03 Jun 2021 at 09:50 MRI of the heart in Tushino 14801
Left ventricular hypertrophy is a fairly common heart disorder. The disease in most cases begins to develop in patients suffering from hypertension. Hypertrophy provokes an increase in the size of the wall of the left ventricle. The disease can provoke a change in the size of the septum, which is located between the left and right ventricles. The development of hypertrophy in most cases occurs over several years.
LEFT VENTRICLE ACTIVITY
Sinus rhythm accelerated heart rate 90. El.
The axis of the heart is semi-horizontal. ORRT is not clearly expressed (or SRRT - illegible). Predominance of left ventricular activity. What it is? Strangely enough, my blood pressure in a calm state at home (when measured with an electronic tonometer) is constant/up to 80, and my pulse is always normal, as soon as I see any doctor, jitters and anxiety begin, my hands tremble, and my heart starts beating about 100 and blood pressure 140/100.
It is clear that home blood pressure monitors have an error, but not as much?
Simply put, the heart is an electrically driven pump.
Typically, electrical stimulation of the heart begins in the sinus (sinoatrial) node. It is located in the right atrium near the mouth of the superior vena cava. This node consists of specialized cells that can automatically produce an electrical impulse. From the sinus node, the impulse spreads to the right atrium and then to the left atrium.
The first stage of activation of the heart muscle is electrical excitation of the right and left atria. This, in turn, is a signal for contraction of the atria, which simultaneously provide blood flow through the tricuspid and mitral valves into the right ventricle and left ventricle. The electrical impulse then travels to specialized conductive tissue at the atrioventricular junction, which includes the AV node and the Tis bundle. After this, the impulse passes to the left bundle branch of His (LBB) and the right bundle branch of His (RBBB), and then to the ventricular myocytes.
It is located at the base of the interatrial septum and extends to the interventricular septum. The superior (proximal) part of the AV connection is the AV node (sometimes the terms “atrioventricular node” and “atrioventricular junction” are used interchangeably). The lower (distal) part of the AV junction is called the bundle of His, named after the physiologist who described it.
The electrical impulse simultaneously propagates along the LBP and PNPG to the ventricular myocardium with the help of specialized conductive cells (Purkinje fibers), which are located in the ventricular myocardium.
Normally, when the heart's excitation begins in the sinus node (normal sinus rhythm), the AV junction transmits the electrical impulse to the ventricles. However, under some circumstances, the AV junction can act as an independent pacemaker of the heart (for example, if the sinus node function is impaired, it can become the source of an ectopic rhythm). In such cases, instead of sinus rhythm, an AV junction rhythm occurs, which is clearly visible on the electrocardiogram.
The propagation of electrical impulses through the atria leads to contraction of the atria, and propagation through the ventricles leads to contraction of the ventricles. As a result, blood flows to the lungs and into the systemic circulation. Contraction of the heart after its electrical excitation can be considered as electromechanical coupling. This mechanism is based on the entry of calcium ions into the myocytes of the atria and ventricles during the propagation of an electrical impulse.
When using site materials, a backlink is required
The human body is characterized by the ability to quickly adapt to various changes in the functioning of the circulatory system. In most hypertensive patients, due to a persistent increase in blood pressure, a compensatory increase in the left ventricle occurs, which is fraught with loss of tissue elasticity with weakening of the cardiac septum.
Diagnostic methods
Before making a diagnosis, your doctor will take your medical history and perform a thorough physical examination, including taking your blood pressure and testing your heart function. If preliminary studies indicate that the ventricle may indeed be enlarged, a number of additional screening tests are performed.
Electrocardiogram (ECG)
Electrical signals will not confirm ventricular enlargement. But cardiologists can identify some difficulties in the passage of the impulse, which will indicate a violation of the density of the muscle tissue of the heart.
MRI
Images of the heart taken with a special tomograph will directly indicate ventricular hypertrophy.
2Signs of predominance of ventricular potentials
Predominance of left ventricular potentials
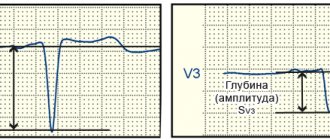
The predominance of ventricular potentials or the predominance of its electrical activity is detected by the electrocardiographic method. ECG signs of the predominance of LV activity are changes in the leads responsible for the left parts of the heart. Since the R wave on the cardiogram is responsible for the excitation of the ventricles, the dominance of RV or LV activity will influence changes in this wave in the corresponding leads. If LV activity predominates in the left precordial leads (I, II, AVL, V5-V6), the R wave will be larger than normal - more than 25 mm.
