Myocardial infarction: clinical picture, diagnosis, treatment
Acute myocardial infarction (MI) is a clinical syndrome that occurs as a result of damage to the heart muscle when there is a discrepancy between the myocardial oxygen demand and the ability to deliver it. In this case, necrosis of cardiomyocytes occurs in the damaged area simultaneously, which distinguishes this process from other forms of myocardial damage.
Etiology and pathophysiology. Risk factors are hypercholesterolemia, diabetes mellitus, arterial hypertension, sedentary lifestyle, family history, smoking and others.
The main process in the process is considered to be atherosclerosis of the coronary arteries, which includes rupture or deendothelialization of the atherosclerotic plaque, thrombosis, vasoconstriction, often against the background of inflammation. An important role is also played by impaired blood clotting, a decrease in coronary blood flow and its insufficient compensation by collateral circulation, impaired prostaglandin metabolism, the function of the kallikrein-kinin system, and immunological disorders. Regardless of the cause, MI is characterized by the onset of irreversible death of myocardial cells. The infarct zone, which initially covers the subendocardial layer of the myocardium, begins to spread to deeper layers, heading towards the epicardium. Even with total occlusion of the coronary vessel supplying the infarcted area, some antegrade blood flow is observed, which may allow viable cardiomyocytes to remain in the affected area, so it is believed that there is a time period of up to 6-12 hours when it is possible to influence the size of the necrosis area by increasing blood flow in damaged area.
In more than 50% of patients, total coronary occlusion develops in the area of a pre-existing atherosclerotic plaque. Total occlusion most often develops in the proximal segments of large arteries, which subsequently manifests itself on the ECG as pathological Q waves. In the absence of total thrombotic occlusion of the coronary vessel, Q-non-forming MI occurs more often (according to the ECG).
The development of MI is accompanied by impaired systolic and diastolic function and left ventricular (LV) remodeling. Violation of systolic function is due to the fact that the necrotic area of the myocardium does not participate in heart contraction, while in the undamaged nearby zone there is compensatory hyperkinesia. Diastolic dysfunction is associated with decreased elasticity and distensibility of the myocardium. As a result, LV diastole is incomplete, the myocardium is not relaxed enough, and end-diastolic pressure increases. These disorders occur when less than 10% of the mass of the left ventricular myocardium is affected. LV remodeling is caused by thinning of the myocardium and a decrease in myocardial tone in the area of necrosis, compensatory expansion of the LV cavity, the development of a state of hibernation in the peri-infarction zone, activation of the circulating and local renin-angiotensin and sympathoadrenal systems, and hyperproduction of endothelin. Cardiac remodeling after MI can be adaptive or maladaptive. The adaptive nature is manifested in reducing the size of the LV, maintaining satisfactory contractility of the LV, and stabilizing myocardial stress. The hemodynamically favorable shape of the LV is maintained, satisfactory contractility of the LV is maintained and myocardial stress is stabilized. The maladaptive nature of the LV remodeling process consists of progressive LV dilatation with a transition to a hemodynamically unfavorable spherical heart shape, which leads to the development of a restrictive type of LV diastolic filling. This type of dysfunction is a powerful predictor of cardiovascular mortality.
Clinical picture. Manifestations of MI have many variants. From an asymptomatic course and episodic discomfort in the heart area to a full-blown pain attack with various rhythm and conduction disturbances. More often described are sensations of “pressure,” “heaviness,” and “burning” in the central part of the chest with irradiation to the shoulder girdle, arm, jaw, and epigastric region. The patient is restless, puts his hand to the sternum (Levine's sign). For an elderly patient with multiple concomitant pathologies, MI often manifests itself in signs of heart failure (increasing shortness of breath, edema, palpitations, atypical anginal pain).
Physical examinations vary from complete normality to pronounced abnormalities (expansion of the apex impulse, appearance of 3rd and 4th tones, weakening of tones, appearance of moist rales in the lungs, etc.). None of these signs confirms, but does not exclude the presence of MI. Diagnosis of MI is based on identifying markers of damage to the heart muscle.
