Risk factors and prevention of cardiovascular diseases
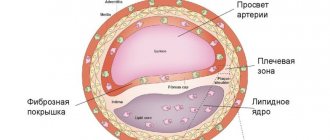
Despite the variety of serious diseases relevant to the modern world, cardiovascular diseases are still the leading cause of death in the world. Heart disease accompanies any type of illness that affects the cardiovascular system. These are mainly heart diseases, vascular diseases of the brain and kidneys, as well as diseases of peripheral arteries. The causes of heart disease are varied, but the most common are atherosclerosis and hypertension. In addition, with age, a number of physiological and morphological changes occur that impair the function of the heart and blood vessels, and subsequently lead to an increased risk of heart disease, even in healthy people without symptoms.
Risk factors for developing cardiovascular diseases
Risk factors can be removable and non-removable. Avoidable are risk factors that can be eliminated in one way or another, and NOT avoidable are risk factors that (unfortunately) cannot be eliminated.
Below I will list the risk factors, and you count - how many of them do you have? The more risk factors you have, the more likely you are to develop cardiovascular disease, and if you have diseases, to develop complications.
Unavoidable risk factors:
- Gender and age: the risk is higher in men than in women; with age, the differences decrease (at the age of 35–70 years, men have a 30% higher risk of death from stroke, and 2–3 times higher risk of death from ischemic heart disease than women. At the age of 75 years, the risk of death from CVD is approximately the same in men and women Men over 55 years of age and women over 65 years of age are more susceptible to cardiovascular diseases.
- Menopause. Menopausal women have a higher risk of cardiovascular disease.
- Heredity. Heart disease in your direct relatives indicates a higher likelihood of developing similar diseases in you.
- Geographic region of residence: high incidence of stroke and ischemic heart disease in Russia, Eastern Europe, and the Baltic countries.
- Damage to target organs (heart, brain, kidneys, retina, peripheral vessels). The presence of irreversible diseases of the listed organs significantly increases the risk of cardiovascular disaster.
- Diabetes. Diabetes mellitus is currently classified as a target organ disease. Signs of diabetes: thirst, dry mouth, high fluid intake, frequent (painless) and copious urination.
Avoidable risk factors:
- Smoking was named first because it is the easiest to eliminate: smoking increases the risk of heart disease by 1.5 times; increases the risk of atherosclerosis, obliterating vascular diseases, and cancer; increases LDL cholesterol (the worst for the heart); increases blood pressure both in patients with hypertension and in people with normal blood pressure.
- Hypercholesterolemia (total cholesterol > 5.2 mol/l).
- Dyslipidemia (changes in the ratio of levels of different cholesterol fractions):
- Increased systolic (upper) blood pressure > 140 mmHg.
- Increased diastolic (lower, “heart”) blood pressure > 90 mm Hg.
- Increased salt intake.
- Obesity: with a body mass index of 25 - 29 (obesity 2 degrees) the risk of coronary heart disease is 70% higher, with a BMI > 30 (obesity 3 degrees) - 300% higher; At the same body weight, the risk of coronary artery disease, stroke and death increases with increasing waist/hip ratio.
- Alcohol abuse.
- Physical inactivity (daily exercise of light or moderate intensity for 20 minutes reduces the risk of death from coronary artery disease by 30%).
- Stress.
- Increased blood sugar.
- In case of impaired renal function, when protein begins to leak through the kidneys, as well as hypercreatininemia (chronic renal failure) - a later criterion for kidney damage, when the kidneys cannot cope with their function.
- Pulse blood pressure (the difference between systolic and diastolic) is more than 60 mmHg, high blood pressure variability (range of values within 24 hours), insufficient decrease or increase in blood pressure at night. That is, there should be no sudden surges in pressure, and at night the blood pressure should be lower than during the day.
- Tachycardia, i.e. rapid pulse or heartbeat.
- Sleep apnea syndrome. This includes snoring and short-term pauses in breathing during sleep.
- Socioeconomic status (the lower the social status, the higher the risk of cardiovascular disease).
- Stress.
PREVENTION
- Quit smoking and protect yourself from secondhand smoke.
Firstly, smoking is one of the main causes of atherosclerosis, arterial hypertension, coronary heart disease and stroke. And, on the contrary, stopping smoking leads to a reduction in the risk of the disease by exactly half. Secondly, cigarette smoke contains not only nicotine, but also carcinogenic tars that affect the human cardiovascular system. The characteristic fact is that passive smoking is just as destructive as active smoking.
- Don't abuse alcohol.
Alcohol in minimal quantities (no more than 20 ml of ethanol for women and no more than 30 ml of ethanol for men per day) thins the blood and has a beneficial effect on the cardiovascular system, but if the norm is exceeded, its effect becomes sharply negative.
- Control your weight.
People who are overweight and especially obese are 2–3 times more likely to develop cardiovascular diseases, and they are more likely to develop complications. Control your weight and waist circumference.
- Eat right.
