Myoglobin is a protein found in the heart and skeletal muscles.
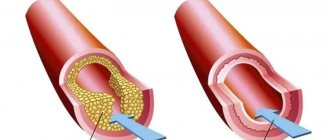
It traps oxygen in muscle cells, allowing them to produce the energy needed for muscle contraction. When the heart or skeletal muscles are damaged, myoglobin is released into the blood, where it circulates for several hours. It is then filtered from the blood by the kidneys and excreted from the body in urine. High concentrations of myoglobin are toxic to the kidneys, and in severe injuries, the release of myoglobin into the blood can lead to kidney failure.
Myoglobin can be used as an auxiliary test in the diagnosis of myocardial infarction, but it is not specific for this disease, since it is released into the blood when any muscle is damaged. One of the common causes of a sharp increase in myoglobin in the blood is rhabdomyolysis, the rapid breakdown of muscle tissue. It can be caused by severe injuries (for example, in a car accident), electric shock, burns, thrombosis, intoxication, certain infections (HIV, influenza, streptococcus), uncontrolled diabetes, hypo- and hyperthyroidism, and late-stage muscular dystrophies.
Detailed description of the study
Myoglobin is a specific protein found in muscle cells of skeletal muscles and the heart. Also, a small part of the protein can be synthesized in blood vessels, liver, and brain. It has a greater affinity for oxygen than hemoglobin. This determines two important functions of protein - the accumulation of oxygen in tissues and its use at critically low levels of oxygen in the muscle. Oxygen is transported to the mitochondria, where reactions occur to produce energy for the cells.
Myoglobin enters the blood when the myocardium and skeletal muscles are damaged. Myoglobin analysis is most often used to diagnose heart damage - myocardial infarction. It manifests itself as severe pain in the chest area, pain can radiate to the left arm, jaw, and stomach. Sweating, shortness of breath, nausea, and loss of consciousness are also sometimes observed. Symptoms mainly occur at rest.
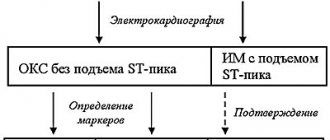
The advantages of myoglobin include the fact that this protein is the earliest marker of myocardial infarction. It very quickly enters the bloodstream when cardiomyocytes (heart muscle cells) are destroyed and can be detected within an hour after a heart attack. The indicator reaches its highest values after 4-12 hours and returns to normal within 24 hours. However, this analysis is not specific for infarction, therefore, to clarify the diagnosis, the analysis should be performed together with the determination of other markers of myocardial damage (troponin and creatine kinase-MB).
Myoglobin levels also increase when skeletal muscles are damaged due to the following diseases:
- Myositis is inflammation of muscle tissue. Symptoms include fever, muscle weakness and muscle pain.
- Myodystrophies are mainly represented by Duchenne or Becker muscular dystrophy. They are hereditary diseases and are accompanied by paresis, paralysis, cardiac disorders, and damage to the respiratory system. Duchenne muscular dystrophy manifests itself in early childhood with rapid progression of symptoms and immobility. Becker's dystrophy has a milder course, debuts later, at the age of 10-20 years, and is characterized by slowly increasing muscle weakness, which allows people with this disease to maintain the ability to walk independently for a long time.
- Compression syndrome, which occurs when long-term compressed areas of the body are released by heavy objects (during natural and man-made disasters, landslides). As a result, toxic substances (myoglobin, creatinine, potassium and calcium ions, lysosomal enzymes, etc.) are released into the blood from damaged tissues, which can lead to acidosis (increased blood acidity) and the development of renal failure.
It must be said that myoglobin is excreted unchanged by the kidneys. If their function is impaired (kidney failure), the level of protein in the blood may be elevated. Excessive protein excretion also has a negative impact on kidney function.
Thus, determining the level of myoglobin in the blood serum together with other markers makes it possible to timely diagnose myocardial infarction and diseases associated with damage to skeletal muscles, and therefore prescribe treatment in a timely manner and reduce the risk of complications.