Markers of cardiomyocyte damage. Currently, the most convincing marker is troponin. It has a higher sensitivity to MI than the MB fraction of creatine phosphokinase (MB-CPK). Modern methods of analysis make it possible to give troponin almost absolute cardiac specificity, but given this quality, troponin can also be elevated in non-ischemic myocardial damage. Therefore, only an integrated approach (clinical data, echocardiographic, etc.) can prove acute myocardial ischemia and the development of MI. Troponin levels rise in the first 4–6 hours and remain elevated for 8–12 days. The duration of detection of the marker makes it possible to diagnose MI at a later stage, without testing lactate dehydrogenase (LDH). For more accurate orientation in the timing of MI, it is advisable to study “short-lived” markers of necrosis. An “early” marker of myocardial necrosis is an increase in CK-MB activity. CF-CPK activity increases in the first hours of myocardial damage and exceeds normal levels between 6–12 hours of illness, reaching a peak at 18–24 hours of illness, and by 48 hours the marker levels return to normal. It is necessary to remember other reasons for the increase in CF-CPK: damage to skeletal muscles, chronic myopathies, renal failure, hypothyroidism due to decreased clearance, and also that the ratio of CF-CPK and total CPK is not considered a criterion for diagnosing MI.
Electrocardiography. The most significant signs of MI are changes in the ST segment (rising with convexity upward). For lower localization of MI, an ECG should be recorded on the right side of the chest in leads V3R or V4R. Circumflex occlusion is characterized by changes in the so-called posterior leads (V7–V9), most often in the form of the appearance of a pathological Q wave. However, the above signs cannot be considered 100% mandatory. In most cases, there are no typical ECG changes, which may be due to the presence of intraventricular conduction disturbances or isolated ST segment depression.
Echocardiography (EchoCG). The diagnostic accuracy of echocardiography depends on the quality of the resulting image. The absence of pathology on echocardiography cannot serve as a basis for excluding coronary heart disease or necrosis of the heart muscle. EchoCG does not allow distinguishing a fresh focus of asynergia from a zone of post-infarction cardiosclerosis. The study is indispensable for excluding complications of myocardial infarction and concomitant pathologies.
Treatment. To achieve the maximum positive result, treatment should begin as early as possible, starting from the first hour of the disease, which will allow for a significantly better prognosis. Reperfusion therapy by thrombolysis or primary angioplasty should be performed as early as possible. It has been proven that early treatment leads to a significant reduction in mortality in all forms of MI. Primary angioplasty on the infarction-associated artery in the first hour of the disease allows you to restore natural myocardial perfusion in the damaged area. The later the reperfusion is performed, the higher the mortality rate. Currently, the availability of angioplasty remains low.
In 1996, the European Society of Cardiology and the American College proposed recommendations for the treatment of patients with acute myocardial infarction, consisting of a number of fundamental positions.
1. Pain syndrome is of utmost importance for the course of MI. The more pronounced and prolonged the pain syndrome, the greater the risk of developing severe complications. In the absence of hemodynamic contraindications, a sublingual form of nitroglycerin (NTG) can be used to relieve an anginal attack. In some cases, this makes it possible to obtain regression of acute ischemic changes on the ECG. In this case, NTG should be used with caution in lower localization of MI, since severe arterial hypotension may develop. IGT can also cause circulatory collapse and a sharp decrease in heart rate (vasovagal reaction). If the effect of sublingual NTG is obtained, intravenous infusion of this drug in low doses (5–10 mcg/min) can be used. The use of NTG does not exclude the use of analgesics. The use of powerful vasodilators (for example, calcium antagonists) is not recommended due to the occurrence of severe hypotension and reflex tachycardia. In the absence of a rapid analgesic effect from IGT, narcotic analgesics are prescribed - morphine hydrochloride IV up to 10 mg with repeated administration of the drug until the pain syndrome is completely relieved. In addition to the main effect, morphine helps to reduce pre- and afterload on the heart and reduces pressure in the vessels of the pulmonary circulation. The main side effects are hypotension and relative bradycardia, depression of the respiratory center, nausea and vomiting. Promedol is also used for pain relief.
To enhance the analgesic effect, a combination of morphine and an antipsychotic is used, most often droperidol, which also has a powerful antiemetic effect. For elderly patients, these regimens should be used with caution due to concomitant pathology, since respiratory dysfunction is often possible. For this age group of patients, it is recommended to use a combination of a narcotic analgesic and a tranquilizer, for example, Fentanyl 0.005% 2 ml and Seduxen 0.5% 2 ml.
A great achievement in the analgesia of intractable anginal attacks has been the epidural block. Widespread use is difficult due to the development of specific complications and the presence of technical difficulties in its implementation.
