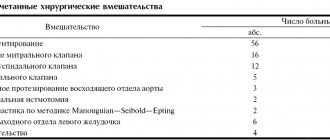
Types of heart valve replacement surgeries
Surgeons perform 2 types of operations. Valve insufficiency is corrected using plastic surgery. When the valve narrows (stenosis), it is completely replaced. The most common surgery is to replace the heart's mitral or aortic valve.
Two types of prostheses are used - biological and mechanical. Biological, porcine valve, is installed in elderly patients. It does not provoke blood clots and lasts 8-15 years. The disadvantage of a porcine prosthesis is the high risk of bacterial inflammation. The mechanical valve has a service life of more than 20 years, but with it the person must take blood thinners for life.
A heart valve is replaced when it wears out. The cost of the operation is determined by the surgeon based on a complete examination of the patient.
Good afternoon dear friends! If you have had heart valve surgery, then this topic is for you. It is known that a radical method of treating patients with acquired heart defects is surgical correction of valvular lesions. Acquired defects often arise due to rheumatism, an infectious process on the heart valves, or age-related calcification of the valves (usually aortic or mitral). The bicuspid aortic valve (found in 1-2% of the population; normally it is tricuspid) wears out faster and often calcifies at 50–60 years of age. Clinically, heart disease is manifested by shortness of breath, fatigue, and palpitations during exercise. If you have complaints, you must consult a doctor for examination. It is important to understand that surgery improves the quality of life. Heart valve replacement surgery is performed under artificial circulation. The goal of valve surgery is to normalize blood flow to the heart. The affected valve is replaced with an artificial one. In the human body, the lifespan of an artificial valve depends on many factors, including the patient’s lifestyle. To maintain health, patients who have undergone surgery to correct valvular heart disease must undergo regular medical examinations and lead a healthy lifestyle. If your condition is satisfactory and there are no complications, you should visit a cardiologist once or twice a year. If the patient’s well-being changes, his follow-up schedule changes, and examinations are carried out depending on his condition. After heart valve surgery, it is necessary to take medications prescribed by your doctor in strict accordance with the recommendations received, and it is important to follow a certain diet. Stopping medications or changing their dosage yourself is strictly prohibited. If you have a mechanical valve implanted, you will be prescribed medications - anticoagulants. They thin the blood to prevent clots from forming. The effect of anticoagulants must be closely monitored using a blood test called a coagulogram. It is important to prevent the development of infection in a patient with an artificial heart valve. Call your doctor immediately if you experience the following symptoms: – Sudden or gradually increasing shortness of breath. – Temporary blindness in one eye or a gray veil before the eyes. – Weakness or numbness in the face, legs, arms, or one side of the body, even if it was temporary. – Slurred speech, even for a short period of time. – Unusually rapid weight gain, fluid retention, swelling of the legs in the ankle area (to control, you need to weigh yourself every day). – Weakness, especially if accompanied by a fever that does not go away within a few days (doctors recommend taking your temperature twice a day for 2-3 weeks). – Chills or fever with a temperature above 40°C. – Unusual bleeding or bruising. – Dark or even black stools, dark urine, also pay attention to the presence of blood in the stool. – A burning sensation or change in urinary frequency. – Loss of consciousness, even for a short period of time. – A sudden change or absence of the normal sound or sensation in your heart valve as it opens and closes, or in your heart rhythm and rate. – Redness, swelling, discharge or discomfort in the incision area. A lifestyle with an artificial heart valve requires giving up bad habits. First of all, you should stop smoking, and it is better to do this even before surgery. Monitor your blood pressure levels. You should limit the amount of salt you consume, reduce the amount of animal fats, fried foods, smoked foods in favor of vegetables, lean meats and fish, all this will help you maintain your health for a long time and avoid new problems.
Indications and contraindications for surgery
Indications:
- congenital heart defects;
- lack of results of drug treatment for chronic heart failure accompanying mitral valve stenosis;
- fainting with aortic stenosis;
- aortic valve stenosis, manifested after coronary artery bypass grafting;
- valve calcification.