In the right leads, changes in the negative S wave will be observed. It will be more than 15 mm in depth in III, AVF, V1-V2. If the activity of the pancreas predominates, the opposite picture will occur. In the right leads, the height of the R wave will be greater than 7 mm. In the left chest leads, the negative S wave will be deeper than 7 mm. However, you should not draw conclusions only based on the R and S waves. It is necessary to evaluate other elements of the electrocardiogram, combining everything with clinical data.
Signs of LVH on ECG
LVH or left ventricular hypertrophy is an increase in the volume of the structural unit of the heart (left ventricle) due to increased functional loads that are incompatible with capabilities. Hypertrophy on the ECG is not the cause of the disease, but its symptom. If the ventricle extends beyond its anatomical size, then the problem of myocardial overload already exists.
Severe signs of LVH on the ECG are determined by a cardiologist; in real life, the patient experiences symptoms of heart disease, which determine dilatation (pathological enlargement of the heart chamber). The main ones include:
- instability of heart rhythm (arrhythmia);
- symptom of short-term cardiac arrest (extrasystole);
- persistently elevated blood pressure;
- extracellular hyperhydration of the extremities (edema due to fluid retention);
- lack of oxygen, impaired frequency and depth of breathing (shortness of breath);
- pain in the heart area, chest area;
- short-term loss of consciousness (fainting).
If symptoms appear on a regular basis, this condition requires consultation with a doctor and an electrocardiographic examination. A hypertrophied ventricle loses its ability to contract fully. Impaired functionality is displayed in detail on the cardiogram.
In the early stages, as a rule, there are no symptoms of the disease, as the heart copes with increased load. Further manifestations of LV hypertrophy are as follows:
- heart pain and shortness of breath, which worsen with physical activity;
- weakness, dizziness;
- cardiopalmus;
- swelling of the legs and feet, especially in the evenings.
Complications of left ventricular hypertrophy are arrhythmia, systemic circulatory disorders, coronary heart disease (including heart attack, sudden cardiac arrest).
Slow and uneven enlargement of the heart muscle, which can develop over years, is often characterized by a blurred clinical picture. Many people first learn about the presence of LVH only during a routine examination with detailed visualization of the chambers of the heart. Other variants of moderate myocardial hypertrophy are accompanied by pronounced symptoms, presented in the form of arrhythmia, angina pectoris, shortness of breath, and cyanosis.
Severe left ventricular hypertrophy is accompanied by shortness of breath and chest pain, as well as a feeling of palpitations and interruptions in heart function.
The most common signs indicating compensatory enlargement of the left ventricle include:
- chest pain, the pathogenesis of which is associated with compression of the coronary vessels that provide oxygen to the myocardium;
- a violation of the heart rhythm, which, due to its nature, can vary greatly in different patients: some patients experience severe tachycardia, others note interruptions in the functioning of the heart or atrial fibrillation;
- a feeling of lack of oxygen and rapid fatigue become frequent companions of left ventricular hypertrophy, since increased myocardial contractions due to an increase in muscle fibers leads to chronic fatigue due to overstrain of the circulatory system;
- changes in blood pressure, which most often consist of persistent hypertension, can be both a consequence of left ventricular hypertrophy and its true cause;
- a pressing headache that occurs against the background of spasm of cerebral vessels significantly affects the general well-being of the patient, and ischemia of brain tissue over time contributes to the development of chronic dizziness and impaired visual acuity.
The clinical picture of the disease largely depends on the cause that caused myocardial hypertrophy. If we are talking about renal hypertension, then the above symptoms are added to frequent urination and pain in the lumbar region. In case of myocardial infarction, which has caused a compensatory increase in healthy areas of the heart, cardiac arrhythmias and signs of tissue ischemia will predominate.
Also, in the stage of decompensation, the patient may experience episodes of cardiac asthma, since the myocardium of the left ventricle is not able to pump the required amount of blood
Factors causing the disease
Excessive load on the LV is based on congenital or acquired heart disease.
