Intraocular pressure (in other words, ophthalmotonus) is the fluid pressure inside the eyeball. Its measurement is one of the main diagnostic studies carried out by an ophthalmologist to assess the condition of the visual apparatus.
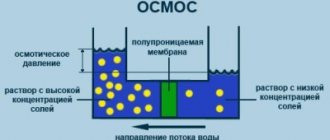
Everyone has normal eye pressure: it is necessary to maintain the shape of the eyeball and keep it in good shape. In the cavity of the eyeball, which is a closed system, aqueous humor is continuously produced. There are ways for its outflow, called the drainage system: excess fluid is evacuated into the venous vessels.
Iphthalmotonus is the result of the relationship between the volume of secreted moisture and the rate of its removal through the drainage system - mainly through the trabecular meshwork, which is located in the corner of the anterior chamber of the eye. The most common deviation of ophthalmotonus from the norm is called high intraocular pressure: it leads to glaucoma and severe disabling consequences. Low pressure is also not normal: in this case, the eyeball does not hold its shape, and the functioning of the vitreous body is disrupted.
What is ophthalmotonus?
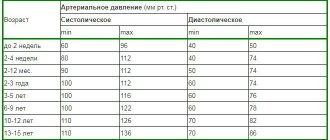
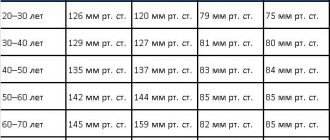
Intraocular pressure is normal when approximately 2 mm³ of fluid enters and flows out of the eye every minute. It is with this ratio that it has an indicator of 12 to 22 mmHg. The value may depend on age, physical activity, even the pressure is different in the morning and evening. However, so far it does not exceed 22 mm Hg. and does not fall below 12 mmHg, then it is considered normal. If the process of inflow and outflow is unstable, then the pressure is not normal. There are three types of such violations.
- Transient - there is a short-term deviation from the usual indicator and a return to the limits.
- Labile - pressure increases occur on a regular basis.
- Stably elevated blood pressure is constantly observed, and this poses a great danger to the health of the visual organs.
However, IOP varies depending on age. Until the age of 40, it is 12-22 mm Hg; at 50-60 years, a value of 23-25 mm Hg is considered normal, and after 70 years, this figure increases to 23-26 mm Hg. These values do not indicate a pathological condition.
Folk remedies
Alternative medicine can be used to supplement the treatment prescribed by your doctor. There are simple but effective recipes that have stood the test of time.
Aloe decoction
Used to wash eyes. Aloe (about 5 leaves) is poured with boiling water (250-300 ml). Boil the product for 5 minutes. After cooling, the decoction is ready for use.
Decoction of nettle and lily of the valley
Used for lotions. Nettle and lily of the valley (2 tsp each) are poured with boiling water (200 ml). Cover the container with a lid and let the product brew for 9-10 hours. Cotton pads soaked in liquid are applied to closed eyes (for 5-7 minutes).
Potato compresses
The raw root vegetable is grated on a fine grater. Combine it with apple cider vinegar (5 ml). Let it brew for half an hour. The pulp is applied to gauze napkins and placed on closed eyes. You need to keep the compress for 10 minutes.
Regardless of which prescription is chosen to stabilize eye pressure, the course duration is at least 1 month. Regularity of procedures – 2-3 rubles. in Week.
Causes and symptoms of high blood pressure
Increased IOP is much more common than hypotonicity. Its increase may be due to various factors:
- increased production of intraocular fluid;
- significant physical activity;
- frequent consumption of coffee or alcohol;
- severe stress, etc.
An additional risk factor is also the presence of chronic diseases that affect the condition of the eyes: diabetes mellitus, cardiovascular pathologies, hereditary factors. If you have relatives suffering from glaucoma, then you should definitely visit an ophthalmologist for a vision test. With minor deviations from the IOP norm, a person does not even notice discomfort - there are no symptoms of the disorder. They appear only during labile surges or with constantly elevated IOP, when the values already reach 40-50 mmHg. With an average intraocular pressure of 22 to 40 mm Hg. nothing hurts, my eyes don’t turn red, and it doesn’t affect my vision. It is not for nothing that glaucoma, which is inevitable with a persistently increased IOP, is called the “silent thief of vision.”
In old age, you also need to carefully monitor the state of ophthalmotonus. According to medical statistics, 20% of people over 65 years of age are diagnosed with glaucoma, after 70 years of age this figure is 30%, and among people over 80 years of age - 40%. This is explained simply: over time, the outflow of fluid from the eye worsens.