Contraindications:
- heart attack;
- stroke;
- extreme degree of heart failure with mitral valve stenosis;
- endocarditis.
A case of successful aortic and pulmonary valve replacement
To the Telemedicine Department of the Scientific Center for Cardiovascular Surgery named after. A.N. Bakulev received a discharge from a 43-year-old patient from Smolensk with a diagnosis of:
Subacute infective endocarditis with damage to the aortic valve and pulmonary valve, caused by Enterococcus faecalis. Arterial hypertension stage 3, risk 4. NC PA, 3 FC. Moderate pulmonary hypertension. Early recovery period of ischemic stroke in the territory of the left middle cerebral artery (cardioembolic variant). Partial motor aphasia, mild right-sided hemiparesis, moderate cognitive impairment. Bilateral segmental pneumonia, resolution stage.
Survey at the place of residence
The patient was admitted to the clinic at his place of residence as an emergency. Upon examination, he complained of severe general weakness, increased body temperature to 39.0°C, and shortness of breath when walking.
Considers himself sick for one week when his body temperature rises to 39.0°C. He was hospitalized in a hospital with a diagnosis of left-sided pneumonia and received treatment. Five days after hospitalization, an acute cerebrovascular accident (ACVA) was detected, and therefore the patient was transferred to the neurological department. Where echocardiography revealed damage to the aortic and pulmonary valves. The diagnosis was made: infective endocarditis. A bacteriological examination of the blood revealed the growth of Enterococcocus faecalis. After antibiotic therapy with improvement, the patient was discharged home.
Three months later, the patient’s condition worsened again: body temperature increased to 39.5-40.0°C, and shortness of breath increased. Hospitalized in the cardiology department of the Special Clinical Hospital. A bacteriological examination of the blood revealed the growth of Enterococcocus faecalis. Antibacterial therapy was carried out for 20 days. At the time of contacting the National Center for Cardiovascular Surgery, the body temperature had returned to normal. Receiving treatment.
The medical history materials were transferred to the TMC for teleconsultation with the Scientific Center for Cardiovascular Surgery named after. Bakulev and solving the issue of surgical treatment.
Research results
Inspection:
The general condition is moderate. Height 176 cm, weight 100 kg. Hypersthenic physique. The skin is pale. There is no swelling. Breathing through the nose is free, respiratory rate is 17 per minute. The chest is normosthenic in shape. Both halves of the chest participate in breathing evenly. Percussion above the lungs - pulmonary sound. The boundaries of the lungs are not displaced. Breathing is vesicular, no wheezing. Heart sounds are sonorous, rhythmic, rough diastolic murmur at all points of auscultation. Heart rate 80/min. Blood pressure is 130/40 mmHg, pulse is correct 80/min. The abdomen is soft and painless. The lower edge of the liver is not palpable, the percussion border is 10*9*8 cm. Pasternatsky's sign is negative on both sides. Urination is free and painless. Consciousness is clear. Correctly oriented in space, time and self.
Research
ECG:
sinus rhythm, heart rate 85/min, normal position of the electrical axis of the heart, decreased recovery processes in the myocardium of the left ventricle.
Echocardiography (EchoCG):
signs of infective endocarditis localized to the aortic valve and pulmonary valve. Dilatation of the left atrium and right chambers of the heart. Monophasic diastolic flow. Moderate mitral, tricuspid, aortic, pulmonary regurgitation. Moderate pulmonary hypertension, Average pressure gradient on the pulmonary artery - 45 mmHg. A small amount of fluid in the pericardium, up to 100 ml.
Ultrasound examination (ultrasound)
abdominal organs: ultrasound signs of moderate hepatomegaly, moderate diffuse changes in the liver. Diffuse changes in the pancreas. Moderate splenomegaly.
Spiral computed tomography (SCT)
abdominal cavity: CT scan - signs of a bilateral segmental inflammatory process (resolution stage).
Consultation with a neurologist: Early recovery period of ischemic stroke in the LSMA basin (cardioembolic variant). Partial motor aphasia, mild right-sided hemiparesis, moderate cognitive impairment.
