Bisoprolol is a 2nd generation beta-blocker. It is actively used in the monotherapy of hypertension and the treatment of heart failure. This drug is also used in complex therapy when taken simultaneously with ACE inhibitors, angiotensin antagonists and calcium antagonists.
It is also often prescribed with specific drugs from the cardiological group. Available in tablet form. But this particular drug is not always suitable, there is a particular intolerance to its main component, and it is a substance of the same name, so you have to select analogues.
Bisoprolol is prescribed to patients who have been diagnosed with:
- IHD;
- myocardial infarction;
- chronic form of heart failure;
- glaucoma;
- tachyarrhythmia.
According to reviews from specialists who have been monitoring the health of patients taking Bisoprolol for many years, the drug quickly and easily reduces blood pressure. But it has a bad effect on your heart rate during exercise.
Bisoprolol is an inexpensive but effective drug in tablets that has the following actions:
- significantly reduces cardiac output and heart rate;
- suppresses the secretion of renin, due to which a decrease in blood pressure occurs;
- causes a decrease in peripheral resistance of blood vessels and expansion of their walls, which allows to further reduce pressure;
- eye pressure also has a positive effect, normalizing it without reducing visual acuity;
- provokes contraction of the smooth muscles of internal organs.
Bisoprolol analogues in tablets without side effects are needed for those who, after starting to take the medication, experience undesirable symptoms, manifested in the form of such conditions:
- digestive disorders;
- reducing blood pressure levels;
- insomnia;
- fatigue;
- depressive disorders;
- headache;
- memory and vision impairment;
- exacerbation of asthma.
As for contraindications, Bisoprolol is contraindicated for use if the patient has:
- special intolerance to the active component or additional ones;
- acute heart failure or chronic decompensation;
- cardiogenic shock;
- sick sinus syndrome;
- sinoarterial blockade;
- bradycardia;
- chronic decrease in blood pressure;
- severe course of bronchial asthma;
- metabolic acidosis.
A specialist should select an analogue, even if it has no contraindications or undesirable manifestations. Self-medication can lead to serious complications.
Instructions for use of "Bisoprolol"
β-adrenergic receptor blockers (β1-AR) are a large group of drugs that competitively and selectively inhibit the binding of catecholamines to the corresponding receptors.
The latter are proteins of the outer cell membrane that “recognize” and connect the molecules of adrenaline and norepinephrine circulating in the blood. β1-AR are localized on the membrane of the fibers of cardiomyocytes, kidney cells and adipose tissue. The effect on the structures causes an acceleration of the pulse and increased heart contractions, stimulates glycogenolysis (the breakdown of complex carbohydrates) in the liver, and relaxation of the vascular wall of the arteries.
"Bisoprolol" is a new generation drug that dissolves in blood plasma and fat cells of tissues. Excretion of active metabolic products is carried out in two ways: renal excretion and elimination with bile into the intestine.
This feature is one of the advantages of the drug, which allows Bisoprolol to be prescribed to patients with chronic kidney or liver diseases and elderly people. The drug is considered safe for use by patients with type 2 diabetes, as it does not affect carbohydrate and lipid metabolism.
Pharmacokinetic properties:
- More than 90% of the active component is absorbed from the intestinal cavity;
- connection with blood plasma proteins – 28-32%;
- adsorption and bioavailability are independent of food consumption;
- the drug begins to act after 3-4 hours;
- The therapeutic maximum is reached after 10-12 hours and lasts more than a day.
Indications for use
"Bisoprolol" is used in the clinical practice of cardiologists, therapists and endocrinologists. The most common indications for taking the drug:
- hypertension (essential and symptomatic);
- acute and chronic forms of IHD (angina pectoris, myocardial infarction (MI), cardiosclerosis);
- chronic heart failure (CHF) with left ventricular systolic dysfunction (reduced ejection fraction);
- symptomatic treatment of thyrotoxicosis – a pathology with increased synthesis of thyroid hormones;
- hypertrophic cardiomyopathy;
- permanent form of atrial fibrillation, supraventricular (supraventricular) tachycardia.
The goals of prescribing Bisoprolol for acute MI on the first day:
- pain relief;
- limiting the area of necrosis in the muscle;
- prevention of severe arrhythmias;
- reducing the risk of death.
