Bradycardia is a change in heart rhythm in which the heart rate decreases to 30-50 beats per minute, due to a decrease in the automation of the sinus node.
The reasons for this condition are varied:
- sclerotic changes in the myocardium affecting the sinus node;
- exposure to cold;
- increased tone of the parasympathetic nervous system;
- increased intracranial pressure (with cerebral edema, tumor, meningitis, cerebral hemorrhage);
- influence of drugs (digitalis, quinidine);
- lead poisoning, nicotine;
- hypothyroidism (decreased thyroid function);
- starvation, typhoid fever, jaundice, etc.
A low heart rate can occur in well-trained athletes and some young healthy people (for example, cyclist Miguel Indurain had a resting heart rate of 28 beats/min[1]). This is normal in the absence of other pathological symptoms such as fatigue, weakness, dizziness, fainting, chest discomfort or difficulty breathing.
Minor disturbances of sinus rhythm may not cause any subjective sensations in a person. If there is a significant decrease in heart rate (less than 40 beats per minute), then the person may complain of weakness, dizziness, cold sweat, fainting due to brain hypoxia (oxygen starvation), since there is no adequate blood supply. In any case, it will be useful to have an examination with a cardiologist.
Causes of bradycardia
Neurogenic bradycardia
The main role in the development of a slow heartbeat is played by a disorder of the nervous system. It can be expressed in various pathological conditions: neuroses, vagoinsular crises, bleeding in the brain, inflammatory diseases of various brain structures. Among the causes of neurogenic bradycardia are renal, hepatic, and intestinal colic. Hernias and ulcers of the gastrointestinal tract can contribute to rhythm disturbances
Ischemic bradycardia
Ischemic bradycardia is influenced by a number of influencing factors. By taking them into account, you can reduce the risk of developing coronary artery disease, and with it, bradycardia. First of all, cardiologists pay attention to biological indicators (age, gender, hereditary predisposition). Behavioral characteristics play a role, in particular, nutrition, bad habits, and an inactive lifestyle. If necessary, anatomical, metabolic and physiological characteristics are analyzed.
Extracardiac bradycardia
Extracardiac bradycardia can be a consequence of traumatic lesions, which are accompanied by severe blood loss. Severe inflammation and infectious effects are also often accompanied by a slowdown in heart rate. If the thyroid gland does not function sufficiently (hypothyroidism), then bradycardia is one of the symptoms of the development of pathology.
Vagal bradycardia
Vagal bradycardia can develop for other reasons, more related to the internal state of the body. First of all, this is the aging process, nervous system disorders, and infectious diseases. Also, tumor processes, myxedema, and excess potassium in the blood affect cardiac activity. Some drugs - 23-24 (antihypertensive and vasodilators), if taken incorrectly, can also cause rhythm disturbances.
Hyperkalemia and bradycardia
A slow heartbeat primarily occurs with hyperkalemia (excess potassium in the blood). This condition is associated with several reasons. First of all, this is a violation of the excretion of potassium from the body, which is often observed with nephropathies, systemic lupus erythematosus, adrenal and kidney failure. Hyperkalemia in combination with bradycardia can develop with increased transition of a microelement from the plasma of cells into the intercellular fluid, and from there into the blood. This often develops with extensive injuries, burns, and ischemic tissue damage. Also, rhythm disturbances can occur against the background of a lack of insulin production and with the development of intracellular acidosis.
Drug-induced bradycardia
There are drugs that, if taken incorrectly, cause a slowdown in cardiac activity. In particularly severe cases, cardiac arrest may occur. Such drugs primarily include cardiac glycosides, which most often cause drug-induced bradycardia and emergency visits for patients who have taken these drugs incorrectly. Other such medications are potassium-containing medications. They are often used to eliminate tachycardia, while forgetting that excess potassium in the body negatively affects cardiac activity.
Drug-induced bradycardia can develop while taking muscle relaxants. They are often used to relax muscles, but if used incorrectly, the heart can stop. Anti-heartburn medications are also not as safe as they initially seem. Their prolonged use or incorrectly selected dose can cause quite pronounced bradycardia. However, the medicine can be passed through breast milk, so it is extremely important for nursing mothers not to take medications for heartburn.