The documents were sent to the Scientific Center for Agricultural Sciences named after. A. N. Bakulev to resolve the issue of surgical treatment.
Telemedicine consultation at the Bakulev Center
Based on the results of a consultation in the telemedicine department of the National Center for Cardiovascular Surgery, surgical correction of valve pathology under artificial circulation was recommended for emergency indications.
Polyclinic NCSS named after Bakulev
Six days after the telemedicine consultation, an examination was carried out in the clinic of the National Center for Cardiovascular Surgery, the results of which established the diagnosis:
“Secondary infective endocarditis with damage to the aortic valve and pulmonary valve, active phase, subacute course. Aortic valve insufficiency.
Pulmonary valve insufficiency. Arterial hypertension 3 degrees. Condition after acute ischemic cerebrovascular accident. NK 2a degree.”
A decision was made to hospitalize him.
Hospitalization at the Bakulev Center
The patient was hospitalized in the department of emergency surgery of acquired heart defects at the age of 43 years.
Upon inspection:
moderate condition. The severity of the condition is due to heart failure. Consciousness is clear. Activity is somewhat reduced. Hypersthenic. Height 176 cm, weight 94 kg.
The body structure is correct. There is no swelling. The skin is pale, the mucous membranes are pale pink. The tongue is moist and clean.
The chest is of the correct shape. Breathing is harsh, weakened on the left in the lower parts, no wheezing, respiratory rate (RR) 18/min. Heart sounds are muffled, rhythmic, heart rate (HR) 80 beats/min. Diastolic murmur is on the pulmonary artery, systolic-diastolic murmur is on the aorta. Blood pressure 120/80 mmHg. The liver is located on the right, not enlarged. The spleen is not palpable. Physiological functions are normal. Pasternatsky's symptom is negative on both sides.
Examination in the department
ECG:
sinus rhythm, normal position of the electrical axis of the heart. Heart rate 75 beats per minute.
EchoCG:
| LP | 4.3 | LV: | CSR | 48 | KDO | 188 | EF 74% |
| MK: | PMS is compacted | FC 35mm | Regurgitation stage 1 | TK: | not changed | ||
| AK: | FC 22mm. tricuspid, the valves are compacted, signs of destruction of the valves, vegetation, perforation. Regurgitation grade 3-4. | ||||||
LA - left atrium, LV - left ventricle, ESV - end-systolic volume, EDV - end-diastolic volume, EF - ejection fraction, AK - aortic valve, FC - annulus fibrosus, MK - mitral valve, TC - tricuspid valve, PMS - anterior mitral valve.
X-ray:
in the lower lobe on the left there is an infiltration measuring 4.5*2.5 cm, in the pleural cavity on the left there is a minimal amount of fluid, the pulmonary pattern is enhanced. TTI = 51%.
On the fourth day of hospitalization, surgery was performed:
aortic valve replacement with a mechanical prosthesis MIX No. 25 with sanitation of the fibrous ring; pulmonary valve replacement using a mechanical prosthesis MICS No. 25 with sanitation of the fibrous ring; suturing of the oval window, under IR, hypothermia and FHKP.
Postoperative period and discharge
The postoperative period proceeded without complications. Enterococcus faecalis was isolated from cultures of intraoperative material.
EchoCG:
PV = 60%.
Aortic valve prosthesis: leaflet movement is normal, peak gradient on the prosthesis is 19 mmHg;
Pulmonary valve: peak gradient on the prosthesis is 13 mm Hg. There is no free fluid in the pericardial cavity.
ECG:
sinus rhythm. There are no rhythm or conduction disturbances.
Analyzes
blood and urine without pathology.
X-ray:
in dynamics there is less enhancement of the pulmonary pattern; on the right there is a rough “heaviness” in the area of the apex of the heart. There is no fluid in the pleural cavities.
The patient was transferred from intensive care on the second day after surgery in satisfactory condition.
Doesn't have a fever. The skin is clean. The breathing in the lungs is harsh, there is no wheezing. Heart sounds are rhythmic, the melody of the prosthesis, heart rate = 80 beats/min. Blood pressure = 120/75 mm Hg. The liver is not enlarged. Physiological functions are normal. Postoperative wound without signs of inflammation.