Moderate consumption of meat (especially red), a sufficient amount of fish (minimum 300 g per week), consumption of vegetables and fruits, refusal or limitation of fatty, fried, smoked foods - these are simple and effective measures that will not only allow you to keep your body in good shape, but will also significantly reduce the risk of cardiovascular diseases. Monitor your blood cholesterol levels and remember that they can be normalized with proper healthy eating.
- Move more.
The normal and necessary level of physical activity is 150 minutes of any physical activity per week - this is a prerequisite for successful prevention of cardiovascular diseases.
- Learn to control stress.
Chronic lack of sleep, as well as constant psychological stress, weaken the immune system, exhaust a person, and cause arrhythmia and disturbances in cardiac activity in general. Healthy sleep and a philosophical attitude to life, on the contrary, significantly increase your chances of avoiding cardiovascular diseases.
- Diabetes control.
If you have diabetes, strictly follow all the recommendations of your doctor, monitor your blood sugar levels and be aware of any changes in your health.
- Monitoring blood pressure levels.
Monitor your blood pressure and, if you have any disorders (hypertension, hypotension), be sure to follow all the recommendations of your doctor.
ADVICE OF A CARDIOLOGIST:
ALGORITHM OF ACTIONS FOR HEART PAIN.
1. Pain in the heart area is one of the most common reasons why people seek emergency medical care. These pains attract attention and cause concern more than many others.
2. It is known that half of the adverse outcomes in various forms of acute coronary syndrome (ACS is a concept that unites a number of severe and life-threatening conditions at any moment) occur in the first hours of the disease, so time in this case is a dangerous enemy, and the greatest efforts must be made be targeted for early diagnosis and treatment.
3. The positive effect in the treatment of ACS directly depends on the time of seeking medical help. In this case, the signs of a heart attack may be reversible and will not significantly affect the functional state of the heart in the future.
4. The onset of myocardial infarction often has a typical character - the pain seems to burn, press and squeeze, occurs in the area behind the sternum and can radiate to the left arm. Often pain is accompanied by severe anxiety and fear: a person tries to find a place for himself, cannot fully understand what is happening. In the case of initial forms of the disease, pain subsides within one to five minutes after taking the drug. If the pain does not disappear after this period of time, it means that this is a signal that the disease has become more severe, and, therefore, there is a high chance of developing a myocardial infarction.
5. During an attack, the following measures are recommended for urgent pain relief:
- create physical and psycho-emotional peace for the patient: lie down, sit down, or stop if chest pain appears during exercise;
- It is urgent to take 1 tablet of nitroglycerin under the tongue.
- The analgesic effect of nitroglycerin usually occurs within 1–5 minutes. To stop an attack, 1-2 tablets of nitroglycerin are enough;
- you need to take ½ tablet of acetylsalicylic acid;
- if the attack is prolonged (lasts 10–15 minutes) and repeated doses of nitroglycerin are ineffective, you must immediately call an ambulance - this cannot be tolerated!
6. If the pain lasts more than 10–15 minutes, it cannot be tolerated. It is urgent to call an ambulance. The outcome of treatment depends on how early the patient consulted a doctor. Nowadays, many patients tend to delay this. Some believe that the pain is associated with osteochondrosis, others - with bronchitis, smoking, etc. Such underestimation of the symptoms of the disease often causes late treatment, and therefore a late start of treatment.
ATTENTION! A patient with a heart attack is strictly forbidden to get up, walk, smoke or eat until the doctor’s special permission; Do not take Aspirin (Acetylsalicylic acid) if you are intolerant to it (allergic reactions), as well as with a clear and severe exacerbation of gastric and duodenal ulcers; Nitroglycerin should not be taken if there is severe weakness, sweating, as well as severe headache, dizziness, acute impairment of vision, speech or coordination.
ACUTE CEREBRAL CIRCULATION IMPAIRMENT (ACI).
Main signs (symptoms):
- Numbness, weakness, “disobedience” or paralysis (immobility) of an arm, leg, half of the body, distortion of the face and drooling on one side;
- Speech disorders (difficulty in choosing the right words, understanding speech and reading, slurred and unclear speech, up to complete loss of speech);
- Impaired or loss of vision, double vision, difficulty focusing;
- Impaired balance and coordination of movements (feelings of “swaying, sinking, body rotation, dizziness”, unsteady gait up to falling);
- Unusually severe headache (often after stress or physical exertion);
- Confusion or loss of consciousness, uncontrollable urination or bowel movements.
If any of these signs suddenly appear, call an ambulance immediately, even if these manifestations of the disease were observed for only a few minutes.
Algorithm of actions before the arrival of an emergency medical team.
If stroke occurs, it is necessary to follow the instructions received earlier from the attending physician; if there were no such instructions, proceed according to the following algorithm:
- If the patient is unconscious, place him on his side, remove removable dentures (food debris, vomit) from the mouth, make sure that the patient is breathing.
- If the victim is conscious, help him take a comfortable sitting or semi-sitting position in a chair or on a bed, placing pillows under his back. Provide fresh air. Unbutton your shirt collar, belt or waistband, and remove tight clothing.