Arrhythmia: types, diagnosis and treatment
What is a heart rhythm disorder called arrhythmia and why does its type, tachycardia, occur? - says Ekaterina Radikovna Perminova, a cardiologist at the CORDIS Medical Center. ⠀ Heart rate (HR) at rest is affected by age, physical fitness and other factors. A normal rhythm should be in the range of 60 to 100 beats per minute. The sinus node, which is located in the anterior upper part of the right atrium, is responsible for its regulation. Arrhythmia is a disturbance in heart rate, firing sequence, and conduction. It may feel like a sinking heart or appear as extraordinary contractions.
Arrhythmia has several types that differ from each other. The three main types include sinus, ventricular and atrial arrhythmia. They are further distinguished by heart rate:
- atrial fibrillation is considered the most common type. Cardiac muscle fibers work asynchronously due to twitching or “flickering” of the atria. Their reduction simply disappears. At the same time, the ventricles also stop working normally.
- tachycardia - in this condition, a person’s pulse exceeds 100 beats per minute. Tachycardia that occurs during heavy physical exertion is considered normal. But if you are completely calm and your pulse is high, we can talk about pathology.
- bradycardia - with this type of arrhythmia, the heart rate is less than 60 beats per minute. It often appears when you feel normal. But if you constantly feel unwell, the pathological process has already started.
- extrasystole usually appears for no apparent reason. A premature contraction seems to be woven into the normal heart rhythm. The cause of the attack can be severe stress.
- paroxysmal disorders are expressed in a sharp increase in pulse rate, strong heartbeat with the inability to count its beats. Sometimes their frequency reaches 200 beats per minute. This is a special type of tachycardia, leading to sudden weakness and even loss of consciousness. The condition is considered extremely dangerous. Immediate medical attention is needed here.
CAUSES OF ARRHYTHMIA Arrhythmia does not always occur due to problems related to the functioning of the heart. It can be a consequence of other cardiac pathologies: - heart attack - coronary heart disease - cardiomyopathy - myocarditis - arterial hypertension - heart failure - heart defects (congenital and acquired) - cardiosclerosis - injuries and wounds of the heart These diseases lead to damage to the heart muscle and complicate normal propagation electrical impulse of the heart to its parts. ⠀ HOW ARRHYTHMIA MANIFESTS
- sudden weakness
- headache
- dizziness to the point of loss of consciousness
- shortness of breath, lack of air
- fast or slow heartbeat
- chest compression, pain
BRADYCARDIA
indicates various cardiac pathologies. Most often it appears due to blockage of the sinus node and is characterized by a slowing of the heartbeat to 30-50 beats/min. Other causes of bradycardia include: - heart attack, coronary heart disease, arterial hypertension, heart disease - age-related changes in the heart muscle - reflex effects (cold water, blow to the chest or neck) - increased intracranial pressure, pressure on the carotid artery or eyeballs - stomach and duodenal ulcers - use of drugs that replace heart rate - consequences of poisoning with chemical or organophosphorus substances - disturbances in potassium balance and calcium levels
SYMPTOMS OF BRADYCARDIA If you have a heart rate less than 40 beats per minute, this may lead to the development of heart failure. Common symptoms of bradycardia include:
- general weakness, cold sweat
- pale skin and mucous membranes
- dizziness
- swelling
- convulsions
- dyspnea
- low blood pressure
- fainting or momentary loss of consciousness
- absent-mindedness
WHAT TO DO Unfortunately, arrhythmia can be either an independent pathology or a manifestation of another disease. Therefore, if you begin to sleep poorly, wake up with shortness of breath in the middle of the night, if you have tremors in your hands and you panic more and more often, you have heart problems. With sinus bradycardia, a rare pulse and respiratory arrhythmia are observed. To diagnose it, daily ECG monitoring, cardiac ultrasound, and exercise bicycle ergometry are prescribed. The sooner you see a doctor, the lower your risk of developing cardiovascular problems. Sinus bradycardia requires constant prevention. Quit smoking and alcohol, normalize blood pressure and weight, eat right. Worry less and exercise.
TACHYCARDIA
is not considered a severe pathology. Rather, it is a symptom when the heart rate exceeds 100 beats per minute. It is usually caused by increased physical activity in those who do not regularly engage in heavy physical labor or sports. But sometimes the CAUSES of tachycardia can be: - dehydration - increased sensitivity to coffee, strong tea, nicotine, alcohol - high temperature - sleep problems - anemia - obesity - strong emotions, stress, fear - old age - hypertension or hypotension - taking certain medications (from a runny nose or cough) - intoxication - in some cases - heart disease
In a completely healthy person, the heart rate can reach 150-200 beats/min. and higher. It happens that an attack lasts from several minutes to several hours. Your norm for tachycardia and arrhythmia is quickly passing symptoms without weakness, sweating and decreased blood pressure.