On the eighth day after surgery, in satisfactory condition, the patient is discharged home with recommendations: observation by a cardiologist at the place of residence; limiting physical activity; continue taking prescribed medications; EchoCG monitoring after one week for separation; limiting fluid intake to 1.5 liters per day for a month; control of prothrombin index; a general blood and urine test once a week and control at the clinic of the Scientific Center for Cardiovascular Surgery every year. Rehabilitation in a cardiological sanatorium.
Description prepared by:
Makarenko Maria Vladimirovna
Operation technique
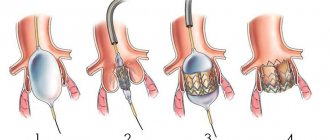
The patient is given general anesthesia. After opening the chest, the patient is connected to a heart-lung machine. Mitral valve replacement involves opening the left atrium, and aortic valve replacement involves opening the aortic wall. The doctor removes the affected valve and sews in a new one. The duration of the operation is 3 - 6 hours.
If such surgery is contraindicated for the patient, aortic heart valve replacement can be performed endovascularly or minimally invasive surgery can be used.
Mitral valve: new life!
Details Published on November 10, 2020
In the cardiac surgery departments of the V.P. Polyakov widely use various techniques for mitral valve reconstruction.
Mitral valve reconstruction is considered worldwide to be the optimal surgical treatment for mitral valve dysfunction for any etiology of the disease.
Why is the function of the mitral valve impaired?
The most common causes of mitral valve dysfunction are: • Connective tissue dysplasia (CTD) • Coronary heart disease (CHD) • Chronic rheumatic heart disease • Infective endocarditis
Why reconstruction and not prosthetics?
The main advantages of mitral valve reconstruction over replacement:
Preservation of heart function!
By restoring the valve's original structure, surgeons can better preserve the heart's natural shape and function.
Freedom from taking medications throughout your life!
Patients who have had a mitral valve replacement must take blood thinners for the rest of their lives. These medications often cause a variety of adverse side effects and are best avoided if possible. In contrast, such drugs are not required in patients who have had valve function restored.
Longer service life!
A number of scientific studies have shown that 15 years after heart valve reconstruction in 82–87% of patients, its function is not impaired. For prosthetics, this figure is 72–82%.
In addition, biological prosthetic heart valves made from animal tissues are subject to degradation after 10–15 years (or even earlier!) (they fail due to changes in the structure of the valve leaflets). In such a situation, a repeat operation to replace the heart valve is necessary. Risk of surgery! The average mortality rate during mitral valve reconstruction surgery ranges from 1 to 2%, compared with 5 to 7% for replacement (Society for American Thoracic Surgeons 2021 Harvest 1 Executive Summary). As the head of the cardiac surgery department No. 11 of the Regional Clinical Children's Hospital named after V.P. explains. Polyakova Dmitry Valerievich Kuznetsov , timely surgical intervention allows you to preserve your own valve, restoring its function to almost all patients with STD or IHD! With infective endocarditis, this figure is somewhat lower and is about 40%, it all depends on the extent of destruction of the valve structures by the infectious process. Most often, patients are admitted with an advanced pathological process, when infectious agents have destroyed most of the valve structures. In such a situation, only its replacement is possible. And earlier diagnosis of infective endocarditis in the initial stages of the disease at the prehospital stage, when the structures of the mitral valve have not yet been destroyed, can increase the chances of restoring the valve structure without replacing it in patients. Patients with chronic rheumatic heart disease are the most difficult in terms of prospects for mitral valve reconstruction, since the pathological process in them, as a rule, lasts for years and proceeds unnoticed by the patients. And they come to the attention of cardiac surgeons with already greatly altered structures of the mitral valve, so it is almost impossible to restore it. But even in such situations, 10–20% of patients manage to undergo valve reconstruction without replacing it!
Important!
Employees of the cardiac surgery departments of the V.P. Polyakov Regional Clinical Children's Hospital constantly evaluate not only the immediate, but also the separate results of reconstructive operations on the mitral valve in their patients. After 5–10 years, in 90% of patients the function of the reconstructed valves is not significantly impaired and does not require repeated surgical intervention.