BBs reduce mortality in chronic heart failure and prevent complications from the circulatory system during surgical interventions (coronary artery stenting, bypass surgery).
Mechanism of action
The active substance binds to β-AR and prevents the interaction of catecholamines and the occurrence of cellular reactions. Bisoprolol is a cardioselective drug that selectively blocks β1-adrenergic receptors located in the heart and does not affect the structures of the lung tissue.
The pharmacological effects of the drug are presented in the table.
| Structure | Influence |
| Myocardium (muscular lining of the heart) |
|
| Conducting system |
|
| Coronary vessels |
|
| Kidneys |
|
Consequences of using Bisoprolol:
- reducing energy costs during tachycardia, sympathicotonia - conditions with increased stimulation of adrenergic receptors;
- correction of pathological remodeling (changes in structure) of the myocardium;
- delay or slowdown of cardiac functional failure due to dysfunction of beta-adrenergic receptors;
- decreased sensitivity to adrenaline with a progressive decline in the contractile function of cardiomyocytes.
Composition and release form
The drug is produced in the form of flat white tablets with a beveled edge. The concentration of the active substance (bisoprolol fumarate) ranges from 2.5 to 10 mg, depending on the chosen dosage. There is a dividing strip on the surface of the tablet, which indicates an equal amount of the drug in each half.
The cardboard packaging contains 2-5 blisters with tablets of 10 pieces, instructions for use of Bisoprolol.
Method of administration and dosage in various cases
Basic rules for using the drug: 1 time per day in the morning, without chewing, regardless of food intake, with a glass of water.
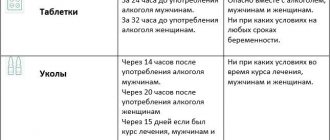
The product is incompatible with alcoholic beverages. Concomitant use with alcohol reduces the therapeutic effect and increases the likelihood of adverse reactions.
Arterial hypertension, ischemic heart disease with angina pectoris
Treatment begins with minimal doses and is gradually increased to therapeutic (effective). The target daily amount of Bisoprolol is 5 mg (if necessary - 10 mg).
The daily dosage is selected individually in accordance with blood pressure and heart rate.
CHF with LV systolic dysfunction
For treatment, a combination of Bisoprolol with ACE inhibitors, diuretics and angiotensin-2 blockers is used. Before starting therapy, it is necessary to exclude the possibility of progression of the pathology.
Therapy for CHF involves a “stepwise” increase in the dose of the drug over 3 months. Transition to a higher concentration is allowed if the previous one is satisfactory.
| weeks | Daily dose (mg) |
| 1st | 1,25 |
| 2nd | 2,5 |
| 3rd | 3,75 |
| 4-7th | 5 |
| 8-11th | 7,5 |
| 12th | 10 |
If undesirable consequences of taking the drug or exacerbation of heart failure occur, therapy with Bisoprolol is temporarily discontinued. Treatment is resumed after normalization of the patient's parameters with a minimum dose of 1.25 mg.
Selection of an effective dosage by titration requires constant monitoring by a doctor: the patient is in a day hospital.
Abrupt cessation of taking the drug in case of CHF is accompanied by a risk of progression of circulatory disorders, and in case of coronary artery disease - an increase in the frequency of attacks of chest pain in patients.
Bisoprolol is prescribed with extreme caution to patients with bronchospasm, uncontrolled diabetes mellitus, those on a strict diet, obliterating vascular pathologies and Prinzmetal's angina.
Contraindications
The complex effect of the active substance on organs and tissues is the main reason for restrictions on taking Bisoprolol:
- Uncontrolled circulatory failure (acute or chronic), the treatment of which requires parenteral administration of medications.
- Cardiogenic shock - taking the drug aggravates the patient's condition.
- Conduction disturbance along the atrioventricular connection of 2-3 degrees, with the exception of patients with a pacemaker.
- Sick sinus syndrome is a primary disorder of cardiac automaticity. Taking Bisoprolol is one of the reasons for hemodynamic ineffectiveness.
- Secondary bradycardia, arterial hypotension.
- Uncontrolled bronchial asthma (BA). One of the side effects of the drug is spasm of the smooth muscles of internal organs, which provokes obstruction in patients with asthma.