When should a myoglobin test be performed?
Most often, determination of myoglobin level is required to confirm myocardial infarction. The basis for the analysis is the following symptoms experienced by the patient:
- chest pain radiating to the shoulder blade or neck
- severe shortness of breath, difficulty breathing, lack of air
- blood pressure surges
- numbness of limbs, cold sweat
- increased anxiety and fear in the patient
Taking a blood test to determine myoglobin levels requires special preparation. All factors that may affect the accuracy of the result should be excluded. The blood test is taken in the morning, on an empty stomach, the last meal should take place no later than 8-9 hours before the test. In the morning you can only drink plain water. Coffee, juices or tea are strongly discouraged as these drinks may interfere with the accuracy of the results.
Alcoholic beverages and smoking are prohibited. On the day of the test, the patient should be in a calm, relaxed state.
References
- Kuleva, N.V., Krasovskaya, I.E. New role of myoglobin in the functioning of cardiac and skeletal muscles. Biophysics, 2021. - T. 61(5). — P. 861-864.
- Clinical protocol for the diagnosis and treatment of progressive Duchenne/Becker muscular dystrophy, 2021. - 19 p.
- Chaulin, A.M., Duplyakov, D.V. Biomarkers of acute myocardial infarction: diagnostic and prognostic value. Clinical practice, 2021. - No. 3.
- Clinical protocol for the diagnosis and treatment of idiopathic inflammatory myopathies, 2021. - 29 p.
- Clinical laboratory diagnostics. National leadership. In 2 volumes / ed. V.V. Dolgova, V.V. Menshikov. - M.: GEOTAR-Media, 2012. - 928 p.
- Acute myocardial infarction with ST segment elevation of the electrocardiogram. Clinical guidelines, 2021. - 157 p.
What is cardiac troponin?
Troponins are a family of proteins that are found in skeletal muscle and cardiac muscle - the myocardium. There are three types of troponin: troponin C, troponin I and troponin T. Together they are involved in muscle contraction. Troponin I and troponin T are found only in cardiac muscle. These cardiac-specific troponins (also referred to as cTnI and cTnT) are normally practically not found in the blood. When myocardial injury occurs, cardiac troponins I and T enter the bloodstream in large quantities. The amount of troponins entering the blood directly depends on the amount of myocardial damage.
The most sensitive and specific for damage to the heart muscle is troponin I. If a person has a myocardial infarction, that is, the death of part of the heart muscle, the level of troponins in the blood increases 3-4 hours after the damage and can remain elevated for 10-14 days.
Role in the kitchen[edit]
Myoglobin contains hemes, pigments responsible for the color of red meat. The color of meat is determined in part by the degree of oxidation of myoglobin. In fresh meat, the iron atom is in the oxidation state of ferrous iron (+2) bound to an oxygen molecule (O 2 ). Well-done meat is brown because the iron atom is now in the ferric oxidation state (+3), having lost an electron. If meat has been exposed to nitrites, it will remain pink because the iron atom is bonded to NO, nitric oxide (eg corned beef or dry-cured ham). Grilled meats may also have a reddish-pink "smoke ring" caused by the binding of the heme center to carbon monoxide. [20] Raw meat packaged in a carbon monoxide atmosphere also has the same pink "smoke ring" due to the same principles. It is noteworthy that the surface of this raw meat also has a pink color, which in the minds of consumers is usually associated with fresh meat. This artificially induced pink color can last up to one year. [21] Hormel and Cargill reportedly use this meat packaging process, and meat processed this way has been on the consumer market since 2003. [22]
Further reading[edit]
- Kollman JP, Bulatov R, Sunderland SJ, Fu L (February 2004). "Functional analogues of cytochrome c oxidase, myoglobin and hemoglobin". Chemical Reviews
.
104
(2):561–88. DOI: 10.1021/cr0206059. PMID 14871135. - Reeder BJ, Svistunenko DA, Cooper CE, Wilson MT (December 2004). "Radical and redox chemistry of myoglobin and hemoglobin: from in vitro studies to human pathology." Antioxidants and redox signals
.
