Elevated blood sugar, or hyperglycemia, occurs for a variety of reasons. Normally, the sugar level should not be higher than 5.5 mmol/l. The severity of hyperglycemia is determined by two main factors: the total amount of glucose in the blood and the rate at which it increases. In medical practice, the pathological condition in question is classified according to two criteria: fasting hyperglycemia and afternoon hyperglycemia.
Glucose is necessary for the cells of the human body, but if its level exceeds the norm, this can lead to irreversible consequences. The person himself may not notice the symptoms of this condition for a long time if it is mild. If the sugar level is significantly elevated, characteristic signs appear that are important to recognize in time and consult a doctor. In our clinic you can always get advice from competent specialists, take the necessary tests and undergo a course of treatment.
Causes of high blood sugar
High blood sugar may be associated with certain diseases:
- diabetes mellitus and other endocrine pathologies;
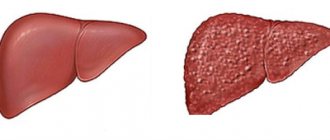
- liver diseases;
- dysfunction of the pancreas;
- severe infectious diseases;
- obesity.
Diabetes mellitus is considered the most common cause of hyperglycemia, which is long-lasting and negatively affects almost all internal organs and systems of the body.
Factors that contribute to hyperglycemia that are not associated with pathologies of the body are also identified:
- overeating, predominance of simple carbohydrates in the diet;
- stress;
- severe premenstrual syndrome in women;
- alcohol abuse;
- hereditary predisposition.
Associated symptoms
A pronounced increase in blood sugar levels manifests itself with characteristic symptoms, which are especially clearly visible in patients with diabetes:
- constant thirst and dry mouth;
- increased urge to urinate;
- dizziness;
- headache;
- increased appetite, weight gain or sudden weight loss (this symptom is typical mainly for patients with type 1 diabetes);
- skin itching, furunculosis, prolonged wound healing;
- increased blood pressure due to impaired renal function;
- increased irritability;
- drowsiness;
- apathetic state;
- difficulty concentrating;
- decreased vision;
- susceptibility to infectious diseases.
Having noticed such manifestations in yourself, you may suspect hyperglycemia, but only a qualified doctor will make an accurate diagnosis. In our clinic you can undergo a full range of examinations to identify acute and chronic diseases. An experienced endocrinologist will develop effective treatment tactics to eliminate pathological symptoms and return you to good health.
Links[edit]
- ^ abcdefghij American Diabetes Association (2014). "Diagnostics and classification of diabetes mellitus". Diabetes care
.
37
: S81 – S90. DOI: 10.2337/DC14-s081. PMID 24357215. - Pais I, Hallschmid M, Jauch-Chara K et al (2007). "Mood and cognitive performance during acute euglycemia and mild hyperglycemia in patients with type 2 diabetes." Exp. Clin. Endocrinol. Diabetes
.
115
(1):42–46. DOI: 10.1055/s-2007-957348. PMID 17286234. - Sommerfeld AJ, Deary IJ, Frier BM (2004). "Acute hyperglycemia alters mood and reduces cognitive performance in people with type 2 diabetes". Diabetes care
.
27
(10): 2335–40. DOI: 10.2337/diacare.27.10.2335. PMID 15451897. - ^ ab Geijselaers, Stefan LC; Sep, Simone JS; Claessens, Danny; Scar, Miranda T.; Van Boxtel, Martin PJ; Henry, Ronald M.A.; Verhey, France R.J.; Kroon, Abraham A.; Dagnelie, Pieter C.; Schalkwijk, Casper G.; Van der Kallen, Carla J. H.; Bissells, Gert Jan; Stehouwer, Cohen D.A. (2017). "The role of hyperglycemia, insulin resistance and blood pressure in cognitive differences associated with diabetes - the Maastricht study". Diabetes care
.
40
(11): 1537–1547. DOI: 10.2337/dc17-0330. PMID 28842522. - Kraemer, Fredrik B.; Shen, Wen-Jun (2002). "Hormone-sensitive lipase". Journal of Lipid Research
.