- Raynaud's disease (angiotrophoneurosis) is a vascular pathology with impaired tone of the smooth muscles of the arterial wall. An additional decrease in pressure is the cause of microcirculation disorders.
- Pheochromocytoma (in the preoperative period).
- Metabolic acidosis.
- Acute and chronic renal failure.
- Hepatic encephalopathy.
- Persistent hypokalemia, hyponatremia.
- Acute glomerulonephritis.
An absolute contraindication to taking the drug is intolerance to Bisoprolol or the auxiliary components of the drug. In other cases, the doctor evaluates the risks and benefits for the person.
Side effects
Undesirable consequences of taking the drug most often occur during induction therapy, are mild and disappear within 10-14 days. Possible adverse reactions during treatment with Bisoprolol:
- slow heart rate, signs of worsening heart failure;
- violation of intracardiac conduction;
- dizziness, migraines, fainting;
- dry eye syndrome;
- bronchospasm in patients with chronic obstructive pulmonary diseases;
- nausea, stool disorders;
- hypersensitivity reaction, urticaria, itching;
- muscle asthenia, cramps;
- reactive hepatitis;
- feeling of coldness, numbness, “crawling” in the extremities, arterial hypotension;
- decreased potency;
- depressive disorders, insomnia, nightmares;
- increased levels of cholesterol, triglycerides, transaminase activity (ALT, AST);
- general malaise, loss of strength.
Violation of the regimen of administration, dosage of the drug, metabolic and excretory disorders are the causes of the development of intoxication. Clinical signs of an overdose of Bisoprolol:
- slow pulse - bradycardia;
- drop in blood pressure, up to collapse, loss of consciousness;
- acute cardiovascular failure;
- hypoglycemic state (more often in patients with diabetes mellitus);
- bronchospasm.
There is no antidote (specific antidote) for acute intoxication with Bisoprolol. Overdose therapy is carried out depending on the symptoms of the disorder.
- intravenous administration of 1 ampoule of 1% Atropine solution;
- infusion of 0.9% NaCl solution and vasoconstrictor drugs (“Adrenaline”);
- administration of 2% Isoprenaline solution;
- diuretics (“Furosemide”, “Veroshpiron”, “Hypothiazide”);
- β2-adrenergic agonists (“Salbutamol”, “Fenoterol”, “Terbutaline”);
- dropper with glucose and Glucagon.
Drug compatibility
Complex therapy of cardiovascular diseases requires the selection of safe combinations to achieve maximum effect. Drug interactions of Bisoprolol with other drugs are presented in the table.
| Concomitant use is prohibited | Careful use recommended |
|
|
Research results
According to the results of the SDS test, the use of therapy with bisoprolol led to an increase in the duration of development of SDS at the minimum limit of the synchronization range (by 20.9%); a decrease in the synchronization range (by 18.8%) and the RAS index (by 46.3%). These changes indicate a decrease in ASD. As a result of taking sotalol, patients experienced a decrease in the synchronization range (by 9.4%) and the RAS index (by 12.7%); there was no significant change in the duration of development of SDS at the minimum border of the synchronization range. Thus, these changes show a less pronounced decrease in RAS when taking sotalol compared to that in the bisoprolol group (Table 2).
According to the results of echocardiography, during the use of therapy with bisoprolol, the peak velocity of the transmitral diastolic flow E (VE) increased (by 7.8%), the ratio of VE and the peak velocity of the transmitral diastolic flow A (VA) (VE/VA) (by 18.2 %), peak velocity of LV base elevation in early diastole (Ve′) (by 21.1%), deceleration time of transmitral diastolic flow E (DTE) (by 25%); the end-diastolic size (EDD) of the LV decreased (by 7.6%), the anteroposterior size of the left atrium (LA) (by 5.6%), the ratio of VE and Ve′ (VE/Ve′) (by 17.6% ), VA (by 12.6%); LVEF, interventricular septal thickness (IVS) and posterior wall thickness (PV) were not subject to significant changes. The listed changes indicate an improvement in the structural and functional parameters of the myocardium. As a result of therapy with sotalol, VE (by 8.4%), VE/VA (by 20%), Ve′ (by 18.5%), DTE (by 31.7%) increased; LV EDV decreased (by 4.6%), LA anteroposterior size (by 2.4%), VA (by 9.7%), VE/Ve′ (by 20.5%); LVEF, LV PV thickness, and IVS thickness did not change significantly. These changes demonstrate regression of cardiac remodeling processes, which is comparable to that under the action of bisoprolol (Table 3). In both groups, LV isovolumetric relaxation time (IVRT) increased comparablely.