6
(6): 954–66. DOI: 10.1089/ars.2004.6.954. PMID 15548893. - Schlieper G, Kim JH, Molojavyi A, Jacoby C, Laussmann T, Flögel U, Gödecke A, Schrader J (April 2004). "Adaptation of myoglobin knockout mice to hypoxic stress". American Journal of Physiology.
Regulatory, Integrative and Comparative Physiology .
286
(4):R786-92. DOI: 10.1152/ajpregu.00043.2003. PMID 14656764. S2CID 24831969. - Takano T (March 1977). “The structure of myoglobin has been refined with a resolution of 2-0 A. II. Structure of sperm whale deoxymyoglobin." Journal of Molecular Biology
.
110
(3):569–84. DOI: 10.1016/S0022-2836 (77) 80112-5. PMID 845960. - Roy A., Sen S., Chakraborty A.S. (February 2004). "Nonenzymatic glycation in vitro enhances the role of myoglobin as a source of oxidative stress." Free Radical Research
.
38
(2): 139–46. DOI: 10.1080/10715160310001638038. PMID 15104207. S2CID 11631439. - Stewart, J. M., Blakely, J. A., Karpovich, P. A., Kalanshi, E., Thatcher, B. J., Martin, B. M. (March 2004). "Unusually weak oxygen binding, physical properties, partial sequence, autoxidation rate, and potential phosphorylation site of beluga whale (Delphinapterus leucas) myoglobin." Comparative biochemistry and physiology
B.
137
(3):401–12. DOI: 10.1016/j.cbpc.2004.01.007. PMID 15050527. - Wu, G., Wainwright, L. M., & Poole, R. C. (2003). Microbial globins
.
Advances in microbial physiology. 47
. pp. 255–310. DOI: 10.1016/S0065-2911(03)47005-7. ISBN 9780120277476. PMID 14560666. - Mirceta S., Signor A. V., Burns J. M., Cossins A. R., Campbell K. L., Behrenbrink M. (June 2013). "The evolution of mammalian diving ability tracked by the net surface charge of myoglobin". The science
.
340
(6138): 1234192. DOI: 10.1126/science.1234192. PMID 23766330. S2CID 9644255.. Also see the Proteopedia article on this discovery.
What are muscle hemoglobin molecules?
Myoglobin is a protein that is present in striated muscles, similarly located in myocardial tissue. Myoglobin is part of a group of chromoprotein molecules.
Myoglobin contains a gene that is interconnected with part of the body’s proteins and is part of the prosthetic group. The myoglobin molecule contains amino acid components.
A protein is a monomer that consists of a single chain.
There are structures of a protein molecule:
- The primary structure is the monomer stage, consisting of a polypeptide linking chain, which includes amino acid residues,
- The structure of the secondary confirmation stage , which has an α-helical shape and 75.0% of molecules have this structure,
- The tertiary type structure has an α-helical shape, which is folded into a compact globule.
To determine the structure of a tertiary species, an X-ray analysis method is needed.
Normal myoglobin index
Standard indicators may increase upward and depend on laboratory research methods:
- Diagnostic test – immuno-nephelometric,
- RIA radioimmunoassay analysis,
- Study using immunofluorescence analysis.
Despite the varying sensitivity of laboratory tests, the volume of myoglobin does not exceed the index from 65.0 to 80.0 μg/l.
Standard indicator:
- For representatives of the stronger sex from 19.0 to 92.0 μg/l,
- For the female body from 12.0 to 76.0 μg/l,
- The average normative coefficient is 49.0, and also more or less by 17.0 units (for males),
- The average standard for women is 35.0, and also more or less by 14.0,
- The concentration of myoglobin molecules in urine is less than the index of 20.0 μg/l; in an absolutely healthy body, myoglobin protein should not be present in urine.
When the myoglobin index in the blood differs from the normative units, then myoglobinemia is diagnosed.