Consequences and rehabilitation in the postoperative period
After the operation, the patient is in the intensive care unit. Doctors monitor the patient’s condition, as negative consequences are possible and he will need rehabilitation . On the first day, there may be complications such as internal bleeding, thromboembolism, cardiac arrhythmias, infective endocarditis, and heart attack (in less than 5% of cases). After two days, the patient is allowed to get up and walk. At this time, he may complain of chest pain and increased fatigue. The patient is discharged home within 4 to 10 days, where he is under the supervision of a doctor.
The postoperative period lasts 3 weeks, during which temporary disturbances in sleep, vision, appetite, and swelling of the legs are possible. A month later the patient undergoes a full examination. The cardiologist calculates adequate physical activity, diet, and prescribes supportive treatment. It is important to perform physical therapy to strengthen the heart muscle.
Personal experience“There are jokes about a ticking bomb”: I have a mechanical heart valve
I was born with a ventricular septal defect. Prematurity affected my general well-being, so I spent the first months of my life within the walls of the hospital.
I don’t remember the first operation at all - it was performed when I was three years old. The septal defect was removed, but then, for an unknown reason, aortic valve insufficiency developed. They tried to eliminate it when I was six by performing a second operation, but in the end they simply delayed replacing the valve with an artificial one. The heart was given several more years to grow to the size of an adult organ. As far as I understand, in case of severe valve insufficiency there is no option “not to operate”, otherwise you greatly risk your health and well-being. You can postpone it, but this entails a whole list of restrictions - depending on the situation, sports may be prohibited, and you also need to undergo regular examinations. At the same time, I can’t say that I felt particularly bad, but perhaps I’ve already forgotten. I remember that I was forbidden to do physical education at school, so instead I read comics or talked with my classmates.
The second operation was more difficult than the first: I was already of a conscious age. It was impossible to get sick or catch a cold before it, so I was transferred to home schooling for six months. My classmates - I don’t know, on their own or on the instructions of the class teacher - made a whole pack of postcards with drawings and words of support. Now, after many years, I find it very sweet.
My memories of how everything went are vague - I remember how I was taken to a cold operating room, where there were bright spotlights. How they performed a puncture to remove fluid from the lungs, how several doctors held me while one punctured my lung through my back. How they took me for an x-ray to the intensive care unit, at the entrance to which, instead of tiles, there was thick glass, under which lay various Kinder Surprise toys. How my grandmother and aunt brought the newest and coolest Barbie dolls every time they visited. I also remember that my mother lived in the same room with me and often went away for a long time to smoke. She was also very thin, and amid constant stress over my health, she developed severe anxiety and agoraphobia. I was a kind of staunch soldier who, at six years old, instead of being frightened by my mother’s breakdowns, I simply calmly went to the nurse and asked to call a doctor and give her a sedative.
The third planned operation was performed when I was twelve. I went home schooling again for six months - I don’t know if this was a condition on the part of the doctors or if my mother decided that it was better this way. I wasn’t upset - my friends came to my house, my first normal mobile phone appeared, Internet friends and game consoles, so I never got bored. Now I realize that my parents were most likely worried about the outcome of the operation and spoiled me with gifts while they had the opportunity. I then told them all that I wanted a dog, and we went to choose a puppy. They took him a month after the operation. I don’t want to think that maybe this is how the parents tried to prepare for the worst.