Exercise for the eyes
Purpose of the exerciseExecution techniqueTime costsRelaxing muscles, relieving tension. Close your eyes with your palm. After relaxing, blink a couple of times. Repeat blinking at 5 second intervals. 2 minutes. Increasing the flexibility of the eye muscles. Draw an infinity sign with your eyes, imagining it mentally. Movements are performed exclusively by the pupils. 2 min. Strengthening muscles, improving vision. Select 2 objects in the room: close (30 cm) and distant. Focus your gaze on one and the other object alternately. For 1-1.5 minutes. on every subject. Change the position of the eyes 10-15 times. Improving focus Focus your gaze on your arm extended forward. Bring the phalanges closer to the nose, not reaching 8 cm. Move your hand back. For 2-3 minutes. keep your finger on your finger.Eye exercises improve visual function, normalize the outflow of tear fluid, and reduce stress on the optic nerve.
Symptoms of increased intraocular pressure
Here are some manifestations and signs that may indicate that ophthalmotonus is increased:
- headaches in the temples, dizziness;
- painful sensations in the eyes with sudden movements of the head, raising the eyebrows;
- decreased peripheral vision;
- blurred vision after waking up;
- redness of the eyes due to a pronounced capillary network.
All of these signs can directly indicate the presence of increased intraocular pressure. If they persist, you should visit an ophthalmologist for a comprehensive examination of your vision organs. The most dangerous consequence of increased IOP is glaucoma, which is also called the eye “plague”.
Glaucoma is an ophthalmological disease in which intraocular pressure is constantly elevated or there are sudden changes. If it is not reduced to normal in time, the optic nerve dies, and this inevitably leads to blindness.
According to statistics, approximately 14-15% of blind people in the world have lost their vision due to glaucoma. The overwhelming majority of people with this pathology are over 50 years old. However, it can also occur in infants (congenital) and young adults (juvenile form). The pressure increases due to poor outflow of fluid from the angle of the anterior segment of the eye, which causes its excess to form. As a result, the eyeball begins to put pressure on the optic nerve, causing its damage and, as a result, vision impairment. Then peripheral vision begins to decrease, the visibility area is limited. If the optic nerve dies, the person goes blind. These changes are irreversible. Loss of vision can also occur suddenly as a result of an acute attack.
People at risk (we listed them above) should be especially attentive to the state of their vision. If there are signs of deterioration, you should definitely visit an ophthalmologist for a full diagnosis. Glaucoma cannot be completely cured, but medications can slow the progression of the disease by maintaining stable IOP. In some cases, operations are prescribed to normalize intraocular pressure. They are aimed at increasing the outflow of aqueous humor or reducing its production.
Measurement methods
Patients cannot measure intraocular pressure on their own. This requires medical devices. Common values in numbers are a natural indicator of IOP or the result obtained using the Maklakov technique.
The process of obtaining data involves applying a certain force to the eye. Decoding the response of the organ of vision reflects the result. Measurement impact options:
- Contact - the ocular surface is in contact with the measuring device.
- Non-contact - air flow is used as a force to influence the organ of vision.
When conducting an examination in a clinic, the following tonometry methods are offered:
- electronograph;
- ICare tonometer;
- Goldmann device;
- according to Maklakov;
- non-contact tonometry;
- pneumotonometer;
- device "Pascal".
Pneumotonometry is a painless procedure. The patient does not feel any discomfort during IOP measurement. Taking accurate data is necessary for high-quality diagnosis and adequate prescriptions. Therefore, readings made by an ophthalmologist by pressing a finger on the eyeball are not taken into account. This information can only be used to make a preliminary diagnosis.
Ultra-precise IOP measurements are necessary to diagnose and treat glaucoma. Inaccuracies can have serious consequences.
The pressure inside the eye can be determined by performing daily tonometry. The analysis is carried out in two ways: according to Goldman, according to Maklakov. The devices take accurate measurements without causing any discomfort to the patient.
According to Goldman
The procedure is carried out in this order:
- An anesthetic and contrast liquid are injected into the eye cavity.
- The patient is asked to sit down at the slit lamp, on which the tonometer is fixed.
- The ophthalmologist applies a prism to the eye and applies moderate pressure with the object on the cornea.
- Using a blue filter, a specialist takes readings at the right moment, and then deciphers them using a special scale.
According to Maklakov
The procedure is carried out in a lying position in the following order:
- Injection of an anesthetic solution into the eye cavity.
- Contrast liquid is applied to glass plates.
- Lower the device onto the cornea so that the painted surface comes into contact with it.
- Press on the eyeball with a metal object.
- The resulting prints are placed on damp paper and measurements are taken with a ruler.
Similar actions are performed with the second eye. You can get the most accurate results by taking measurements 2 p. in a day. This approach is due to the fact that throughout the day the ophthalmotonus changes within three units.