SYMPTOMS OF TACHYCARDIA You should consult a doctor when:
- heart rhythm disturbances occur frequently and for a long time
- you begin to experience shortness of breath, lack of air
- if you feel dizzy and sweat
- you urinate often
- you feel scared for no reason
- you stop sleeping normally, you lose your appetite
- there is pain in the heart area
- general health and mood are at zero
WHAT WE DO If you suddenly feel ill, apply a cold compress to your forehead, wash with cool water, and then take one of the sedatives: Corvalol, Valocordin, valerian, motherwort or peony infusion. Of course, if you discover symptoms of arrhythmia, you need to undergo an ECG examination. It shows the consequences of rhythm disturbances, even if you are already fine and the attack has passed. But it may happen that tachycardia is accompanied by loss of consciousness, severe chest pain or shortness of breath. Then call an ambulance immediately. Tachycardia should be treated only after its cause has been determined. To reduce the likelihood of unexplained tachycardia, avoid caffeine, spicy foods, chocolate, alcohol and cigarettes. Also, avoid serious physical activity and be less nervous.
AFIBLIRATORY ARRHYTHMIA
As you know, the heart must contract in a strictly ordered rhythm. And one of the deviations from it is atrial fibrillation (atrial fibrillation). ⠀ The prevalence of this rhythm disorder increases with age: approximately 6% of men and women over 60 years old suffer from atrial fibrillation. ⠀ What happens to our heart during an attack of atrial fibrillation? The atria begin to contract rapidly and erratically, and the sinus node does not coordinate the heart rhythm. These fibrillations can reach 300-600 per minute when the norm is from 60 to 90. Scary, right? ⠀ If atrial fibrillation lasts for a long time, blood clots may occur, and hence ischemic strokes and acute arterial insufficiency of the arteries of the upper or lower extremities. ⠀ REASONS This disease is caused by a number of reasons related to both cardiac pathologies and diseases of other organs or external factors affecting the body: - heart attack - arterial hypertension - tachycardia - myocarditis - severe heart failure - intoxication - cardiosclerosis - rheumatic heart defects - cardiomyopathy - thyrotoxicosis - diabetes - psycho-emotional overload - previous surgical interventions - hypokalemia ⠀ Atrial fibrillation in itself does not threaten your life. But atrial fibrillation interferes with the synchronous functioning of the heart and increases the risk of developing chronic cardiovascular failure and thromboembolic complications. ⠀ SYMPTOMS So, we can talk about atrial fibrillation if you find the following symptoms: erratic heartbeat
- feeling of heart fluttering
- chest pain
- weakness and sweating
- labored breathing
- dizziness and fainting
- shiver
- frequent urination
- feeling of fear
⠀ But as soon as you restore your heart rate, these symptoms disappear. Atrial fibrillation is of three types: - paroxysmal from 30 seconds to 7 days - persistent - longer than 7 days - constant
HOW TO DETECT The following are considered the most accurate diagnostic methods for identifying atrial fibrillation and the causes leading to it: ECG Ultrasound of the heart MRI of the heart Bicycle ergometry and treadmill test 24-hour Holter monitoring Blood test, which can be used to confirm or rule out other diseases You can measure your pulse yourself and assess the regularity and frequency of heart contractions. A fast, slow, or arrhythmic pulse indicates that your heart rhythm is abnormal.
WHAT TO DO First of all, make an appointment with a cardiologist. The doctor will prescribe you treatment to prevent “rhythm disruptions” and their complications, and correct diseases that lead to paroxysmal atrial fibrillation. In some cases, paroxysmal atrial fibrillation may require hospital treatment and electrical pulse restoration of rhythm. We will have to reconsider our lifestyle. If you abuse smoking, alcohol and fatty foods, give up everything that can have a bad effect on your health. Strong tea and coffee can also cause heart rhythm disturbances, so reduce their consumption.
*Prices are presented for informational purposes only. The current price list can be found here
Diagnostics
Patients with detected bradycardia are recommended to consult a cardiologist.
