heart transplantation
Until recently, decompensated heart failure was considered a death sentence. However, today, when medicine has stepped forward, heart transplant techniques have appeared, patients have a chance to live. But, despite all the progress, heart transplantation is still considered a complex, high-tech operation that requires careful preparation.
Indications for heart transplantation
For transplantologists, careful selection of the recipient – the patient who will receive a heart transplant – is important. First of all, we consider those people who are no longer helped by medications, but who can return to an active life if they have a healthy organ. Indications for surgery are:
- left ventricular ejection fraction less than 20%;
- Na in blood serum is less than 135 mEq/l;
- wedge pressure in the pulmonary artery more than 25 mmHg;
- the level of norepinephrine in the blood plasma is more than 600 pkg/ml;
- cardiothoracic index more than 0.6;
- decrease in maximum VO2 less than 10 ml\kg\min.
It is important that these indicators remain intact with the maximum possible drug support. With these indicators, the prognosis for one-year survival without a heart transplant is less than 50%.
ASK ANY QUESTION ABOUT HEART TRANSPLANTATION TO SPECIALISTS OF LEADING CLINICS
Heritage
In 1996, Michael DeBakey, a renowned surgeon who was to become a consultant on President Yeltsin’s upcoming operation, came to Moscow, and the first thing he asked was: “Can I bow to Academician Demikhov?” Demikhov was found with difficulty. The state remembered the outstanding surgeon and then awarded the first and only order - “For Services to the Fatherland”, III degree.
Demikhov’s works are known and remembered all over the world - Christian Barnard was not lying when he called Vladimir Petrovich the father of transplantology.
Preparing the patient for surgery
Heart transplantation is a complex procedure that requires careful preparation. The patient undergoes a multi-stage examination before a decision is made about the possibility of organ transplantation. Necessary:
- carefully collect anamnesis of the disease;
- perform a chest x-ray;
- take a maximal oxygen uptake (VO2) stress test;
- undergo a series of tests for infections to exclude hepatitis, HIV and a number of other diseases that may be a contraindication;
- undergo routine urine and blood tests to assess the general condition of the body;
- undergo cardiac catheterization with tonometry of the right side (necessary to exclude pulmonary hypertension, which will be a contraindication to transplantation);
- take a test to evaluate human lymphocyte antigen (HLA);
- undergo an ECG, EchoCG.
The examination may reveal both absolute and relative contraindications that exclude the patient from being placed on the waiting list for a donor heart.
Unplanned xenotransplantation
Unplanned xenotransplantation
James Hardy had been researching organ transplantation since the mid-1950s and successfully performed the first human lung transplant in 1963. The doctor was willing to perform a heart transplant. The opportunity presented itself in January 1964: 68-year-old Boyd Rush was admitted to the University of Mississippi Medical Center. Here's what was known about him:
- the lower part of the left leg was black with gangrene;
- the face was covered with blood clots;
- Boyd Rush suffered from hypertension for many years;
- the day before, Rush had suffered a heart attack.
Dr. Hardy was the only person who thought he could help Rush. The doctor amputated his leg. Afterwards it was necessary to find a donor heart, but difficulties arose with this, and Rush was already on the verge of death. Then Hardy decided not to waste time and use the organ of a large chimpanzee. The doctor asked his assistant colleagues if they were ready to do this: four voted in favor, the fifth abstained. The operation took place. The transplanted heart beat for about 90 minutes and then stopped: its size was insufficient to save the person’s life.
Subsequently, James Hardy and the doctors involved in the operation were criticized: the idea of organ transplantation and the transplantation of a monkey's heart into a human caused ethical controversy. The outrage subsided somewhat after the doctor published an article in the Journal of the American Medical Association describing the strict ethical principles he and his team followed in evaluating the donor and recipient.
Transplantation technique
Due to decompensation of the disease, not all patients have the opportunity to immediately undergo transplantation. If the patient's condition is unsatisfactory, they can use:
- Pharmacological bridge to transplantation is a technique in which the patient’s condition is brought to satisfactory with the help of medications (mainly infusion ionotropic agents).