43
(10):1585–1594. DOI: 10.1194/jlr.R200009-JLR200. ISSN 0022-2275. PMID 12364542. - "Chronic hyperglycemia may cause heart damage". Journal of the American College of Cardiology
. 2012-02-03. Retrieved February 3, 2012. - Miller, Miller's Anesthesia, 7th edition, pp. 1716, 2674, 2809.
- Jump up
↑ Duncan A. E. (2012).
"Hyperglycemia and perioperative glucose management". Current Pharmaceutical Design
.
18
(38):6195–6203. DOI: 10.2174/138161212803832236. PMC 3641560. PMID 22762467. - Umpierrez, Guillermo E.; Pasquel, Francisco J. (April 2017). "Management of hospital-acquired hyperglycemia and diabetes in older adults". Diabetes care
.
40
(4):509–517. DOI: 10.2337/dc16-0989. ISSN 0149-5992. PMC 5864102. PMID 28325798. - ^ ab Hage, Mirella; Zantout, Mira S.; Azar, Sami T. (07/12/2011). "Thyroid diseases and diabetes mellitus". Journal of Thyroid Research
.
2011
: 439463. doi: 10.4061/2011/439463. ISSN 2042-0072. PMC 3139205. PMID 21785689. - Scaroni, Carla; Zilio, Marialuisa; Foti, Michelangelo; Boscaro, Marco (2017-06-01). "Glucose metabolism abnormalities in Cushing's syndrome: from molecular basis to clinical management". Endocrine Reviews
.
38
(3): 189–219. DOI: 10.1210/er.2016-1105. ISSN 0163-769X. PMID 28368467. S2CID 3985558. - Mubarik, Atik; Aeddula, Narothama R. (2020), "Chromaffin Cell Cancer", StatPearls
, Treasure Island (FL): StatPearls Publishing, PMID 30570981, retrieved 22 November 2021 - Link to Oxford Table. Endocrinology. Turner, Helen E., 1967-, Eastell, R. (Richard), Grossman, Ashley (first edition). Oxford. 2021. ISBN 978-0-19-967283-7. OCLC 1016052167.CS1 maint: others (link)
- Wewer Albrechtsen, Nicolai J.; Kuhre, Rune E.; Pedersen, Jens; Knop, Philip K.; Holst, Jens J. (November 2021). "Glucagon biology and consequences of hyperglucagonemia". Biomarkers in Medicine
.
10
(11): 1141–1151. DOI: 10.2217/ВММ-2016-0090. ISSN 1752-0371. PMID 27611762. - "Hyperglycemia in diabetes". Mayo Clinic. Retrieved September 22, 2021.
- Kim, J.Y.; Bacha, F.; Tfaili, H.; Mikhalishin, SF; Yusuf, S.; Arslanyan, S. (2019). "Adipose tissue insulin resistance in youth ranging from normal weight to obesity and from normal glucose tolerance to impaired glucose tolerance and type 2 diabetes". Diabetes care
.
42
(2):265–272. DOI: 10.2337/dc18-1178. PMC 6341282. PMID 30455334. - Swe MT, Pongchaidecha A, Chatsudthipong V, Chattipakorn N, Lungkaphin A (2019). "Molecular signaling mechanisms of renal gluconeogenesis in non-diabetic and diabetic conditions". Journal of Cellular Physiology
.
234
(6):8134–8151. DOI: 10.1002/jcp.27598. PMID 30370538. S2CID 53097552. - Sargsyan A, German M.A. (2019). "Regulation of glucose production in the pathogenesis of type 2 diabetes". Current Diabetes Reports
.
19
(9):77. DOI:10.1007/s11892-019-1195-5. PMC 6834297. PMID 31377934. - ^ a b Li S, Dong XX (2017). "FoxO integration of insulin signaling with glucose and lipid metabolism". Journal of Endocrinology
.