The use of inhalational anesthetics is currently rarely used, only for certain indications (carrying out cardioversion, artificial ventilation, performing painful manipulations).
2. Restoration of blood flow (recanalization) through the infarction-associated artery significantly reduces the size of the myocardial lesion area. The effectiveness of thrombolytic therapy (TLT) directly depends on the time of initiation of treatment. It is desirable that the time to seek help and start TLT does not exceed 90 minutes. The indication for TLT is the presence of a shift of the ST segment upward from the isoelectric line of more than 0.1 mV in at least two adjacent ECG leads or bundle branch block in patients admitted in the first 12 hours after the onset of symptoms of MI. However, if the pain and the above changes on the ECG persist, it is considered advisable to perform TLT at a later date (up to 24 hours after the onset of the disease). By blockade of the bundle branch we mean new or suspected new complete blockade of the left bundle branch, which complicates the interpretation of the ECG. The most accessible drug with proven effectiveness is streptokinase. The drug activates plasminogen indirectly. The drug should not be prescribed to patients who have had a previous severe streptococcal infection or who have been administered this drug within the past 5 to 6 months. Rapid administration of streptokinase can cause a sharp decrease in blood pressure. The recommended dose of streptokinase is 1,500,000 units per hour.
Urokinase is a direct plasminogen activator, has a short half-life, and causes more rapid restoration of patency of the infarct-associated artery than an equivalent dose of streptokinase. The recommended dose is 2,000,000 units as a bolus and 3,000,000 units as an intravenous drip over 90 minutes.
Tissue plasminogen activator (tPA) is considered a fibrin-specific plasminogen activator. Compared with streptokinase and urokinase, tPA promotes earlier restoration of the patency of the infarction-associated artery, perhaps this factor is responsible for reducing mortality when it is used. The regimen for prescribing tPA is 100 mg IV over 3 hours: 10 mg bolus, then 50 mg during the first hour and another 40 mg over the next 2 hours. If the patient's body weight is less than 65 kg, the drug is prescribed at a dose of 1.25 mg/kg (over 3 hours), with 10% of the total dose being administered as an initial bolus. The use of higher doses (more than 100 mg) of tPA is associated with the risk of intracranial bleeding.
Over time, other tPAs with a slightly different molecular structure were synthesized: reteplase, tenecteplase.
Contraindications to the use of TLT are determined by the risk of serious bleeding, especially intracranial bleeding. There are absolute contraindications: active internal bleeding, any vascular episode within the last 2 months, neoplasm of the central nervous system, severe trauma, surgery within 3 months, pregnancy, severe arterial hypertension. Relative contraindications include suspicion of aortic dissection, cardiovascular resuscitation for 2 weeks, malignant neoplasms, peptic ulcer in the acute stage, hemostasis disorders, systemic diseases, endocarditis and a number of other diseases. The issue of performing TLT in older patients should be decided individually, due to the presence of a large number of concomitant pathologies.
Concomitant treatment
Aspirin should be prescribed to all patients with suspected MI, unless there are contraindications. Its positive effect on survival, the incidence of reinfarction and ischemic strokes has been demonstrated both with and without TLT. When Aspirin is combined with TLT, the effectiveness of the latter increases significantly. Aspirin has been proven to inhibit platelet aggregation and accelerate fibrinolysis. Therefore, all patients with MI should be prescribed Aspirin immediately at a dose of 160–325 mg (chewed).
Heparin, when administered intravenously together with plasminogen activators, helps to accelerate the patency of the infarction-associated artery, especially when using tPA. When using streptokinase, intravenous heparin infusion is not so necessary. The standard heparin therapy regimen calls for an initial bolus of 5000 units of unfractionated heparin, followed by an infusion at a rate of 1000 units/hour until the activated partial thromboplastin time (aPTT) is 1.5 to 2 times the baseline value. Due to the difficulty of accurately titrating this form of heparin, it is recommended to use low molecular weight heparins (LMWH) based on the dose per kg of patient weight.
β-blockers reduce the risk of recurrent myocardial infarction in patients treated with thrombolytic therapy. β-blockers reduce the risk of death, modulate neurohumoral and hormonal systems, slow down the remodeling of the cardiovascular system, and normalize the functional state of platelets. It is recommended to use drugs of this group in the first 12 hours after the onset of MI in all patients who do not have contraindications (bronchial asthma, diabetes mellitus, bradycardia, hypotension). Daily doses of metoprolol and propranolol are used.