- A mechanical bridge to transplantation is a technique based on mono- or biventricular bypass of the ventricles or the use of an artificial heart in the preoperative period.
The operation takes place under conditions of established artificial circulation. Transplantation can be performed heterotopically or orthotopically. In the first case, the donor heart is placed under the patient's heart without removing the latter. This technique is used for severe hypertension in the pulmonary circulation. In other cases, a donor heart replaces the patient's own organ.
Crisis and later years
By 1965, Demikhov, already a Doctor of Science, a world-famous transplant surgeon, was aiming for new heights: at one of the meetings of the Society of Transplantologists he was going to present a project for organ conservation. Demikhov wants to create a bank of animals that would house the organs of deceased donors. But not everyone likes the idea.
Petrovsky, who once met Demikhov by chance during the war, did not forget the arrogant, from his point of view, laboratory assistant. By 1965, he became Minister of Health and tried to destroy his rival. He writes about Demikhov :
“Demikhov is certainly an interesting person, a fanatic, and spoiled by the lack of leadership. From the surgeon's point of view, it has very large defects. From a physiological point of view, there is a complete lack of experimental control. He performs the operation and then does not monitor the dog. Dogs often die from bleeding. He has no surgical training. It works on a pure idea.”
Source
When Vladimir Petrovich talks about his idea at the transplantology section, those present accuse him of quackery. The chairman of the section, Professor Ostroverkhov, reproaches Demikhov for the low level of his experiments and calls Demikhov’s experiments “nonsense.” Everyone is silent. To defend Demikhov means to directly go against Petrovsky. But one person still stands up - Tatyana Andreevna Grigorieva, head of the department of histology at the 2nd Moscow Medical Institute.
“What is happening is not a meeting of a scientific society. This is a vile trial of an outstanding scientist of the world,” says Grigorieva.
Others stand behind her, and most importantly, they give Demikhov himself the opportunity to speak. In the end, the scientist is acquitted, but both he and his supporters know that this is only the first attack. Demikhov is not broken yet, but he is already close to it. His health begins to deteriorate due to the nervous tension he has experienced.
A few years later, the state decides to take away Demikhov’s new apartment, justifying this by the fact that it was given to him by accident, by mistake. Demikhov is getting worse. His wife Liya Nikolaevna said that Demikhov was on the verge: he decided that if they came to evict him, he would throw himself out the window - but he would not complain.
Then the director of the Sklifosovsky Institute stands up for him, winning Demikhova a few more years.
In 1968, Demikhov suffered a stroke. He never recovered from it, but continued to work - his laboratory existed until 1986, and in 1988, Demikhov, as part of a group of surgeons, was awarded the State Prize for introducing bypass surgery into practice.
Gradually, the great scientist began to lose his memory and towards the end of his life he did not even leave the house alone. By the 1990s, he was almost completely forgotten, but most of his ideas not only came true, but also became absolutely routine - both coronary bypass surgery and organ transplants are now found everywhere.
On November 22, 1998, Vladimir Petrovich died from a ruptured aneurysm.
Postoperative period
After the operation, the patient is under medical supervision for a long period of time. During this period, immunosuppressive therapy with the help of hormones and cytostatics is selected, thanks to which it is possible to avoid rejection processes, the condition of the postoperative wound is assessed, and complications are corrected if they arise.
In the first month after surgery, a myocardial biopsy is performed every 1.5-2 weeks. This is necessary to assess the condition of the donor heart. Over time, this procedure is performed less and less often.
2.Rehabilitation after surgery
What to expect after heart transplant surgery?
Recovery process after heart transplant surgery
similar to other heart surgeries.
You will most likely spend a couple of weeks in the hospital. In some cases, you will need more time depending on how your health is assessed and whether there are complications after surgery. At the hospital, you will begin a cardiac rehabilitation program.
. Your doctors will check to see if the donor heart is taking root in your body.
Rehabilitation after heart transplant
A rehabilitation program will help you recover and become active again after your heart transplant.