Hereditary anomalies include:
- Genetic defects. They arise as a result of mutation of one of the genes responsible for the synthesis of heart proteins. In total, about 70 persistent changes were found in these genes that cause proliferation of the LV myocardium.
- Congenital defects: decreased aortic diameter (coarctation), ventricular septal defect, closed or absent pulmonary artery. It is with hereditary defects of the heart muscle that left ventricular hypertrophy in children is associated. Here the main type of therapy is surgical intervention.
- Congenital narrowing of the aortic valve (the outlet of the left ventricle through which blood is ejected into the artery). Normally, the valve area is 3-4 square meters. cm, with stenosis it narrows to 1 square. cm.
- Mitral insufficiency. A defect in the valve leaflets causes blood to flow back into the atrium. Each time during the relaxation phase, the ventricle becomes filled with blood (volume overload).
Acquired left ventricular myocardial hypertrophy can develop under the influence of certain diseases and factors:
- Arterial hypertension. Holds first place among pathologies causing myocardial compaction (90% of cases). Muscle tissue grows due to the fact that the organ constantly works under pressure overload;
- Atherosclerosis of the aorta. Cholesterol plaques are deposited on the walls of the aorta and in its valve, which later become calcified. The walls of the main artery lose elasticity, which interferes with the free flow of blood. The LV muscle tissue, experiencing increasing tension, begins to increase its volume;
- Cardiac ischemia;
- Diabetes;
- Overeating, high weight, obesity;
- Prolonged stress;
- Alcoholism, smoking;
- Adynamia;
- Insomnia, emotional instability;
- Hard physical work.
All of the above causes of left ventricular hypertrophy cause the heart to work more intensely. The reason for this is thickening of the myocardium .
Basic ECG concepts for the left ventricle
The rhythmic work of the heart muscle creates an electric field with electrical potentials having a negative or positive pole. The difference between these potentials is recorded in leads - electrodes attached to the patient’s limbs and chest (indicated “V” on the graph). The electrocardiograph records changes in signals that arrive over a certain time range and displays them as a graph on paper.
A fixed time period is reflected on the horizontal line of the graph. Vertical angles (teeth) indicate the depth and frequency of impulse changes. Teeth with a positive value are displayed upward from the time line, with a negative value - downward. Each tooth and lead are responsible for recording the functionality of a particular cardiac section.
Indicators of the left ventricle are: waves T, S, R, segment S-T, leads – I (first), II (second), III (third), AVL, V5, V6.
- The T-wave is an indicator of the recovery stage of the muscle tissue of the ventricles of the heart between contractions of the middle muscular layer of the heart (myocardium);
- Q, R, S - these teeth show agitation of the cardiac ventricles (excited state);
- ST,QRST, TP are segments indicating the horizontal distance between adjacent teeth. Segment prong = interval;
- Leads I and II (standard) – display the anterior and posterior walls of the heart;
- III standard lead – fixes I and II according to a set of indicators;
- V5 – lateral wall of the left ventricle in front;
- AVL – lateral cardiac wall anterior to the left;
- V6 – left ventricle.
Schematic representation of ST segment elevation in V1 and V2, indicating LVH
The electrocardiogram evaluates the frequency, height, degree of jaggedness and location of the teeth relative to the horizontal in the leads. The indicators are compared with the norms of cardiac activity, changes and deviations are analyzed.
Learn more about changing tine values
Left ventricular hypertrophy is visually determined by the height and width of the R wave in leads V5 V6 (increased wave parameters), compared to leads V1, V2. Transformation of the T-wave in leads V5, V6 indicates left-sided pathology in the case of:
- negative tooth value;
- doublings (two parts of one tooth);
- the first half “looks” down, and the second half looks up.
A slight displacement of the S-T segment up or down relative to the horizontal line is a sign of thickening of the walls of the left ventricle. Significant displacement is an indicator of myocardial infarction or ischemic heart disease (coronary heart disease).
The S-wave in the presence of a hypertraffiated ventricle changes as follows:
- in leads: III, AVF, V1, V2 – increased depth of the tooth;
- in leads: AVL, V5, V6, I – weakly expressed;
- jaggedness is observed.