Study of quality of life in elderly patients after heart surgery
In recent years, the elderly population has increased significantly in developed countries. According to demographers, further aging of the population will be observed in the near future, associated with an increase in overall life expectancy and a decrease in the number of young people. For example, in the Russian Federation in 2000 there were about 18 million people over 65 years old, and in 2021 there will be 21 million people. (Table 1) [36]; Now in Germany, the population of 82 million accounts for 17% of the elderly, and by 2021 the number of elderly people will rise to 22% of the expected total population of 75 million. In the USA, by 2021 the number of elderly people is expected to increase by 5 million [12, 32 ] (Fig. 1).
| Rice. 1 . Population growth over 65 years of age |
Table 1 . Change in the share of elderly people in the Russian Federation 2000G2020 [36] Years
| 2000 | 2005 | 2010 | 2015 | 2020 | |
| Population of the Russian Federation over 65 years old (thousands) | 18 192 | 20 021 | 18 235 | 19 106 | 21 542 |
| Total population of the Russian Federation (thousands) | 145 491 | 140 920 | 136 976 | 133 314 | 129 687 |
| Percentage of the elderly population of the Russian Federation from the total population | 12,5 | 14,2 | 13,3 | 14,3 | 16,6 |
As a result of this phenomenon, cardiologists and cardiac surgeons are increasingly encountering elderly patients in their practice. There are features of the management of elderly cardiac and cardiac surgical patients, determined both by the specifics of the underlying disease and by concomitant diseases [3, 16].
Experts' opinions on the advisability of surgical interventions in older people often differ. Should we focus on conservative therapy or recommend surgical treatment? Iskandrian et al. consider performing surgical operations on the elderly unjustified [21]. According to some authors, early mortality after aortic valve replacement is higher in elderly patients [17]. Others consider advanced age a risk factor for surgical interventions, whether cardiac [13, 26] or other organs [18, 35].
Table
2 demonstrates surgical mortality in patients of different age groups after cardiac surgery: coronary artery bypass grafting (CABG), aortic valve replacement (AVR) and mitral valve replacement (MVR), mitral valve plastic (MVP) [27]. Table 2 . Surgical mortality in patients of different age groups after cardiac surgery (from the database of the Association of Thoracic Surgeons, 1998)
| 51 — 60 | 61 — 65 | 66 – 70 | 71 — 80 | 81 – 90 | ||
| CABG | 1,1 | 1,6 | 2,1 | 2,9 | 4,4 | 7,2 |
| PACK | 2,3 | 2,2 | 2,3 | 3,6 | 4,7 | 7,7 |
| PMK | 3,4 | 2,4 | 3,9 | 5,1 | 8,4 | 16,2 |
| Pl.MK | 0,3 | 0,3 | 0,6 | 1,9 | 1,7 | 20,0 |
| PAK+PMK | 2,2 | 6,0 | 7,1 | 10,8 | 13,2 | 20,0 |
| CABG+PACK | 3,6 | 2,5 | 4,6 | 5,9 | 7,3 | 10,2 |
| CABG+MVP | 6,7 | 7,2 | 8,9 | 12,2 | 14,4 | 21,5 |
| AKSh+Pl.MK | 4,5 | 5,7 | 6,4 | 9,7 | 11,4 | 15,1 |
However, there is now an increasing number of researchers who believe that surgical treatment is a priority. Thus, it is recognized that valve replacement surgery, primarily aortic valve replacement, in patients over 70 and even 80 years of age is the operation of choice, providing acceptable operative mortality and a significant improvement in the quality of life of these patients in the long-term postoperative period [3].
In general, the effectiveness of a particular treatment method is assessed using various criteria. This includes assessing objective data on the patient’s condition and calculating statistical parameters such as mortality, re-operation rates, etc. [4, 9]. However, all these criteria for survival and life expectancy leave uncovered the most important aspects of a person’s life, namely everything that defines him as an active member of society. These factors are assessed by quality of life.
Despite the fact that the term “quality of life” entered scientific terminology in the mid-80s, there is still no clear definition of this concept [34]. Quality of life characterizes various aspects of human life and depends on many factors, from personal to socio-economic. The medical, narrower concept is closely related to the concept of health. The term “quality of life” has been proposed to assess the condition of people with a common disease.
Currently, quality of life is becoming an independent criterion for assessing the effectiveness of treatment, complementing the results of clinical and economic data [7, 19].
Of course, a necessary condition is an adequate method for studying it, which is greatly complicated by the vagueness in the definition of this concept.