Angiotensin-converting enzyme inhibitors (ACE inhibitors). Heart failure (HF) is a common complication and one of the main causes of mortality in the acute period of MI and in the long term after its development. The occurrence and progression of HF in patients who have suffered an MI is associated with the process of remodeling of the LV myocardium, the pathophysiological process of which begins already in the first hours of the disease. Damage to the cellular and structural components of the myocardium and expansion of the infarct zone predisposes to LV dilatation and dysfunction, which determines the high mortality of patients with myocardial infarction. Changes in the structure of the LV in the first 3 days, and subsequently the proliferation of fibroblasts and collagen synthesis lead to the progression of cardiac remodeling. An active participant in these processes is angiotensin II, which causes spasm of the coronary arteries, increased heart function, increased myocardial oxygen consumption, and subsequently the proliferation of fibroblasts. Thus, theoretical grounds have emerged for the use of ACE inhibitors in myocardial infarction. ACE inhibitors, by reducing the synthesis of angiotensin II, which causes vasoconstriction of both the arterial and venous vascular beds, help normalize central and peripheral hemodynamics, thereby preventing the development of cardiogenic shock, significantly reducing the load on the heart, and suppress the process of LV remodeling. However, the use of ACE inhibitors in the acute period of myocardial infarction is limited by the risk of reducing systemic blood pressure (BP). In this regard, despite the proven effectiveness of ACE inhibitors, the search for safe drugs of this group, suitable for use from the first day of MI in combination with TLT, has not lost its relevance. Drugs that do not cause a sharp decrease in blood pressure include lisinopril (Diroton). The effectiveness of Diroton as a means of preventing LV remodeling and the development of HF, as well as reducing the risk of death after the development of MI, has been shown in experimental and clinical conditions. Unlike most ACE inhibitors, Diroton does not require biotransformation in the liver to form active metabolites, and also does not contain a sulfhydrophilic group, which is the cause of a number of side effects. The lack of hepatic metabolism in Diroton allows it to be recommended for patients with liver pathology. Diroton reduces the risk of interaction with other drugs that undergo biotransformation in the liver. A study of the effectiveness of Diroton in patients with MI and in the early post-infarction period showed a decrease in mortality and a decrease in heart failure. Diroton has also proven its effectiveness in elderly patients.
Antiarrhythmic drugs. Usually we are talking about the use of Lidocaine, which was previously prescribed to everyone for the prophylactic purpose of stopping ventricular arrhythmias. Subsequently, recanalization of the infarct-associated artery was found to reduce the likelihood of developing such arrhythmias, and routine use of the drug was shown to increase mortality. Lidocaine should be prescribed only for ventricular tachycardia or ventricular fibrillation.
Magnesium sulfate (magnesium sulfate) may be used in the presence of laboratory-proven hypomagnesemia or other specific indications (for example, polymorphic ventricular tachycardia).
N. V. Zhuravleva , Candidate of Medical Sciences O. A. Povorinskaya Russian Research Institute of Gerontology , Moscow
Differential diagnosis of angina and other cardiovascular diseases
Cardiologist of the Department of Cardiology No. 1 Verbitsky V.L.
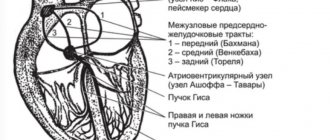
In some patients with a typical clinical picture of angina pectoris and positive stress tests (according to objective criteria), coronary angiography does not find any changes in the coronary arteries; Such patients have no signs of spontaneous angina. In these cases, we can talk about coronary artery disease with unchanged coronary arteries. In the English-language literature, this type of pathology is called “X syndrome.” Special studies show that in these patients the ability of the coronary arteries to dilate is significantly reduced, which is detected when assessing coronary blood flow using argon or rubidium radionuclides under the conditions of a dipyridamole test. When performing a myocardial biopsy in these patients, electron microscopy reveals degenerative changes in cardiomyocytes. Thus, both the decrease in coronary reserve and biopsy data allow us to think of “syndrome X” as the initial manifestations of dilated cardiomyopathy. This diagnosis becomes even more reliable if patients have persistent or transient (appearing under load) blockade of the left branch of the His bundle.