Deviations from the norm of the parameters of the Q, R, S waves are called the voltage of the cardiogram. If the teeth are located below normal by more than 0.5 mV, a low-voltage potential will be recorded on the cardiogram. Voltage changes always indicate the presence of cardiac pathology.
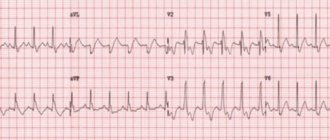
Electrocardiogram of the heart with LVH (signs of pathology are circled in red)
Symptoms, causes and treatment of left ventricular myocardial hypertrophy
Left ventricular hypertrophy is a syndrome characteristic of most diseases of the cardiovascular system, which consists of an increase in the muscle mass of the heart.
Unfortunately, today there are more and more cases of left ventricular hypertrophy in young people. The danger of this is complemented by a higher percentage of deaths than in older people. Men with left ventricular myocardial hypertrophy die 7 times more often than the fairer sex.
Development mechanism
In a normal physiological state, the heart, pushing blood into the aorta, performs the function of a pump. From the aorta, blood flows to all organs. When the left ventricle relaxes, it receives a portion of blood from the left atrium. Its quantity is constant and sufficient to ensure optimal levels of gas exchange and other metabolic functions throughout the body.
As a consequence of the formation of pathological changes in the cardiovascular system, it becomes more difficult for the heart muscle to perform this function. To perform the same amount of work requires more energy expenditure. Then a natural compensatory mechanism is activated - an increase in load leads to an increase in the muscle mass of the heart. This can be compared to how increasing the load on the muscles in the gym results in an increase in muscle mass and volume.
Why can’t the left ventricle “build up” its muscle mass without disturbing its owner? The fact is that in the heart tissue only cardiomyocytes increase. And they make up only about a quarter of the heart tissue. The connective tissue part does not change.
The capillary network does not have time to develop after LV hypertrophy, so rapidly hypertrophied tissue may suffer from oxygen starvation. Which leads to ischemic changes in the myocardium. In addition, the conduction system of the heart remains the same, which leads to disruption of impulse conduction and various arrhythmias.
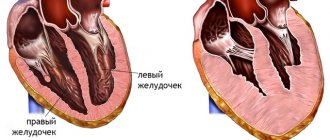
The tissue of the left ventricle, in particular the interventricular septum, is most susceptible to hypertrophy.
During intense physical activity, the heart has to pump more blood and work harder. Therefore, professional athletes may develop moderate left ventricular hypertrophy, which is physiological or compensatory.
In almost all long-term heart diseases, left ventricular hypertrophy is an obligatory consequence.
Left ventricular myocardial hypertrophy is observed with:
- hypertension;
- aortic valve stenosis;
- hypertrophic cardiomyopathy;
- intense long-term physical activity;
- obesity;
- smoking, drinking alcohol.
Thus, for any heart disease, left ventricular hypertrophy is a mandatory syndrome.
Hypertension, especially persistent and poorly treated hypertension, is the main culprit. If the patient says that high blood pressure numbers are familiar and “working” for him, if hypertension was corrected only occasionally or not treated at all, then he certainly has severe hypertrophy of the left ventricle of the heart.
Excess weight is a risk factor for hypertension, which causes left ventricular hypertrophy. In addition, with obesity, blood supply to an enlarged body requires a lot of work to ensure blood supply to all tissues, which also leads to changes in the myocardium.
Of the congenital diseases, the main place is in heart defects with impaired blood outflow from the ventricle.
However, left ventricular hypertrophy will show the same symptoms for any etiology.
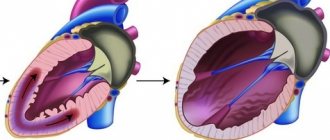
Types of hypertrophy
According to the degree of change in the shape of the left ventricle of the heart and its thickness, eccentric and concentric hypertrophy of the left ventricular myocardium is distinguished.
Concentric hypertrophy of the left ventricle is characterized by thickening of its walls. Its cavity in this case does not change. It is formed when the ventricle is overloaded with blood pressure. This form is typical for hypertension. This etiology accounts for at least 90% and has a high risk of life-threatening cardiovascular complications - more than 35%.
Eccentric left ventricular hypertrophy is characterized by relative preservation of the thickness of the walls of the ventricle, an increase in its mass and the size of the cavity. The risk of severe complications is about 25%. This type develops when there is excess blood volume.