The donor heart can respond to stress in different ways. Your heart rate will not rise as much as before. The heartbeat will also return to normal in a different way. This occurs because some of the nerve connections that control the heart were cut during surgery.
Visit our Cardiology page
World experience and prices
As practice shows, a transplanted heart, if all medical recommendations are followed, can work without interruption for 5-7 years. However, the aging process in the donor organ proceeds faster than in its own, and therefore sooner or later the patient will note the return of all symptoms of heart failure.
The actual practice of heart transplantation differs significantly from country to country. In some countries, these operations are not carried out at all because they are not regulated at the legislative level. In other countries, such operations are clearly regulated and both residents of the country itself and foreign citizens can resort to it. For example, in the Republic of Belarus, organ transplantation is carried out in accordance with the law, which is based on the “presumption of consent”: organ collection from a donor can be carried out after declaring brain death, unless wishes to the contrary are expressed by the patient before death. The organ can be used for further patients in need.
SELECT A FREE CLINIC FOR HEART TRANSPLANTATION
Among the factors leading to deterioration of the condition of the transplanted heart in the long term, specific graft vasculopathy is especially distinguished. However, this is only one of the significant factors, the final result of which is the development of post-transplant restrictive cardiomyopathy [1, 3, 5].
Understanding the reasons for failure in the long-term period after heart transplantation is the main opportunity to overcome the stagnation of results. This publication provides an analysis of the clinical results and histological and ultrastructural organization of the myocardium of the donor heart, based on the study of heart biopsies of patients who survived 10-22 years after transplantation.
Material and methods
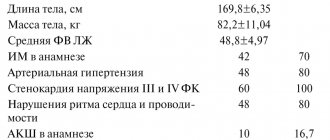
By July 2012, at the Russian Scientific Center for Surgery named after. acad. B.V. Petrovsky performed 29 orthotopic heart transplantation operations. 23 patients survived the hospital period (1-3 months p/o) - hospital mortality was 20.7%. A detailed analysis of the results and causes of failure during the hospital period and the first 10 years after transplantation is presented in our earlier publication [1].
9 (45%) patients survived the ten-year period, 5 - 15 years, of which 2 people have already lived more than 20 years after surgery.
Ultrastructural studies of the myocardium and microvasculature were performed regularly from the 10th to the 22nd year after transplantation in 6 recipients (5 men and 1 woman) aged from 33 to 66 years (average age - 47.6 years). Coronary angiography followed by biopsy of the right ventricle was performed annually (or twice a year).
Biopsy samples obtained from each recipient were studied: 3-4 samples from the wall of the right ventricle and the interventricular septum. One of the biopsy specimens, after routine histological processing, was embedded in paraffin and the prepared sections were stained with hematoxylin and eosin and Massan. Semi-thin sections were prepared from other samples embedded in epoxy resin and, after removing the resin, stained with histological dyes: hematoxylin and eosin, toluidine blue, and hyacinth violet.
Ultrathin sections with a thickness of 50-70 nm were prepared from the same blocks, contrasted with uranyl acetate, lead citrate, viewed and photographed in a JEM-100CX electron microscope at an accelerating voltage of 80 kV with a magnification from 5000 to 32,000.
Results and discussion
The morphological picture in the myocardium of the donor heart had similar qualitative changes in the long-term period after surgery (more than 10 years), despite clinical differences between recipients (gender, age, initial diagnosis, features of the postoperative period and treatment). This allows us to assume certain patterns in the process of morphological adaptation of donor hearts in general (see table).
The state of the microvasculature had an uneven mosaic character.
Patient K. There was a pronounced reduction of the microvasculature, which progressed over time. But even these few capillaries were often surrounded by a connective tissue “muff”. Electron microscopy revealed a sharp expansion of the basement membrane of the capillaries. Over the years, the decrease in the density of the microvasculature became even more pronounced.
Patient P. The walls of the capillaries are tortuous, thinned, unevenly expanded; signs of “sludge” of blood cells in the lumen of the capillaries could often be seen. Small intramural arteries and arterioles had thickened, homogenized walls, sometimes their lumen was practically not defined (Fig. 1).