233
(2): R67–R79. DOI: 10.1530/JOE-17-0002. PMC 5480241. PMID 28213398. - Cetin M, Yetgin S, Kara A et al (1994). "Hyperglycemia, ketoacidosis, and other complications of L-asparaginase in children with acute lymphoblastic leukemia." J Med
.
25
(3–4): 219–29. PMID 7996065. - Luna B, Feinglos M. N. (2001). "Drug-induced hyperglycemia." JAMA
.
286
(16):1945–48. DOI: 10.1001/jama.286.16.1945. PMID 11667913. - Capes SE, Hunt D, Malmberg K, Pathak R, Gerstein HC (2001). "Stress hyperglycemia and stroke prognosis in nondiabetic and diabetic patients: a systematic review". Stroke
.
32
(10):2426–32. DOI: 10.1161/hs1001.096194. PMID 11588337. - ^ ab Umpierrez, Guillermo E.; Pasquel, Francisco J. (2017). "Management of hospital-acquired hyperglycemia and diabetes in older adults". Diabetes care
.
40
(4):509–517. DOI: 10.2337/dc16-0989. PMC 5864102. PMID 28325798. - “Diabetes FAQ: General (Part 1 of 5) Section – What are mg/dL and mmol/L? How to convert? Glucose? Cholesterol?" . www.faqs.org
. - General Health Life (2005). "High Blood Sugar". Total Health Institute. Retrieved May 4, 2011.
- Giuliano D., Marfella R., Coppola L. et al (1997). “The vascular effects of acute hyperglycemia in humans are reversed by L-arginine. Evidence for decreased nitric oxide availability during hyperglycemia." Circulation
.
95
(7):1783–90. DOI: 10.1161/01.CIR.95.7.1783. PMID 9107164. - Florvall, Gösta; Basu, MD, Samar; Helmersson, PhD, Johanna; Larsson, M.D., Anders (2006). "The Hemocue urine albumin test shows complete agreement with results obtained with a large nephelometer". Diabetes care
.
29
(2): 422–423. DOI: 10.2337/diacare.29.02.06.dc05-1080. PMID 16443900. CS1 maint: multiple names: list of authors (link) - ↑
Ron Walls;
John J. Ratey; Robert I. Simon (2009). Rosen's Emergency Medicine: Expert Consult Premium Edition - Enhanced Online and Print Options (Rosen's Emergency Medicine: Concepts and Clinical Practice (2v.))
. St. Louis: Mosby. ISBN 978-0-323-05472-0. - Pearson, Ewan R.; Starkey, Brian J.; Powell, Roy J.; Gribble, Fiona M.; Clark, Penny M.; Hattersley, Andrew T. (2003). "Genetic cause of hyperglycemia and response to diabetes treatment." Lancet
.
362
(9392):1275–1281. DOI: 10.1016/s0140-6736(03)14571-0. PMID 14575972. S2CID 34914098. - Aronson, Ronnie; Brown, Ruth E; Li, Aihua; Riddell, Michael S (2019). "Optimal insulin adjustment factor for hyperglycemia following high-intensity exercise in adults with type 1 diabetes: the FIT study". American Diabetes Association
.
42
(1): 10–16. DOI: 10.2337/dc18-1475. PMID 30455336. - "High Blood Sugar". Total health institute. 2005. Archived from the original on 2013-08-17.
- Matthay, Josimer; Bigornia, Sherman J; Sotos-Prieto, Mercedes; Scott, Tammy; Gao, Xiang; Tucker, Catherine L (2019). "Mediterranean diet and 2-year changes in cognitive function by type 2 diabetes status and glycemic control". Diabetes care
.
42
(8):1372–1379. DOI: 10.2337/dc19-0130. PMC 6647047. PMID 31123154. - "Dietary Guidelines 2015-2020". US Department of Health. 2015
- Ma, Ronald C. W.; Popkin, Barry M (2017). “Intergenerational diabetes and obesity – a cycle that needs to be broken?” . PLOS ONE
.
