fresh air;
- do not sit too long at the computer;
- find time in your personal schedule for physical exercise;
- learn to cope with stress;
- get vaccinated against influenza and other infectious diseases in a timely manner;
It is imperative to discuss the issue of “bad habits” with your teenager. It is important that the young person consciously considers it unacceptable for himself to take a sip of a low-alcohol drink or inhale cigarette smoke.
Pregnancy is not contraindicated for women with LVDC. It does not pose a threat to health, passes without negative consequences for mother and child, you just need to notify the doctor about the existing additional chord.
Forecast
In most cases - favorable. Even when symptoms develop, many years pass before the process reaches a critical, decompensated phase.
This can only be achieved consciously. Typically, symptoms in the earlier stages are unbearable and significantly reduce the quality of life. There is no choice but to see a doctor.
The survival rate is good, the likelihood of maintaining working capacity is also good. But this does not mean that you need to sit idly by. You cannot do without the consultation and help of a cardiologist.