Figure 1. Micrograph. Myocardium of patient P. Thickening of the wall of a small artery, the lumen is practically not defined. Semi-thin section, stained with hematoxylin and eosin. About. 60, approx. 10.
Electron microscopy revealed that the endothelial cells of the capillaries were thinned, and the level of micropinocytosis in them was reduced. Over time after transplantation, the number of capillaries per unit area visually decreased.
Patient Sh. The number of capillaries is noticeably reduced. The endothelium of the capillaries is thickened and thinned in some places. The lumen of the vessels was expanded, the “sludge” phenomenon was observed, as well as the adhesion of blood cells to the capillary wall. Diapedetic hemorrhages occurred. Over time, this structure of the microvasculature did not change significantly.
Patient G. By the 10th year of research, the capillary bed was practically unchanged, however, thickening and homogenization of the wall were noted in some arterioles. Over time, a gradual decrease in the density of the capillary bed, perivascular sclerosis, and a decrease in the level of micropinocytosis in the endothelial cells of the capillaries were revealed; in some capillaries, tortuosity of the luminal surface was noted, sometimes with the separation of protruding parts of the endothelial cells into the lumen of the vessel (Fig. 2).
Figure 2. Micrograph. Ultrastructure of the myocardium of patient G., tortuosity of the luminal surface of the capillary with separation of parts of endothelial cells into the lumen of the capillary. Ultra-thin section, double contrast. Uv. 12,000. Adhesion of blood cells to the surface of endothelial cells was often observed. The walls of the microvessels were sharply osmiophilic—impregnated with plasma; diapedetic hemorrhages were observed in the myocardial interstitium near the vessels.
Patient R. Entire myocardial fields were observed, where individual hibernating cardiomyocytes were immured among masses of fibrous tissue (Fig. 3).
Figure 3. Micrograph. Myocardium of patient R. Fields of interstitial sclerosis, single cardiomyocytes with signs of hibernation are “immured” in the thickness of the sclerotic interstitium. Semi-thin section, stained with hematoxylin and eosin. About. 40, approx. 12. Other areas of the biopsy specimens were sharply hypertrophied cardiomyocytes, among which single capillaries were found in the layers of connective tissue.
Patient Kr. There was a sharp expansion of the capillary bed, plethora of microvessels; there was no visible decrease in the density of the capillary bed during the entire observation period (Fig. 4).
Figure 4. Micrograph. Myocardium of patient Kr. Expansion of the capillary bed, signs of “sludge” of formed elements in microvessels. There is no visible decrease in the density of the capillary bed. Semi-thin section, stained with hematoxylin and eosin. About. 20, approx. 12.
There was an increase in the electron density of the cytoplasm of endothelial cells, apparently associated with their plasma impregnation. Over time after transplantation, the state of the microvasculature did not change significantly.
Changes in cardiomyocytes and the interstitial substance of the myocardium of the donor heart also had similar features with certain quantitative differences.
In the long-term period after transplantation
There were no episodes of pronounced rejection reactions.
Some cardiomyocytes are in a state of dedifferentiation, characteristic of the hibernation state: atrophy and loss of striation of myofibrils, accumulation of glycogen and small mitochondria in the central part of the cardiomyocyte (Fig. 5, a).
Figure 5. Micrograph. Ultrastructure of the myocardium of the right ventricle of a transplanted heart 20 years after surgery. a — chromatin margination in the nucleus; accumulation of small enlightened mitochondria, devoid of intermitochondrial contacts, uv. 11,000.
Another group of cardiomyocytes has oddly shaped nuclei containing large nucleoli, often with accumulation of chromatin at the periphery. In this case, mitochondria have different electron densities, are reduced in size, and the specific contours between them are disrupted. Taken together, this indicates both the initial signs of apoptotic degeneration and an extensive form of apoptosis of cardiomyocytes with the formation of apoptotic bodies (see Fig. 5, b).