14
(10): e1002415. DOI: 10.1371/journal.pmed.1002415. PMC 5663330. PMID 29088227. - ↑
Ishii, MD1, Hajime;
Suzuki, MD1, Hodaka; Baba, MD1, Tsuneharu; Nakamura, BS2, Keiko; Watanabe, M.D.1, Tsuyoshi (2001). "Seasonal variations in glycemic control in patients with type 2 diabetes mellitus". American Diabetes Association
.
24
(8): 1503. DOI: 10.2337/diacare.24.8.1503. PMID 11473100. - American Diabetes Association (2019). "Classification and Diagnosis of Diabetes: Standards of Medical Care for Diabetes - 2019" (PDF). Diabetes care
. 42 (Appendix 1) (Appendix 1): S13 – S28. DOI: 10.2337/DC19-S002. PMID 30559228. S2CID 56176183. - Inzucchi, Silvio E; Bergensthal, Richard M; Bus, John B; Diamond, Michaela; Ferrannini, Ele; Nauck, Michael; Peters, Anne L; Tsapas, Apostolos; Wender, Richard; Matthews, David R. (2012). "Management of hyperglycemia in type 2 diabetes: a patient-centered approach". Diabetes care
.
35
(6):1364–1370. DOI: 10.2337/dc12-0413. PMC 3357214. PMID 22517736. - Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT (2012). "The impact of physical inactivity on major noncommunicable diseases worldwide: an analysis of disease burden and life expectancy". Lancet
.
380
(9838):219–229. DOI: 10.1016/S0140-6736(12)61031-9. PMC 3645500. PMID 22818936. - Gujral, UP; Narayan K.M.V. (2019). "Diabetes in people of normal weight: high susceptibility in non-white populations". Diabetes care
.
42
(12):2164–2166. DOI: 10.2337/dci19-0046. PMC 6868465. PMID 31748211.
Diagnostics in our clinic
Diagnosis of hyperglycemia includes taking a medical history, analyzing clinical symptoms and a number of laboratory tests. A blood sugar test is taken in the morning on an empty stomach. In some cases, it becomes necessary to repeat the analysis after a few days to exclude possible stress factors.
In modern medicine, several methods of testing blood for sugar are used:
- rapid test for determining the approximate glucose concentration - can be carried out at home, but does not provide one hundred percent accuracy;
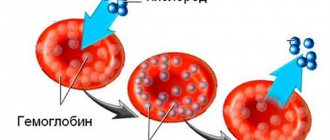
- analysis for glycated hemoglobin - allows you to determine the average glucose level over a certain period of time (1-3 months);
- Glucose tolerance test is a comprehensive study that involves taking blood from a finger prick four times over two hours (on an empty stomach and after taking glucose).
In a healthy person, the glucose level is 3.5-5.5 mmol per liter of blood. An indicator of 6 mmol is considered a prediabetic state. If the glucose concentration exceeds this value, the doctor has reason to diagnose diabetes mellitus.
When performing a glucose tolerance test, a result of up to 7.9 mmol/l is considered as normal. Diabetes mellitus is indicated by a value of over 11 mmol per liter.
Principles of treatment
If you have high blood sugar, you will need treatment to avoid life-threatening conditions. The complex of therapeutic measures includes:
- adherence to the principles of proper nutrition;
- regular monitoring of blood sugar levels - for this you can purchase a special device for home use - a glucometer. It is recommended to carry out the test several times a day. Urgent consultation with an endocrinologist is required if sugar levels increase repeatedly over a short period;
- regular physical activity;
- weight normalization;
- regular monitoring of blood pressure and cholesterol levels;
- taking medications to reduce blood glucose concentrations (insulin secretagogues, alpha-glucosiade inhibitors, etc.).
Treatment tactics are always selected individually depending on the reasons that led to the increase in blood sugar.