For a long time, left ventricular hypertrophy of the heart has minor symptoms or the heart does not let you know that it is working through force. When compensatory capabilities are exhausted and a person begins to complain, the changes in the myocardium are already significant.
The following signs of left ventricular hypertrophy appear in varying degrees of severity:
- dyspnea;
- tachycardia;
- cardiac pain;
- feeling of weakness and fainting;
- fast fatiguability.
Timely early detection reduces the risk of developing severe complications. ECG signs of left ventricular hypertrophy are easily determined by any therapist. This method is cheap and informative.
Left ventricular hypertrophy on the ECG is manifested by an increase in the pulse transit time, ischemic changes on the ECG, impaired impulse conduction, deviation of the axis to the hypertrophied area, a shift in the electrical position of the heart, and the location of the transition zone.
Treatment
If there is difficulty breathing, there is a desire to stop and catch your breath with the usual load, if there is pressure in the chest, or causeless weakness occurs, then you should consult a doctor.
The cardiologist will prescribe a complete clinical, biochemical and instrumental examination. Upon examination, specific heart murmurs and an increase in its boundaries may be detected. An X-ray examination will show how enlarged the heart is and in what parts. An echocardiogram will help determine the location of disorders and the degree of decrease in heart activity.
Once a diagnosis of left ventricular myocardial hypertrophy has been established, treatment depends on the degree of its severity and the severity of the patient’s general condition.
Changes in heart size are a consequence of other diseases. When treating a patient diagnosed with left ventricular hypertrophy, the causes that led to it are of primary importance.
Depending on the severity of the patient’s condition and how severe the left ventricular hypertrophy is, treatment can be carried out in a hospital or at home.
A prerequisite for successful treatment is a correct lifestyle. If this recommendation is ignored, any therapy is useless.
The diet reduces salt intake. Products that strengthen the heart muscle are recommended.
Constant monitoring of ECG and blood pressure levels and regular examination by a cardiologist are required.
If your condition is satisfactory, regular walks in the fresh air are good. Also, moderate left ventricular hypertrophy does not exclude race walking and swimming at a gentle pace. Excessive physical activity is avoided.
Medicines are taken throughout life. These are calcium channel blockers, beta blockers, antihypertensive drugs, metabolic cardiac medications.
In some cases, surgery may be recommended. During the operation, areas of thickened muscle are excised.
Complications
Complications are more than dangerous. This includes circulatory failure, rhythm disturbances, ischemic changes, and myocardial infarction.
Cardiovascular failure is the inability of the heart to perform its pumping function and provide the body with blood.
Rhythm disturbances occur as a result of the fact that the conduction system of the heart does not have the ability to hypertrophy. The time and quality of impulse conduction changes. Areas may appear where impulses do not pass through.
Ischemic manifestations (lack of oxygen in the tissue) occur due to the relatively slow development of the capillary network in the hypertrophied heart tissue. As a result, she does not receive enough oxygen. On the other hand, when working with increased load, the myocardial need for oxygen increases significantly.
For hypertrophy of the left ventricle of the heart, treatment continues for a long time. It has been proven that early treatment and the patient’s responsible attitude towards it can significantly improve the quality and length of life of patients.
Left ventricular hypertrophy detected during an ECG means the presence of excessive load on the heart and myocardial diseases:
- narrowing of the aortic lumen in the valve area (aortic stenosis). Due to the transformation of the valve leaflets, blood flow is disrupted, and the heart is forced to work in emergency mode;
- change in the volume of the left ventricular wall towards thickening (hypertrophic cardiomyopathy). The thickness of the walls impedes blood circulation, which increases the load on the myocardium;
- persistently high blood pressure (hypertension).
Deformation can occur due to reasons that depend directly on the patient himself. First of all, these are the following factors: eating habits leading to obesity, irrational physical activity. LVH is common to many athletes, since excessive load on the heart during training provokes an increase in the volume and mass of the organ, systematic psycho-emotional overload (state of stress), and an unhealthy lifestyle (smoking, alcohol, lack of fresh air, unhealthy foods).
When working under conditions of increased overload of the circulatory system with the volume of circulating blood or due to spasm of arterial vessels, the left ventricle increases in size to adapt to such situations.