What is low ophthalmotonus
In addition to increased IOP, low blood pressure also occurs, although much less frequently. This condition may be caused by the following reasons:
- retinal detachment;
- inflammatory processes in the eyes;
- eye injuries;
- low blood pressure;
- dehydration and some others.
With reduced ophthalmotonus, the following symptoms are observed: dry eyes, painful sensations when blinking, pop-up dots, burning, blurred vision. Low IOP is no less dangerous than high IOP. Clinical examination of this condition reveals papilledema, venous congestion, maculopathy, papillar atrophy, vitreous opacities, and keratopathy. Visual functions deteriorate significantly.
Prevention measures
It is always easier to prevent diseases, so experts recommend adhering to the following rules in everyday life.
- Time for work and rest should be balanced. The body (including the visual system) needs at least 8 hours a day to rest.
- You need to take breaks throughout the day. At this time, you can allocate 3-5 minutes to perform eye exercises or massage.
- Before going to bed, it is recommended to massage the eyeballs with your fingertips, making circular movements clockwise and counterclockwise.
- Observe personal hygiene rules.
- Stick to a balanced diet. Include more fresh fruits, berries and vegetables, and foods containing Omega-3 acids in the menu.
- Use vitamin complexes, which include microelements beneficial for eye health.
- When performing exercises, you should not put too much pressure on your eyeballs. Heavy physical exercises involving heavy lifting and other overexertion are also not recommended. This automatically increases the IOP.
- Spend more time outdoors on weekends. Active games and hikes are the best cure for all diseases.
Periodically you need to visit an ophthalmologist for a preventive examination. This will help identify the problem at an early stage, which will simplify treatment.
How can you measure intraocular pressure?
To measure IOP, contact and non-contact tonometers of various modifications are used, including pneumotonometers. The ophthalmologist decides which method to use for diagnosis, depending on the patient’s age, existing pathology, etc.
At the Center for Contact Vision Correction on Tverskaya, intraocular pressure can be checked using various methods. You can make an appointment by calling +7, +7 (800) 100 95 96. Our specialists will carry out other diagnostic procedures if necessary. We are glad to see residents of Moscow and the Moscow region, as well as guests of the capital, in our Center. The Central Clinical Hospital on Tverskaya is open every day, without days off or breaks, from 9.00 to 21.00 (doctors are seen until 20.00 ).
Nutrition
Some adjustments are made to the diet. The amount of foods that contribute to the rise of insulin is reduced. This applies to potatoes, pasta, sugar, bakery products, and cereals. It is recommended to consume more dark-colored berries (blackberries, blueberries), as well as vegetables that contain lutein (spinach, Brussels sprouts, broccoli).
Omega-3 fatty acids should be included in the menu. They can be consumed in the form of dietary supplements or natural products - seafood (salmon, tuna, salmon, herring).
Types of tonometers
More than a hundred years have passed since the appearance of the first device for measuring IOP. A large number of hardware modifications have been developed. Only a few of them were in demand.
- The non-contact device measures the effect of a pulse of air on the smoothing of the cornea. A stream of compressed air, dosed in strength and volume, is supplied to the center of the cornea. The equipment records the deformation of the cornea. The non-contact pneumotonometer does not require the use of anesthetics or colored substances. The possibility of injury to the cornea and infection is excluded. Delivery of results is automated. The procedure is easily tolerated by children and is not contraindicated in patients with a number of limitations. The method is simple, but less accurate compared to contact analogues.
- Applanation:
- Maklakov's tonometer is a hollow cylinder with a lead ball inside. The base is made of glass plates onto which special paint is applied. The plate is pressed against the cornea, it becomes colored, and the color disappears on the glass. The area of the spot depends on the size of the contact; the larger it is, the lower the tone and IOP. The same operation is repeated with the second plate. The diameter of the circle imprint on paper is measured using a special ruler with printed IOP values, which are inversely proportional to the size of the display.
- The Goldmann tonometer is placed at the slit lamp. Sodium fluorescein is instilled into the eye. The illuminated prism is placed on a natural lens, adjusting the pressure so that the colored green half rings come together. The result is read on a scale.
- Impressional:
- The most successful Schiotz tonometer. It is a concave plate at the base with a rod attached to it, connected to an arrow on the scale. A piston with a weight moving along it is placed on the cornea. Under the influence of IOP, the piston moves and deflects the needle on the device. Lowering the plunger by 0.05 mm moves the pointer by 1 mm. The IOP value is calculated using tables taking into account the weight of the weight. The tonometer is easy to use, but is inferior in accuracy to applanation devices.
- Dynamic contour:
- The Pascal tonometer is mounted on the slit lamp. The tip resembles the contours of the cornea, which does not flatten under its influence. A miniature sensor is located in the center. The probe is placed on the tear film and automatically measures the pressure. The device calculates the average of a series of measurements.