Figure 5. Micrograph. Ultrastructure of the myocardium of the right ventricle of a transplanted heart 20 years after surgery. b — advanced phase of apoptosis of cardiomyocytes, condensation of nuclear remnants and organelles, beginning of the formation of apoptotic bodies, uv. 12,000.
And finally, as the duration of the post-transplantation period increases, in the myocardium of the donor heart, cells with large nuclei and a narrow rim of cytoplasm are more often detected in the immediate vicinity of cardiomyocytes, which, by their morphology, can be classified as pluripotent (stem?) cells (see Fig. 5 , V).
Figure 5. Micrograph. Ultrastructure of the myocardium of the right ventricle of a transplanted heart 20 years after surgery. c - a cell with a large nucleus and a narrow rim of cytoplasm (near the modified cardiomyocytes), resembling a stem cell in ultrastructure, uv. 12,000.
It is important that in the long-term period after surgery the number of capillary vessels per unit area of myocardial section decreases. This process is natural, but uneven and is expressed to varying degrees in different patients.
An electron microscopic study showed that over time, in biopsy samples of a transplanted heart, the capillary becomes an almost rare structure. The preserved capillaries are often surrounded by a connective tissue “muff”.
It can be assumed that progressive microcirculation disorders may underlie chronic ischemia of the donor myocardium, resulting in hibernation and apoptosis of cardiomyocytes [2].
We have previously reported that from the first months after transplantation, all recipients experience hyperlipidemia, which is more pronounced with the initial diagnosis of ischemic cardiomyopathy. It was this fact that served as the basis for the fact that since the mid-90s we have included exchange plasmapheresis in the mandatory protocol for postoperative therapy [4]. Planned plasmapheresis sessions, starting from the first month after transplantation, were performed in only one patient, Kr., who underwent anatomical heart transplantation 16 years ago. Then they were repeated at least 3-4 sessions annually. Despite the constant tendency towards severe hyperlipidemia and initial severe ischemic heart disease, it was in this recipient that minimal microcirculation disorders were noted in the donor heart. In our opinion, this observation requires careful further analysis.
An interesting and significant fact is that after 10 years, not a single recipient showed morphological signs of a rejection reaction. Despite this, coronary angiography is absolutely necessary for these patients (sometimes 2 times a year!) for the timely detection of local stenoses in the epicardial coronary arteries and the performance of angioplasty in order to prevent myocardial infarction.
Data obtained from ultrastructural study of the donor heart correlate with the results of clinical and functional monitoring of recipients in the long-term period after transplantation. Transplant dysfunction begins to develop according to the diastolic type of heart failure, which is based on increasing myocardial sclerosis (subendocardial, interstitial). Compensatory hypertrophy of functioning cardiomyocytes (in the absence of a rejection reaction) allows maintaining normal ejection fraction values for a long time. According to M. Bilingham and C. Berry [3], the myocardial mass of a transplanted heart increases significantly with time from the moment of transplantation.
Thus, the condition of the donor heart in the long-term period after transplantation (dystrophy-hypertrophy of cardiomyocytes, impaired microcirculation, interstitial sclerosis) can, in our opinion, be considered as a special form of post-transplantation cardiomyopathy, the causative factors of which cover all periods of possible myocardial damage, starting from the donor stage .
Demikhov's idea
Even during the war, Demikhov came up with the idea of supplying the myocardium with blood, bypassing the plug. It is necessary to transfer the internal mammary artery to the heart and stitch it with the coronary artery below the site of sclerotic narrowing. This bypass is called a shunt. The first bypass proposed by Demikhov – mammaro-coronary (from the word “mammaria”, the Latin name for the thoracic artery) – turned out to be the most reliable.
Bypass surgery must be performed quickly, without leaving the heart without power for a long time. The war gave rise to a solution to this problem: vascular stapling devices appeared. There was only no surgical hospital where they would decide on such an operation. Demikhov started alone. Without money, connections or medical education.