Cardiomyocytes acquire greater volume and length. If there is not enough blood flow in the coronary arteries, then the myocardium experiences a nutritional deficiency, the manifestation of which is ischemia. When compensation reserves are depleted, insufficiency of cardiac contractility develops.
The etiological factors of myocardial hypertrophy are different; they can be physiological (in athletes and people of physical labor) and pathological.
The progressive course of hypertrophy leads to ineffective cardiac output, which is manifested by the following complications:
- acute or chronic cardiac decompensation,
- sudden cardiac arrest,
- ventricular fibrillation,
- ischemia or infarction of the heart muscle,
- arterial thromboembolism,
- stroke.
Diagnosis of cardiomyopathy
Diagnosis of left ventricular hypertrophy occurs in several ways: by identifying signs of the disease on an ECG, examining the heart using ultrasound or using a magnetic resonance imaging scanner. If you experience any heart problems or symptoms of illness, you should contact a cardiologist, and if you have already suffered some kind of defect and suspect complications, you need a cardiac surgeon and, possibly, a treatment system.
Left ventricular hypertrophy on ECG
ECG is a common diagnostic method that helps to find out the thickness of the heart muscle and voltage characteristics. However, it can be difficult to identify LVH on an ECG without the participation of other methods: an erroneous diagnosis of hypertrophy may be made, since on the ECG the signs that are characteristic of it can be observed in a healthy person. Therefore, if they are found in you, this may be due to increased body weight or its special constitution. Then it is worth conducting another echocardiographic examination.
LVH on ultrasound
Ultrasound examination helps to more likely judge individual factors and causes of hypertrophy. The advantage of ultrasound is that this method allows not only to diagnose, but also to determine the characteristics of the course of hypertrophy and the general condition of the heart muscle. Indicators of cardiac echocardiography reveal changes in the left ventricle such as:
- ventricular wall thickness;
- ratio of myocardial mass to body mass;
- coefficient of asymmetry of seals;
- direction and speed of blood flow.
MRI of the heart
Magnetic resonance imaging helps to clearly calculate the area and degree of enlargement of the ventricle, atrium or other compartment of the heart, and to understand how strong the degenerative changes are. MRI of the myocardium shows all the anatomical features and configuration of the heart, as if “stratifying” it, which gives the doctor complete visualization of the organ and detailed information about the condition of each department.
Dangerous consequences
The left ventricle is responsible for oxygen saturation and movement of arterial blood into the aorta and further through all small vessels to nourish the organs. As the volume increases, the blood presses on the walls, the connective tissue displaces the muscle tissue, and the ventricle ceases to cope with its functional duties.
Pathology can even lead to death
What such changes threaten is determined by the following diagnoses:
- coronary heart disease - a violation of the blood supply to the heart due to thickening of the walls of the gastric chamber;
- myocardial infarction – death (necrosis) of part of the heart muscle;
- ventricular extrasystole (arrhythmia) – failure of the heart rhythm;
- atrioventricular or ventricular block - cessation of the passage of electrical impulses between the atria and ventricles, leading to hemodynamics;
- heart failure is a low contractility of the heart muscle, often leading to death.
Timely detection of LVH will help prevent serious complications. The most informative in terms of diagnosing pathology is the electrocardiographic examination method.
Reasons for the development of the anomaly
Enlargement of the left ventricle can occur if some unfavorable factor causes the heart to work harder than usual. This means that the heart muscle will need to make several times more contractions in order to pump blood around the body.
Model of the heart with left ventricular hypertrophy
Reasons that can provoke a significant deterioration in heart function:
- High blood pressure (hypertension) is considered the most common cause of thickening of the ventricular wall. More than one third of all patients learn about hypertrophy at the time of diagnosis of arterial hypertension.
- Aortic valve stenosis is a disease that is a narrowing of the flap of muscle tissue that separates the left ventricle from the aorta. Narrowing of the aortic valve causes the heart to contract several times more often in order to pump blood into the aorta.
- Hypertrophic cardiomyopathy is a genetic disease that occurs when the heart muscle becomes abnormally thick and stiff.
- Professional sports. Intense, long-term strength training, as well as irregular performance of endurance exercises, can lead to the fact that the heart is not able to quickly adapt and cope with the additional load. As a result, the left ventricle may swell (enlarge).