With mitral valve prolapse syndrome, there is a pressing or burning pain in the third or fourth intercostal space to the left of the sternum. Much less often the pain is localized behind the sternum or xiphoid process. Mild pain can last for hours, intensifying after physical and emotional stress. When intensified, the pain can cover the entire heart area. In some patients, the pain is relieved by nitroglycerin. The pain is often combined with cardiac arrhythmias (extrasystole, atrial fibrillation, atrioventricular block). It is believed that mitral valve prolapse predisposes to spasm of the coronary arteries. This syndrome is more common in patients with an asthenic build with a flat chest - with a reduced anteroposterior size. In patients with mitral valve prolapse, abnormalities of the ST segment and T wave are often detected, especially when performing an exercise test. On FCG and during auxultation in patients, a mesosystolic murmur is detected at the apex, which is often preceded by a mesosystolic click. The diagnosis of mitral valve prolapse has improved significantly due to the widespread use of ultrasound methods of cardiac examination in the clinic. It allows you to detect prolapse of one or both mitral valve leaflets into the atrium. Valuable diagnostic data can be obtained by ventriculography. Establishing a diagnosis of mitral valve prolapse does not exclude the simultaneous presence of stenosing coronary atherosclerosis in the patient.
Valvular stenosis of the aortic mouth, like arterial hypertension, leads to overload and hypertrophy of the left ventricle, increasing the myocardial oxygen demand. The shortening of the period of diastolic filling of the left ventricle observed with a defect of this type contributes to a decrease in coronary blood flow. These patients often complain of pain in the heart area. In the early stages of the disease, they have the character of cardialgia, and with severe aortic stenosis, typical attacks of angina occur. If a systolic murmur is heard on the aorta in patients with angina, then it is necessary to carry out all available diagnostic studies aimed at identifying aortic stenosis. The diagnosis of aortic stenosis is made on the basis of the characteristic systolic murmur (diamond-shaped murmur on a phonocardiogram), physical, radiological and electrocardiographic signs of left ventricular hypertrophy. X-rays often reveal calcification of the aortic valve. Echocardiographic data are of great differential diagnostic importance. Detection of aortic stenosis does not exclude the simultaneous presence of atherosclerosis of the coronary arteries. Aortic stenosis in a patient with angina pectoris, combined with attacks of cardiac asthma, has a dire prognosis.
With mitral heart disease, patients often complain of pain in the heart area, in some cases indistinguishable from angina. The cause of this pain may be pulmonary hypertension, characteristic of mitral stenosis, pathogenetically associated with insufficient blood supply to the hypertrophied right ventricle. Sometimes pain sensations have a neurotic basis, but typical attacks of angina pectoris are highly likely to indicate a concomitant stenotic lesion of the coronary arteries of the heart, which is confirmed by coronary angiography data. When carrying out a differential diagnosis of angina pectoris, it is necessary to exclude aortalgia - pain accompanying inflammatory and degenerative diseases of the aorta. With syphilitic aortitis, which is rare in our time, aortic insufficiency occurs; the pathological process also affects the mouths of the coronary arteries of the heart, which can be accompanied by typical attacks of angina. With nonspecific aortoarteritis, typical angina is rarely observed; prolonged pain in the heart area without irradiation is characteristic.
With an aortic arch aneurysm, numerous accompanying symptoms caused by compression of neighboring organs (cough, dysphagia, hoarseness, visual disturbances, fainting, asymmetrical pulse, compression of the superior vena cava) help to make a correct diagnosis. With aortic dissection, the pain is of maximum intensity from the very beginning. The widest irradiation is characteristic: pain, starting behind the sternum, then radiates to the neck, back, abdominal area, along the spine and even to the legs. Spider fingers and other signs of Marfan syndrome may lead the doctor to believe that chest pain is related to aortic dissection, to which these patients are predisposed.
Pain in the heart area is the most common and one of the early symptoms of myocarditis . They are varied, unlike angina pectoris, they last for hours and days. In the acute period of the disease, the intensity of pain may vary, but the pain is almost constant. When diagnosing, it is necessary to take into account the connection with a recent infection, fever, leukocytosis, and enlargement of both ventricles of the heart. With a more or less prolonged course, cardiomegaly and heart failure become obligatory symptoms of myocarditis. Differential diagnostic difficulties more often arise with mild heart damage, when after a sore throat, flu or other infection, unpleasant sensations appear in the heart area, accompanied by changes in the final part of the ventricular ECG complex. Patients have a tendency to tachycardia and shortness of breath, and a systolic murmur is heard. More often, these symptoms are manifestations of infectious-allergic myocarditis; they gradually undergo a reverse development.