Currently, there are a large number of methods for assessing quality of life. All of them are divided into general ones, i.e. used to assess the quality of life in any disease, and specific, intended for patients with a specific disease [7]. They reflect subjective indicators B perception of health status and assessment of the severity of symptoms by the person himself. Based on the methods, questionnaires are constructed, which are filled out either directly by the patient, or by a doctor or specially trained personnel. However, the abundance of methods for assessing quality of life makes it very difficult to determine the reliability of research results on the same problem.
The most commonly used general methods are Sickness Impact Profile (SIP), Nottingham Health Profile (NHP), Stanford Physical Activity Recall [6, 31, 33].
The SIP technique demonstrates the impact of health status on sleep, eating, housekeeping ability, etc., and consists of 136 questions. The NHP technique evaluates the role of symptoms in the patient’s health. The questionnaire of this technique is short and easy to fill out. The Stanford Physical Activity Recall technique has become widespread due to its ability to be used in large-scale studies.
One of the most popular general methods currently is the Medical Outcomes Study 36 – Item Short Form Health Survey [4, 5]. It is called the “gold standard” of general techniques. Thus, when compared with NHP, greater sensitivity of SF-36 was noted. The questionnaire consists of 36 questions with various answer options. The results are presented in the form of points (0B100) and are distributed across 8 scales; a higher score indicates a higher QoL score. As a result, a quantitative assessment of the following categories is made:
- Physical Functioning (PF) - physical functioning - reflects the degree to which the health condition limits the performance of physical activities (self-care, walking, climbing stairs, carrying heavy objects, etc.).
- RoleBPhysical (RP) – the influence of physical condition on role functioning (work, performing usual activities).
- Bodily Pain (BP) – the intensity of pain and its impact on the ability to perform daily activities.
- General Health (GH) – general health status – the patient’s assessment of his current condition.
- Vitality (VT) - vitality (feeling full of strength and energy or, on the contrary, exhausted).
- Social Functioning (SF) – social functioning is determined by the degree to which a physical or emotional condition limits social activity (communication).
- RoleBEmotional (RE), the influence of emotional state on role functioning, involves assessing the extent to which emotional state interferes with the performance of work or other daily activities.
- Mental Health (MH) - mental health assessment B characterizes mood (presence of depression, anxiety, general indicator of positive emotions) [8].
Assessment of quality of life is widely used by many researchers as a criterion for the effectiveness of heart surgery, including in elderly patients.
Currently, cardiac surgery for the elderly is receiving more and more attention in developed countries. This problem is also developing in our country, as evidenced by the increasing number of studies on this topic. So, L.A. Bokeria et al. When analyzing the results of operations for acquired heart defects in elderly patients over 65 years of age, they conclude that age should in no way be a reason for refusing surgery [1]. According to G.E. Gendlina et al. [3], the long-term indicators of the condition and hemodynamics of patients over 60 years of age are practically no different from those of younger patients, and the age of patients with acquired heart defects is not a contraindication to open heart surgery.
Optimistic forecasts are made by V.S. Rabotnikov [10] and Yu.L. Shevchenko [11] and colleagues in a study of short-term and long-term results of coronary artery bypass surgery in elderly patients.
Foreign specialists obtain similar results. According to the results of the analysis of the postoperative period and assessment of the quality of life in 11 patients over 80 years of age who underwent abdominal aortic aneurysmectomy, the mortality rate was 9% (one patient out of 11). The effectiveness of the operation was assessed according to several parameters, including quality of life [20 ].
Levin et al. found that aortic valve repair performed in patients over 86 years of age was accompanied by an improvement in clinical symptoms and quality of life [24].
Of great interest is the study by Kwok L. Yan et al. [23]. They observed 543 patients over 65 years of age for two years after cardiac surgery - 400 of them underwent CABG surgery, 61 underwent CABG with plastic surgery, 82 underwent correction of valve pathology. Repeated operations were required in 59 patients. The quality of life was assessed using the SF-36 system.