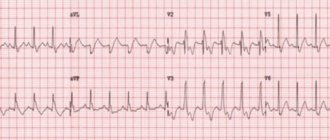
An electrocardiographic study for bradycardia allows you to record a rare heart rate, the presence of sinoatrial or atrioventricular block. If, at the time of ECG registration, episodes of bradycardia are not detected, 24-hour ECG monitoring is resorted to.
For the organic form of bradycardia, an ultrasound of the heart is performed. Ultrasound echocardiography determines a decrease in ejection fraction of less than 45%, an increase in heart size, sclerotic and degenerative changes in the myocardium. Using load bicycle ergometry, the increase in heart rate in connection with a given physical load is assessed.
general information
Modern medicine does not identify a decrease in heart rate as an independent disease, but regards it as a symptom of certain pathological processes. As a rule, in children (including newborns) and adolescents, a sinus form of cardiac bradycardia is detected, which may also be accompanied by arrhythmia.
Assessing the presence or absence of pathology requires an integrated approach, since heart rate norms depending on age are only average values.
Symptoms of a weak (slow) pulse
A 10% decrease in heart rate does not affect your well-being in any way. When the pulse reaches 40 beats/min, symptoms appear:
- weakness;
- dyspnea;
- darkening of the eyes;
- fainting state;
- fainting or loss of consciousness.
In the early stages, a decrease in heart rate may seem like a normal ailment or may be asymptomatic. Therefore, at the first symptoms, measure your blood pressure and pulse. If you notice a deviation from the norm, consult a doctor. At the cardiology center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, you will be offered several heart research programs and will conduct the necessary examinations to determine the cause of a weak pulse.
Prognosis and prevention
The prognosis for bradycardia in a child depends on its cause and severity. In some cases, it is enough to adjust lifestyle or hormonal status to normalize heart function, while in others complex treatment and lifelong monitoring are required. Prevention of the development of pathology includes, first of all, teaching the child to a healthy lifestyle, prevention and timely treatment of diseases that can provoke this condition.
If your child or teenager is experiencing bradycardia, do not wait for the disease to progress; make an appointment with the pediatric cardiologists of the SM-Doctor clinic. You will receive a comprehensive examination, modern and effective treatment if necessary, as well as regular supervision by an experienced specialist.
Disturbances of atrioventricular and intraventricular conduction
Heart block
- slowing down or interrupting the conduction of an impulse through a certain area of the conduction system of the heart. In some cases, the disorder leads to a lack of bioelectrical activity and cessation of heart function.
Atrioventricular block (AV block)
- disruption of the conduction of impulses from the atria to the ventricles. AV blockades can be congenital or acquired, transient or permanent. The causes of acquired AV blocks and symptoms are in many ways similar to SSSS.
There are three degrees of AV block:
- 1st degree - each impulse is carried out from the atria to the ventricles, but more slowly. As a rule, it is asymptomatic and is detected during electrocardiography or 24-hour ECG monitoring. A diagnostic sign is a prolongation of the PQ interval of more than 200 ms on the ECG;
- 2nd degree - the conduction of impulses from the atria to the ventricles is periodically interrupted. Divided into types 1 and 2. Symptoms may occur: episodes of weakness, darkening of the eyes, dizziness. In cases of advanced AV block of the 2nd stage, when several impulses in a row do not reach the ventricles, fainting may occur. ECG sign - periodic loss of the ventricular QRS complex;
- 3rd degree - complete absence of conduction of impulses from the atria to the ventricles. In this situation, the atria and ventricles contract each in its own rhythm. On the ECG, P waves and ventricular QRS complexes are not related to each other; the frequency of the atrial rhythm is more frequent than the ventricular one. Depending on the level of blockade, proximal and distal types can be distinguished. Proximal type AV block at the level of the AV node and His bundle is characterized by a high frequency of escape rhythm (usually up to 40 per minute) with narrow or slightly widened QRS. Distal AV block at the level of the His bundle branches is always characterized by widened QRS complexes with a frequency of less than 40-35 per minute. Complete AV block leads to disruption of the blood supply to vital organs, the development of heart failure, and an increased risk of sudden cardiac arrest.
In case of first degree AV block, asymptomatic 2nd degree AV block of type 1, a wait-and-see approach is used with regular diagnostics and treatment of the underlying disease. For AV block of the 3rd degree, 2nd degree of the 2nd type, symptomatic AV block, the main method of treatment is the installation of a pacemaker.