Pain in the heart area is a common occurrence in people suffering from alcoholism. In this case, a diagnosis of coronary artery disease is often made, and pain is regarded as angina pectoris. Difficulties in diagnosis are associated with the fact that patients hide alcohol abuse. The ECG often reveals nonspecific changes in the ST segment and T wave. A bicycle ergometer test may be positive. X-rays reveal an expansion of the borders of the heart. An echocardiogram reveals dilatation of the left ventricle. Dynamic observation of patients shows worsening myocardial damage and the appearance of severe arrhythmias provoked by large amounts of alcohol. Diagnosis of alcoholic cardiopathy is facilitated by simultaneous signs of liver damage. Many cardiovascular disorders in these patients are associated with autonomic disorders, which manifest themselves very early, even before the development of severe myocardial damage. Coronary angiography, as a rule, does not reveal stenotic lesions of the coronary arteries.
is often mistaken for ischemic heart disease in patients with neurocirculatory dystonia (we used one of many designations for the disease). Cardiac syndrome with neurocirculatory dystonia is long-lasting and persistent. The pain is mostly stabbing or aching, localized mainly in the apex of the heart or in the second to fourth intercostal space to the left of the sternum. The pain is relieved or reduced by taking valocordin, validol, sedatives, and using mustard plasters.
Vegetative-dystonic syndrome in neurocirculatory dystonia is manifested by lability of pulse and blood pressure, peripheral vascular disorders, and vegetative-vascular paroxysms of predominantly sympathetic-adrenal origin. Asthenic syndrome is characterized by both physical and intellectual exhaustion and a significant decrease in performance. Weakness (of a neurogenic nature) manifests itself primarily in the morning. During the day, the feeling of weakness and fatigue may increase, forcing patients to go to bed. Neurocirculatory dystonia is characterized by a syndrome of neurotic respiratory disorders: a feeling of lack of air, dissatisfaction with inhalation and yawning, the need to periodically take deep breaths. Sometimes the feeling of suffocation or a lump in the throat comes first. Periods of “paroxysmal shortness of breath of a neurotic” are less common. Eggs with neurocirculatory dystonia never feel completely healthy; they always exhibit some syndrome or a combination of several. The onset or exacerbation of the disease is usually associated with a stressful situation (mental and physical stress), less often with infectious exposure or hormonal changes (pregnancy, abortion, dysvariant disorders, menopause).
The long-term existence of cardiovascular disorders without clear organic heart pathology favors the diagnosis of neurocirculatory dystonia. ECG changes concern only the final part of the ventricular complex. With normal heart sizes and normal position of the electrical axis, biphasic or negative T waves are recorded, especially in the chest leads. To more accurately interpret ECG abnormalities, a number of functional and pharmacological tests have been proposed. Hyperventilation and orthostatic tests lead to the appearance or deepening of isoelectric or negative T waves in the chest leads. After stopping the test, the ECG approaches the initial level. Tests with propranolol and potassium chloride, with positive results, are characterized by the transition of a negative or biphasic T wave to a positive one. Positive test results are more often observed in neurocirculatory dystonia, indicating that changes in the final part of the ventricular complex are associated with functional disorders. However, the differential diagnostic value of these tests should not be overestimated. A positive test with propranolol rather indicates increased activity of the sympathetic-adrenal system, which also happens with coronary pathology. The bicycle ergometer test is negative in most patients. Patients often refuse to undergo it until diagnostic criteria are reached due to fear or fatigue. In these cases, other stress tests become more valuable. The dipyridamole test in these patients is usually negative. The isoproterenol test is occasionally false-positive in hypersympathicotonia. Transesophageal electrical stimulation of the atria has great diagnostic value.
In patients in this category, it is extremely important to conduct the entire complex of stress tests. If all tests are negative, then the diagnosis of IHD is confidently removed. If some of the samples are positive, then patients need to undergo coronary angiography. Excluding coronary pathology allows you to more clearly formulate the diagnosis and choose treatment.