Hyperglycemia and diabetes mellitus
Hyperglycemia, or high blood sugar (glucose) , is a serious problem for people with diabetes. Hyperglycemia occurs when there is too much sugar in the blood. People with diabetes can develop two specific types of hyperglycemia:
- Fasting hyperglycemia is a blood sugar level above 130 mg/dL (7.2 mmol/L) after a person has not eaten for at least 8 hours.
- Postprandial or postprandial hyperglycemia is usually defined as blood sugar levels above 180 mg/dL (10 mmol/L). In people without diabetes, postprandial or postprandial blood sugar levels rarely exceed 140 mg/dL (7.7 mmol/L). Although sometimes 1-2 hours after a heavy meal, the sugar level can reach 180 mg/dL (10 mmol/L). Accordingly, elevated blood sugar levels after meals may indicate an increased risk of developing type 2 diabetes.
If a person with diabetes experiences frequent or prolonged periods of hyperglycemia, as indicated by high levels of glycosylated hemoglobin HbA1c in the blood, damage to nerves, blood vessels and other organs may develop. Hyperglycemia can also lead to the development of other more serious conditions, including ketoacidosis, which is more common in people with type 1 diabetes, and hyperglycemic hyperosmolar nonketonemic coma in people with type 2 diabetes and people at increased risk of developing it.
In order to prevent the development of complications of diabetes mellitus, it is very important to quickly treat the symptoms of hyperglycemia.
What leads to the development of hyperglycemia?
Hyperglycemia in diabetes mellitus can be caused by:
- Missed insulin injections or taking oral glucose-lowering medications
- Eating too many carbohydrates compared to the prescribed insulin dose or simply eating too many carbohydrates
- Eating too much food and calories
- Infectious diseases
- Diseases
- Stressful situations
- Decreased physical activity or doing less exercise than usual
- Exhausting physical activity
What are the symptoms of hyperglycemia in diabetes mellitus?
If you have diabetes, you should know the early signs of hyperglycemia. If left untreated, hyperglycemia can develop into ketoacidosis (if you have type 1 diabetes) or hyperosmolar coma (if you have type 2 diabetes), which are serious conditions that require emergency medical attention.
Early signs of hyperglycemia in diabetes mellitus are:
- Increased thirst
- Headache
- Trouble concentrating
- Blurred vision
- Frequent urination
- Increased fatigue (weakness, feeling tired)
- Weight loss
- Blood sugar level above 180 mg/dL (10 mmol/L)
Long-term hyperglycemia in diabetes mellitus can lead to the development of:
- Vaginal and skin infections
- Slow-healing cuts and wounds
- Decreased vision
- Nerve damage resulting in painful, cold or numb feet, hair loss on the lower extremities and/or erectile dysfunction
- Stomach or small intestine problems, such as chronic constipation or diarrhea
How is hyperglycemia treated in diabetes mellitus?
If you have diabetes and have any early signs of hyperglycemia, be sure to recheck your blood sugar levels several times. Before you call your doctor, you may want to write down a few of your blood sugar results. He or she will recommend the following for you:
- Drink more water. Water will help remove excess sugar from your urine and prevent dehydration.
- Do more exercise. They will help reduce the concentration of sugar in your blood.
Warning: If you have type 1 diabetes and your blood sugar level reaches 240 mg/dL (13.3 mmol/L), you should test your urine for the presence of ketone bodies. If they are, DO NOT exercise. If you have type 2 diabetes and your blood sugar concentration is above 300 mg/dL (16.6 mmol/L), even without ketone bodies, DO NOT exercise.
- Change your eating habits. You may need to see a nutritionist to change the amount and type of foods you eat.
- Change the medications you are taking. Your doctor may change the amount, timing, or type of diabetes medications you take. Do not change your drug treatment without first discussing it with your doctor.
If you have type 1 diabetes and your blood sugar levels are above 250 mg/dL (13.8 mmol/L), your doctor may want to test your urine for the presence of ketone bodies.
If your blood glucose concentration is consistently above 180 mg/dL (10 mmol/L) 1 to 2 hours after eating, or two repeat test results show levels above 300 mg/dL (16.6 mmol/L), call your doctor .
Next »