If the presence of myoglobin in urine is detected during the analysis, then a diagnosis of myoglobinuria is made.
Index increased
Physiological increase in muscle type hemoglobin. The causes are related to the load on the skeletal muscle tissue, especially during sports and training, as well as when using physical therapy with electrical impulses.
A pathological increase in the index occurs in the following diseases:
- Damage to the heart muscle during myocardial infarction (hemoprotein increases, and the level of creatine kinase also increases). Myoglobin increases 30 minutes after the onset of pain, and its presence can be detected even 3 days after the attack,
- Kidney failure and uremic syndrome,
- Inflammation that occurs in muscle tissue
- In case of injury,
- Deep thermal tissue burns,
- Chemical burns in muscle tissue,
- Muscle cramps,
- After surgery,
- Muscle dystrophy.
Index downgraded
The muscle type hemoglobin index in the blood decreases only under the influence of pathology, such as:
- Arthritis of rheumatoid type,
- Inflammation of muscle tissue polymyositis,
- Myasthenia gravis is the presence of antibodies in the blood that affect myoglobin.
Polymyositis
Material and methods
The myoglobin content in the blood of 30 (19 men and 11 women aged 41-94 years) corpses who died as a result of acute cardiovascular failure and chronic coronary heart disease was determined. Blood sampling was carried out at autopsy no later than 35 hours after death. Blood was taken in an amount of 10 ml with a dry syringe from the femoral vein of the corpse into a sterile bottle, according to paragraph VII, Chapter 88 of Order No. 346n of the Ministry of Health and Social Development of the Russian Federation. dated 12.05.10 “On approval of the procedure for organizing and conducting forensic medical examinations in state forensic institutions of the Russian Federation.” Two methods were used: a passive hemagglutination reaction with the erythrocyte diagnosticum DS-ERYTHRO-MYOGLOBIN NPO Diagnostic Systems and an immunoturbidimetric test with the DiaSys Diagnostic Systems GmbH kit. The technique using erythrocyte diagnosticum is semi-quantitative: a visual assessment of the presence of hemagglutination is made depending on the degree of dilution of the test sample. Immunoturbidimetric test - quantitative: a fixed time method is used. It is based on the photometric measurement of the antigen-antibody reaction between anti-human myoglobin antibodies immobilized on latex particles and the myoglobin present in the sample. Statistical processing of the results was carried out using the BIOSTAT software package. Spearman correlation was used to analyze the correlation between the data from the two samples.
What is the normal level of troponin in the blood?
Reference values: <0.29 ng/ml. Usually the level of troponin I in the blood is so low that it cannot be measured. Therefore, even a slight increase may indicate heart damage.
A significantly elevated troponin I level is very likely to indicate a myocardial infarction or other heart damage. If a person suffering from angina or complaining of heart pain does not have elevated levels of troponin I, this excludes the possibility of heart damage.
What are the reasons for increased troponin I levels in the blood?
The main reason for the increase in troponin I concentration is the death of cardiac muscle cells, which most often occurs during myocardial infarction. After a heart attack, troponin I levels remain elevated for 10 to 14 days.
Much less commonly, troponin I may increase due to the following reasons.
- Myocarditis – infectious inflammation of the heart muscle
- Pericarditis – inflammation of the lining of the heart
- Pulmonary embolism – blockage of the pulmonary artery by a blood clot, leading to restriction of blood flow in the lung area
- Heart injury, including surgery
full list of questions
‹ Previous page | Next page >
Conclusion
With proper distribution of the load on the muscle group and a healthy, balanced diet and lifestyle, myoglobin will be within standard values.
The role of this protein is very important in the human body: providing oxygen to muscle cells, transporting oxygen to its destination and transporting carbon dioxide to the lungs.
With a normal reading of myoglobin in the blood, there will be an uninterrupted operation of the gas exchange process in the body for the proper functioning of life-supporting organs.
(
1 ratings, average: 5.00 out of 5)