Go to action
Arriving from the front in Moscow, he got a job teaching physiology at the Fur Institute, where he received premises for experiments. Then I found my classmate Aron Gurvich, with whom I had once argued a lot about immunity. Wounded in the war, Gurvich worked at the Institute of Biological and Medical Chemistry. He helped a friend - he brought morphine for anesthesia from work and caught two stray puppies in Neskuchny Garden. On February 23, 1946, the heart of one dog was transplanted into another, and the recipient lived with both hearts for 15 minutes. This was done without hypothermia, a heart-lung machine, or immune suppression drugs.
In the same year, Demikhov managed to transplant both a heart and lungs into a dog, and the animal lived for 6 days. This was the end of the researcher’s work at the Fur Institute - the authorities considered that he was doing nonsense.
Sources
- Toker E., Aktaş S. The childbirth experiences of Syrian refugee mothers living in Turkey: a qualitative study. // J Reprod Infant Psychol - 2021 - Vol - NNULL - p.1-17; PMID:33896296
- Wang B., Zhao D., Lu T., Liu S., Rong C. Quantifications and Applications of Relative Fisher Information in Density Functional Theory. // J Phys Chem A - 2021 - Vol - NNULL - p.; PMID:33891419
- Dimentberg E., Cardaillac C., Richard E., Plante AS., Maheux-Lacroix S. Translation and Cultural Validation of the WERF EPHect Endometriosis Patient Questionnaire into Canadian French. // J Obstet Gynaecol Can - 2021 - Vol - NNULL - p.; PMID:33887447
- Bhandari D., Kotera Y., Ozaki A., Abeysinghe S., Kosaka M., Tanimoto T. COVID-19: challenges faced by Nepalese migrants living in Japan. // BMC Public Health - 2021 - Vol21 - N1 - p.752; PMID:33874937
- Samkange-Zeeb F., Samerski S., Doos L., Humphris R., Padilla B., Bradby H. “It's the First Barrier” - Lack of Common Language a Major Obstacle When Accessing/Providing Healthcare Services Across Europe. // Front Sociol - 2021 - Vol5 - NNULL - p.557563; PMID:33869495
- Elshahat S., Newbold K.B. Physical activity participation among Arab immigrants and refugees in Western societies: A scoping review. // Prev Med Rep - 2021 - Vol22 - NNULL - p.101365; PMID:33868904
- Ono K., Yoshioka N., Hage D., Ibaragi S., Tubbs RS., Iwanaga J. Correction to: Duplication of the external jugular vein: a language barrier of database search in classic anatomical studies. // Surg Radiol Anat - 2021 - Vol - NNULL - p.; PMID:33856506
- Noack E.M., Schulze J., Müller F. Designing an App to Overcome Language Barriers in the Delivery of Emergency Medical Services: Participatory Development Process. // JMIR Mhealth Uhealth - 2021 - Vol9 - N4 - p.e21586; PMID:33851933
- Schrot-Sanyan S., Kolanska K., Haimeur Y., Varlas V., Parisot-Liance L., Daraï E., Bornes M. Language barrier as a risk factor for obstetric anal sphincter injury—A case-control study. // J Gynecol Obstet Hum Reprod - 2021 - Vol50 - N8 - p.102138; PMID:33831603
- Kyaw PP., Geater AF. Healthcare seeking preferences of Myanmar migrant seafarers in the deep south of Thailand. // Int Marit Health - 2021 - Vol72 - N1 - p.1-9; PMID:33829467
Animals can also change body parts
The driver explained to him that any part in the car can be replaced – it’s always like new. And then he uttered a phrase that decided the fate of world transplantology: “Animals can also change body parts.” And he said that the lizard grows a new one instead of a severed tail. Volodya immediately asked questions: “will the dog also grow a new tail?”, “and why does blood come from a cut off tail?” The teacher explained that a dog has a heart that pumps blood. Soon the mother caught Volodya with a knife in his hand, when he was about to cut the puppy’s side and understand how the heart works. The puppy was saved, but the son was flogged for being a knacker. It didn’t help: young Demikhov fell ill with a thirst for anatomical knowledge. Realizing that he would not make a gardener, his family sent Volodya to study.