When establishing a diagnosis of neurocirculatory dystonia, it is necessary to take into account possible variants of the course of the disease (from mild to severe). The lung is characterized by relative monosymptomatics, spontaneous disappearance of symptoms, and preservation of tube ability are possible. The ECG is usually slightly changed. Drug therapy is often not needed. Moderately severe disease is long-term, with an abundance of symptoms, decrease or temporary loss of disability; patients require drug therapy. A severe course is characterized by persistence and multiplicity of pathological symptoms without a tendency to disappear, and the ability to work is reduced.
The severity of the clinical manifestations of neurocirculatory dystonia is determined mainly by the severity of tachycardial and asthenic syndromes, as well as the presence of vegetative-vascular paroxysms, the addition of cardiophobia and other severe psycho-emotional disorders. Among the many complaints of a patient with neurocirculatory dystonia, it is necessary to highlight the meager, but quite identifiable symptoms of angina pectoris. It is necessary to take into account the possibility of a combination of ischemic heart disease and neurocirculatory dystrophy, which makes it possible to make both diagnoses simultaneously. Usually in such cases the doctor relies on coronary angiography data.
Determination of the concentration of markers of myocardial damage used for the diagnosis of acute coronary syndrome (ACS) and myocardial infarction (MI).
Synonyms Russian
Blood tests for ACS, markers of ACS.
English synonyms
Biomarkers of Acute Coronary Syndrome, ACS; Creatine kinase MB (CK-MB), Troponin I, Myoglobin, AST, ALT.
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Children under 1 year of age should not eat for 30-40 minutes before the test.
- Children aged 1 to 5 years should not eat for 2-3 hours before the test.
- Do not eat for 12 hours before the test; you can drink clean still water.
- Avoid physical and emotional stress for 30 minutes before the test.
- Do not smoke for 30 minutes before the test.
General information about the study
Acute coronary syndrome (ACS) is a set of clinical signs and symptoms that suggest that a patient may have unstable angina or acute myocardial infarction (MI). For the differential diagnosis of ACS and other diseases that may occur with a similar clinical picture (for example, pulmonary embolism), and for the differential diagnosis of clinical forms of ACS (unstable angina, MI with or without ST-segment elevation), a number of additional studies are performed. Laboratory tests are an integral part of the diagnostic examination of a patient with ACS and suspected MI.
Diagnostic testing for ACS includes measuring blood concentrations of creatine kinase MB, troponin I and myoglobin, as well as aspartate aminotransferase (AST) and alanine aminotransferase (ALT).
Troponin I
Troponins (C, T and I) are a group of proteins of the contractile complex of the myocardium and striated muscles. Due to the fact that there are isoforms of troponins T and I characteristic exclusively for the myocardium (cardiac troponins T and I), they are used as markers of myocardial damage.
Troponins are the most accurate and currently preferred markers of myocardial damage. Troponin I and troponin T have approximately the same sensitivity and specificity for myocardial injury. These markers are often used together, but can also be used separately.
Cardiac troponin concentrations in the presence of myocardial infarction increase 4 to 10 hours after the onset of symptoms and remain elevated for two weeks after the onset of symptoms, so these markers can be used to diagnose recent myocardial infarction.
The sensitivity of cardiac troponins for MI when examined in the first 4 hours from the onset of symptoms is about 35%, after 10 hours - 95%. Therefore, troponin I is measured several times - upon admission, after 6 and 12 hours. The specificity of cardiac troponins for MI reaches 96%.
It is important to note that the specificity of laboratory markers for myocardial injury and myocardial infarction are not the same thing. Thus, cardiac troponins have 100% specificity for myocardial injury, but not myocardial infarction. An increase in troponin levels can also be observed in other heart diseases, for example, with cardiac injury, chronic heart failure, myocarditis, pericarditis, left ventricular hypertrophy, or with other diseases and conditions accompanied by myocardial damage, for example, sepsis, respiratory failure, pulmonary embolism, chemotherapy for malignancy or chronic renal failure.
It should be especially emphasized that the concentration of cardiac troponins can remain normal during the first 4-6 hours even after a heart attack has occurred.
Cardiac troponins are not only diagnostic, but also prognostic markers. An increase in their concentration is associated with an increased risk of death from MI and its complications. It has been shown that the degree of risk is directly dependent on the degree of increase in troponin concentrations.