Rice. Figure 2 illustrates patients' assessment of health status before and after surgery B at 3, 12, 24 months. respectively. Compared with the state before surgery, all patients noted an improvement in all indicators in all categories after surgical treatment.
| Rice. 2 . Patient assessment of health status before and after surgery |
Note : a - before surgery;
b - after surgery. Extensive experience in open heart surgery in elderly patients has been accumulated at the Scientific Center for Cardiovascular Surgery named after. ON THE. Bakulev RAMS. Work is underway to study quality of life indicators in elderly patients after cardiac surgery [2].
In Fig. Table 3 presents comparative indicators of quality of life in patients over 65 years of age who underwent mitral valve replacement, aortic valve replacement, tricuspid valve replacement, combined operations, as well as interventions combined with coronary artery bypass grafting at the Scientific Center for Cardiovascular Surgery named after. N.A. Bakuleva RAMS.
| Rice. 3 . Comparative indicators of QoL |
Similar data were obtained from other studies of the quality of life in centenarians after heart surgery. Thus, Christian Stoll et al. [15] studied the quality of life of patients with an average age of 66 years after cardiac surgery: the improvement in the quality of life was confirmed by the majority of subjects. According to Shigemitsu, who studied the quality of life of patients over 80 years of age after heart surgery using the NHP technique, there was a significant improvement in quality of life [29]. Similar conclusions are drawn by Sundt [30] regarding aortic valve replacement surgery in patients over 80 years of age. Shapira et al. assess the long-term results of valve surgeries in patients over 75 years of age and quality of life as excellent [28]. The results of many other studies indicate positive results of operations in the elderly [14, 22, 25].
Thus, old age as such is not an obstacle to surgery. Despite the fact that this population is especially difficult for surgery in general and cardiac surgery in particular, due to the characteristics of the underlying disease, duration, and the presence of concomitant pathologies, cardiac surgery is often the method of choice for elderly patients. Proof of this, along with other criteria, is the improvement in the quality of life, which is a full-fledged, independent criterion for the effectiveness of cardiac surgery in the elderly.
Hospitalization at the Bakulev Center in the emergency surgery department for acquired heart defects
At the time of hospitalization in the NCPPS department, the patient was 68 years old.
In the hospital during examination
The condition is of moderate severity. Height 150 cm, weight 75 kg. BSA = 1.78. BMI = 33.33.
The body structure is incorrect. The development of subcutaneous tissue is moderately increased. There is no swelling. The color of the skin is acrocyanosis. The chest is of the correct shape. Respiratory rate 20/min. Breathing is harsh, carried out in all departments. No wheezing. Heart sounds are muffled and arrhythmic. Systolic murmur in the second intercostal space on the right, carried out to the vessels of the neck. Heart rate = 100 beats/min. Blood pressure: on the left arm - 120/60 mm. rt. Art. Satisfactory filling pulse = 100 beats/min.
The liver is not enlarged. The stomach is soft. Physiological functions are normal.
Instrumental studies
EchoCG:
| LP | 48 mm | LV: | CSR | 49 | KDO | 104 | EF 53% |
| MK: | not changed | FC 34mm | Regur. 1 tbsp. | TK: | Regur. 2 tbsp. | ||
| AK: | FC 20mm. Double-leaf. Calcification of the valves. Systolic opening is reduced. Peak gradient on the valve is 110 mmHg. Regurgitation of the 1st degree. | ||||||
| Aorta: | Ascending: 37 mm | ||||||
LA - left atrium, LV - left ventricle, ESV - end-systolic volume, EDV - end-diastolic volume, EF - ejection fraction, AK - aortic valve, FC - annulus fibrosus, MK - mitral valve, TC - tricuspid valve.
Angiocardiography:
Cardiac ischemia. Right type of blood supply to the myocardium. Anomalous origin of the right coronary artery from the left coronary sinus. Stenosis of the anterior interventricular branch in the middle third is 50%.
ECG:
atrial fibrillation with heart rate 70-90 beats/min.
Based on the results of examinations in the hospital, a decision was made to perform radical correction of the defect under conditions of artificial circulation and hypothermia.
On the seventh day of hospitalization, an operation was performed - replacement of the aortic valve with a biological prosthesis Carpentier-Edwards Perimount No. 21 supraannularly with ligation of the left atrial appendage, under conditions of bypass, hypothermia and PCCP.