- Take 2 Glycine tablets and place them under the patient’s tongue.
- Measure the patient's body temperature. If it is 38 degrees Celsius or more, give the patient 1g of Paracetamol (2 tablets of 0.5 g, chew, swallow), (if Paracetamol is not available, do not give other antipyretic drugs!).
- Place ice or freezer food in waterproof bags wrapped in a towel on your forehead and head.
- If the patient has previously taken medications that lower blood cholesterol levels from the statin group (Simvastatin, Lovastatin, Fluvastatin, Pravastatin, Atorvastatin), give the patient his usual daily dose and take the drug with you to the hospital.
- If the arrival of emergency medical services is delayed, measure the patient's blood pressure and if its upper level exceeds 220 mm Hg, give the patient a blood pressure lowering drug that he was taking previously.
- If the victim has difficulty swallowing and saliva drips from his mouth, tilt his head towards the weaker side of the body and blot the dripping saliva with clean napkins.
- If the victim is unable to speak or has slurred speech, reassure and reassure him that the condition is temporary. Hold his hand on the non-paralyzed side, stop him from trying to talk, and don't ask questions that require an answer.
- Remember that although the victim cannot speak, he is aware of what is happening and hears everything that is said around him. Next, before the arrival of the emergency medical team, the patient must place 1-2 Glycine tablets under the tongue at intervals of 5-10 minutes (in total, no more than 10 tablets).
REMEMBER!
- closed cardiac massage performed in the first 60–120 seconds after sudden cardiac arrest allows up to 50% of patients to be brought back to life;
- Only emergency medical care called for the first time 10 minutes from the onset of a heart attack or stroke allows the full use of modern highly effective methods of hospital treatment and many times reduce mortality from these diseases;
- Acetylsalicylic acid (Aspirin) and Nitroglycerin taken for the first time for 5 minutes can prevent the development of myocardial infarction and significantly reduce mortality from it;
- state of alcoholic intoxication is not a reason for delaying calling an ambulance in the event of a heart attack and stroke - about 30% of people who died suddenly at home were intoxicated.
All articles
Print Email
Poor nutrition
Several decades of scientific research have convincingly demonstrated that certain eating habits characteristic of modern life, formed from early childhood, are the cause of the epidemic spread of obesity and diseases associated with atherosclerosis. This includes a diet “rich” in fats and calories, which can influence an increase in blood pressure, serum cholesterol, and is also, according to some data, associated with a higher prevalence of type 2 diabetes.
In many countries, most populations have developed eating habits that were not previously widespread. These habits include excessive consumption of: a) fat and cholesterol; b) refined and processed carbohydrates and other low-fiber foods; c) foods high in calories relative to essential nutrients; d) calories exceeding energy costs; e) table salt and other sodium-rich substances.
It was found that dietary cholesterol has an effect on the increased incidence of coronary heart disease. Therefore, directly or indirectly, dietary cholesterol may increase the risk of developing a number of diseases, and most experts recommend that the average intake should be no more than 300 mg per day.
Population-based studies have demonstrated that CHD mortality and blood lipid levels are lower in populations whose diets are rich in complex carbohydrates and low in fat. Diet is the main factor in everyday life that influences the development of arterial hypertension. Sodium (contained in table salt), excess energy, and alcohol are the main dietary factors that are related to the development of arterial hypertension and a number of other diseases. And populations with low daily consumption of table salt and low incidence of hypertension are simultaneously characterized by high potassium consumption.
Dietary recommendations:
- The diet should include 4 meals a day, with the following distribution of daily calorie content: breakfast 30%, lunch - 40%, afternoon snack - 5-19%, dinner - 25%.
- Limiting easily digestible carbohydrates (baked goods, confectionery, sugary drinks)
- Increasing the amount of fiber consumed (gray cereals, fruits and vegetables > 400g/day)
- Limiting salt intake
- The main direction of obesity prevention is the desire not to overeat
The most effective family transition to healthy eating!
Physical inactivity
Physical inactivity (decreased physical activity) causes a progressive decrease in the adaptive capabilities of the cardiovascular system, promotes weight gain, and reduces the human body’s adaptation to stress. It has been established that individuals with a higher level of physical activity at the same height have lower body weight than individuals with a low level of physical activity. Thus, increasing physical activity may be one of the “tools” for the prevention of CVD.
It is extremely important to control your physical activity, which should be at least 150 minutes per week. This means both visiting gyms in free time from work or study, as well as everyday physical activity (housework or gardening, going to work or school, etc.).
Recommendations for daily physical activity:
- use the stairs instead of the elevator;
- walk from the next nearest public transport stop;
- walks during lunch break;
- use a toilet on another floor;
- when leaving home, if possible, use a bicycle or walk instead of public transport or a car;
- do cleaning and work around the house and garden (vacuuming, wiping windows, mowing, weeding);
- leave sports walking shoes in a visible place in the hallway;
- wash your car at a self-service car wash or by hand;
- try to walk with wider steps and faster than usual.
Following these simple tips will help maintain your health.