Prevention of LVH
The main preventive measures include:
- elimination of bad habits (alcohol and nicotine addiction);
- a healthy diet (eliminating foods containing low-density lipoproteins, the so-called bad cholesterol, while increasing the intake of high-density lipoproteins, the “good cholesterol”);
- body weight control (obesity always negatively affects heart function);
- balanced physical activity appropriate for age;
- regular exposure to fresh air (active oxygen stimulates proper cardiac activity).
These recommendations will help not only avoid heart disease, but also improve your overall quality of life.
Hypertrophy can be prevented only by following the doctor’s recommendations for the treatment of hypertension, atherosclerosis, endocrine and renal pathologies. At the same time, giving up bad habits, normalizing weight and dosed physical activity significantly increase the chances of recovery. In children, timely diagnosis of heart defects and rheumatic diseases, as well as their surgical correction, plays an important role.
Diagnosis of left ventricular hypertrophy using ECG
What it is
Left ventricular (LV) hypertrophy implies an increase in its cavity and walls due to internal or external negative factors.
These usually include hypertension, nicotine and alcohol abuse, but moderate pathology sometimes occurs in people who play sports and are regularly exposed to heavy physical activity.
There are a number of criteria for assessing left ventricular function, which may differ significantly from patient to patient. Interpretation of an ECG consists of analyzing waves, intervals and segments and their compliance with established parameters.
In healthy people without LV pathologies, the ECG reading looks something like this:
- In the QRS vector, which shows how rhythmically excitation occurs in the ventricles: the distance from the first tooth of the Q to S interval should be 60-10 ms;
- The S wave should be equal to or lower than the R wave;
- The R wave is fixed in all leads;
- The P wave is positive in leads I and II, negative in VR, width – 120 ms;
- The internal deviation time should not exceed 0.02-0.05 s;
- The position of the electrical axis of the heart ranges from 0 to 90 degrees;
- Normal conduction along the left bundle branch.
Signs of abnormalities
On the ECG, hypertrophy of the left ventricle of the heart is characterized by the following signs:
- The average QRS interval deviates forward and to the right relative to its position;
- There is an increase in excitation going from the endocardium to the epicardium (in other words, an increase in the time of internal deviation);
- The amplitude of the R wave increases in the left leads (RV6{amp}gt;RV5{amp}gt;RV4 is a direct sign of hypertrophy);
- The SV1 and SV2 teeth deepen significantly (the more pronounced the pathology, the higher the R waves and the deeper the S waves);
- The transition zone moves to lead V1 or V2;
- The S-T segment passes below the isoelectric line;
- Conduction along the left bundle branch is impaired, or complete or incomplete blockade of the bundle is observed;
- The conductivity of the heart muscle is impaired;
- There is a left-sided deviation of the electrical axis of the heart;
- The electrical position of the heart changes to semi-horizontal or horizontal.
The normal thickness of the wall of the left ventricle (LV) of the heart is about 1 cm in an adult and 0.3 cm in a newborn. With increased load, a protective reaction occurs in the form of proliferation of the muscle layer. If the process occurs gradually, then at the same time a blood network has time to form, and this condition is considered a variant of the norm.
Pathological hypertrophy is most often associated with high blood pressure and leads over time to circulatory failure.
Treatment of hypertrophy
Treatment depends on the underlying cause of the enlarged ventricle and may include medications and/or surgery.
Left ventricular enlargement can be controlled by taking tablets
The most common medications prescribed for hypertrophy are the following.
Angiotensin-converting enzyme (ACE) inhibitors
These drugs dilate blood vessels, lower blood pressure, improve blood flow, and help reduce the workload of the heart. Trade names of the drugs: captopril, enalapril and lisinopril. The most common side effect is a persistent, irritating dry cough.
Angiotensin receptor blockers
These drugs are similar to ACE inhibitors, but do not cause a persistent cough.
Beta blockers
Beta blockers help lower your heart rate and normalize your blood pressure. Beta blockers are not usually prescribed as primary treatment for hypertrophy.
Diuretics
Thiazide diuretics help ease blood flow to the heart and lower blood pressure. Trade names: chlorthalidone and hydrochlorothiazide.
Only an experienced cardiologist will select the right type of pills
Surgical treatment consists of repairing or completely replacing the aortic valve.