According to the results of the treadmill test, during therapy with bisoprolol, the maximum load increased (by 11.9%), and the double product decreased (by 17.1%). During sotalol therapy, the maximum load increased (by 14.6%) and the double product decreased (by 16.3%). Thus, both pharmacological treatment regimens increased exercise capacity to the same extent.
According to the results of TSHM, patients taking bisoprolol as part of combination drug therapy showed an increase in the distance traveled (by 14.5%). In 30% of patients there was a decrease in FC of CHF from II to I, in 8% of cases CHF was not registered. Therapy with sotalol led to an increase in the distance traveled (by 16.3%); in 30% of patients the FC of CHF decreased from II to I, in 10% of cases CHF was not registered. Thus, both regimens of pharmacological therapy comparablely reduced the FC of CHF (Table 4).
According to the BP data, target blood pressure values were achieved in 87% of patients taking bisoprolol and in 83% of those taking sotalol.
According to the results of the SM ECG, the use of bisoprolol as part of combined pharmacological therapy made it possible to achieve a decrease in the average heart rate (HR) (by 18.2%), SVT paroxysms (by 69.1%) and the number of supraventricular extrasystoles (by 62.8%). During therapy with sotalol, the average heart rate (by 21.5%), the number of paroxysms of SVT (by 76.4%) and supraventricular extrasystoles (by 79.3%) decreased. The results obtained demonstrate targeted and comparable antiarrhythmic efficacy of combined pharmacological therapy in both groups.
According to the QOL questionnaire for patients with arrhythmia, the sum of negative scores as a result of therapy using bisoprolol decreased by 33%, and during therapy with sotalol - by 47.5%. Obviously, therapy using sotalol improved the quality of life of patients more significantly than using bisoprolol (Table 5).
When using bisoprolol as part of combination pharmacotherapy, side effects occurred in 13% of cases: erectile dysfunction (n=1), dry cough (n=1), drowsiness (n=1), dyspepsia (n=1). During therapy with sotalol, side effects were observed in 17% of cases: dry cough (n=2), drowsiness (n=2), dyspepsia (n=1). These manifestations were mild and transient in nature, which did not require exclusion of patients from the study or discontinuation of therapy.
Analogues and cheaper substitutes
The original "Bisoprolol" (generic name) is produced in Germany by the pharmaceutical company Merck under the name "Concor". The cost on the Russian market ranges from 130 to 460 rubles per package, depending on the dosage of the drug. Currently, many generics (official substitutes) of medicine with a similar composition of imported and domestic manufacturers are registered.
Analogues of "Bisoprolol":
- Russia - Bisoprolol Astrapharm, Aritel;
- Germany - “Bisogamma”, “Cordinorm”, “Bisocard”, “Bisoprolol” (Sandoz, Richter, Ratiopharm);
- Czech Republic – “Coronal”;
- Slovenia - Niperten, Bisoprolol-KRKA;
- Hungary – “Bidop”;
- Italy - "Biol".
Our recommendations
- When choosing a medication with the active substance bisoprolol, it is better to choose Concor. Medicines produced in Europe are no less effective.
- When purchasing Russian drugs, the huge advantage is the price. However, there can be the same quality underneath the low price.
- The choice of analogue must be approached with all responsibility. Otherwise, the situation may only get worse. A properly selected analogue can completely replace Bisoprolol.
Tell everyone:
conclusions
The use of Bisoprolol improves the functional state of the cardiovascular system and prevents the development of stroke and heart attack in coronary artery disease. Correctly selected doses of the drug do not interfere with bronchial patency and respiratory function in patients with obstructive pathology, and do not change the metabolism of glucose and lipids. It is not recommended to self-prescribe or o. Before use, you should carefully read the description of the drug. Clinical practice has confirmed that regular use of the drug according to indications increases the duration and quality of life of patients.