Creatine kinase MV
Creatine kinase MB (CK-MB) is one of the isoforms of the creatine kinase enzyme involved in cellular energy metabolism. The enzyme creatine kinase consists of two subunits M (from the English muscle) and B (from the English brain). Combinations of these subunits form the creatine kinase isoforms CK-BB, CK-MM, and CK-MB. The CK-MM and CK-BB isoforms predominate in muscle and nervous tissue, and creatine kinase MB is found almost exclusively in cardiac muscle. Therefore, an increase in creatine kinase MB concentration serves as a specific indicator of myocardial damage.
In the blood of a person experiencing acute myocardial infarction, an increase in the concentration of creatine kinase MB can be detected within the first 4-8 hours after the onset of symptoms of the disease. The peak increase in concentration occurs at 24-48 hours, and normalization of the indicator usually ends by 3 days. Rapid normalization of this indicator allows the use of creatine kinase MB not only for the diagnosis of primary myocardial infarction, but also for the diagnosis of recurrent infarction. It is believed that the peak concentration of creatine kinase MB does not reflect the extent of myocardial damage.
The sensitivity of creatine kinase MB for MI in a single study is about 35%, and with repeated studies it reaches 95%. For this reason, creatine kinase MB concentration studies are typically repeated 6 and 12 hours after presentation to the emergency room. The specificity of the test reaches 80%. It should be especially emphasized that the concentration of creatine kinase MB may remain normal during the first 4-8 hours even in the presence of an infarction.
If a patient has an increase in troponin I levels with a normal value of creatine kinase MB, they speak of a microinfarction or prolonged minor myocardial damage. Elevations of both creatine kinase MB and troponin I indicate the presence of acute MI.
As in the case of cardiac troponins, an increase in creatine kinase MB can be observed not only in MI, but also in other diseases of the heart and some other organs.
Myoglobin
Myoglobin is a low molecular weight protein present in the myocardium and striated muscle. An increase in myoglobin concentration can be detected in the first 2 hours after the occurrence of myocardial necrosis. Thus, myoglobin is the earliest clinical and laboratory marker of MI. This marker is not specific for myocardial damage, but is very sensitive. The high sensitivity of this marker means that the diagnosis of MI can be practically excluded if the myoglobin concentration measured in the first 4-8 hours from the onset of symptoms of the disease is within normal limits. It should be noted that myoglobin concentration decreases rapidly.
AST and ALT
AST and ALT are enzymes that catalyze the transfer of amino groups between amino acids (transaminases). They are found in many tissues and organs and are therefore not cardiac muscle-specific markers. Myocardial damage is accompanied by an increase in the concentration of AST and ALT in the blood, which can be detected 6-12 hours after the onset of myocardial necrosis, reaches a peak after 24-48 hours and normalizes by the 7th day of the disease.
Changes in AST and ALT concentrations can be observed in many other diseases, including liver disease, hemolysis, renal, splenic and intestinal ischemia, as well as with the use of salicylates, opioids and warfarin.
Currently, AST and ALT are considered as additional markers of myocardial damage. In terms of their information content, they are significantly inferior to cardiac troponins and creatine kinase MB.
When confirming the diagnosis of “MI” or another clinical form of coronary heart disease (CHD), it is advisable to conduct additional laboratory examinations to identify and correct risk factors for CHD, primarily hypercholesterolemia (lipid profile) and diabetes mellitus (fasting glucose or glycated hemoglobin).
What is the research used for?
- For the diagnosis of acute coronary syndrome (ACS) and myocardial infarction (MI).
When is the study scheduled?
- In the presence of typical symptoms of ACS: sudden intense pain in the heart area, associated with physical activity or occurring at rest, radiating to the left arm, neck, lower jaw, lasting more than 15 minutes and accompanied by dizziness, weakness, shortness of breath, palpitations and anxiety;
- when identifying ECG signs of myocardial infarction.
What do the results mean?
Reference values
For each indicator included in the complex:
- [06-003] Alanine aminotransferase (ALT)
- [06-010] Aspartate aminotransferase (AST)
- [06-023] Creatine kinase MB
- [06-076] Troponin I
- [06-079] Myoglobin
What can influence the result?
- Time elapsed since the onset of the first symptoms of the disease;
- volume of myocardial damage;
- presence of concomitant heart diseases;
- the presence of diseases of skeletal muscles, kidneys, liver and some other organs;
- taking cardiotoxic drugs (doxorubicin, mitoxantrone).