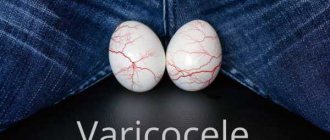
Varicocele - dilation of the veins of the spermatic cord in men - is a widespread disease, found in 16.2% of adult men. The highest incidence of varicocele (15-19%) occurs at 14-15 years of age. In children under 10 years of age, varicocele is much less common, in 0.7-5.7% of cases. In addition to aesthetic problems and some painful symptoms, varicocele contributes to infertility: 30-40% of men examined for infertility are diagnosed with this pathology. The disease's mechanism of development resembles pelvic varicose veins in women and is treated according to similar principles.
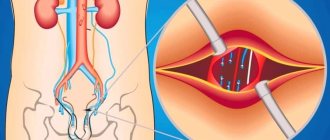
Most often, varicocele develops due to compression of the left renal vein between the superior mesenteric artery and the aorta with a congenital acute angle of origin. This leads to difficulty in venous outflow from the left kidney and reverse flow (reflux) of venous blood through the testicular vein.
Statistics on varicocele: why you need to see a urologist during puberty
The content of the article
Typically, pathology develops in young men during puberty. It is during this period that the disease reaches its peak, which, with timely detection and treatment, can be prevented.
Statistics show how high the risk of remaining infertile is for any young man who does not attend routine examinations with a urologist. According to her data, every fifth man over the age of 17 suffers from varicocele. In a third of cases, the pathology reduces the ability to conceive (fertility).
Prevention
It is easier to prevent any disease than to treat it, so it is necessary to carry out preventive measures.
Measures aimed at reducing the risk of developing pathological dilation of veins in the scrotum:
- healthy eating has a beneficial effect on the intestines;
- taking vitamins;
- use contraception during sexual intercourse;
- reasonable physical activity;
- Regular visits to the doctor from adolescence.
Reasonable adherence to preventive measures not only minimizes the risk of developing the disease and its relapse, but also contributes to the choice of an effective and less invasive treatment method.
Causes of nodular veins in the testicles
Varicose veins of the testicles can have 2 forms:
- Primary - occurring as an independent disease.
- Secondary, when the pathology is a complication of other diseases.
Causes of varicocele:
- Heredity is a genetic predisposition
. Anomalies in the development of veins in most cases are inherited, being detected in adolescents during the period of maturation (puberty). Weak veins and vein valve defects or absence of vein valves are common, causing veins to stretch easily when blood flow increases. - Anatomical structure
. The main cause of varicocele is strangulation of the left renal vein. When pinched, testicular varicose veins are a complication associated with a powerful influx of venous blood. Symptoms appear only in a vertical position; in a horizontal position, the venous network is normal. - Tumors
in the pelvis and abdominal cavity. Large tumors infringe on the veins leading to the testicles. The pressure stretches the venous walls. - Constriction of veins
. The blood flowing in the veins presses harder, gradually stretching the walls. - Lifting weights, heavy loads during training
. When lifting weights, the abdominal muscles tense, which leads to a rush of blood to the extremities. Under load, veins that are prone to stretching expand sharply, causing varicocele. - Constipation
, diarrhea. With chronic constipation, a man has to strain, which again affects the blood flow in the lower part of the body. A similar situation occurs with prolonged diarrhea.
Excess weight and sexual activity contribute to the development of varicose veins.
Diagnostics
An angiosurgeon or phlebologist can easily identify varicicole. Diagnosis determines the relationship between symptoms and treatment for varicicole. Primary diagnosis consists of collecting anamnesis - interviewing the patient about the nature and presence of complaints, their dependence on physical activity or injuries received.
At certain stages of the disease, physical examination reveals visible varicose nodes, and palpation gives an idea of plexuses in the bunch. A sign of pathology is laxity of the affected testicle. Palpation must be carried out standing and lying down under pressure and in a calm state, which makes it possible to clarify the localization of the diagnosis.
Instrumental diagnostic methods:
- with varicicol, ultrasound is done for the abdominal cavity, including the kidneys;
- MRI and CT to exclude thrombosis;
- after adulthood, a spermogram is performed - pathology shows asthenozoospermia or oligospermia, a decrease in activity or quantity, respectively.
Additional diagnostic methods:
- Ultrasound of the scrotum,
- dopplerography,
- thermography and thermometry,
- rheography.
To construct a treatment regimen for varicicolitis in men, retrograde venography of the kidneys and testicles, transscrotal testicular phlebography and antegrade venography are performed.
The multidisciplinary medical clinic (academician Roitberg’s clinic) offers modern, accurate and fast research methods.
Symptoms of varicocele: the disease may be asymptomatic
In 85-88% of cases, varicose veins affect the left testicle along the blood flow. Bilateral involvement is rare, occurring in approximately 5% of diagnoses.
There are several possible options for the development of varicocele:
- Asymptomatic.
- Mild symptoms. In young men, there is a noticeable slight increase in the left half of the scrotum. It may be slightly lowered.
- Noticeable symptoms. Nagging pain in the testicles that appears or intensifies with walking, excitement, lifting heavy objects and other stress.
- Objective symptoms. A clear pattern of the veins of the testicles, their convolution. With advanced varicose veins, there is a noticeable decrease in the volume of the affected area associated with atrophy.
If you look at the affected testicle through the eyes of a urologist, a varicocele looks like this:
- weakening of veins;
- compression of veins;
- increased pressure in the veins of the testicles;
- disruption of blood flow.
Poor circulation affects the entire organ: the veins and small capillaries of the scrotum area are affected.
With a bright degree of varicocele, you can visually notice thickening, plexus and protrusion of veins. It's not pretty, but it's not scary either. Another complication of testicular varicose veins is much more dangerous - infertility caused by deterioration of spermatogenesis. Urologists often note a connection between varicocele and infertility, so they recommend treating the disease.
Preventive measures
An annual visit to the urologist, even in the absence of any complaints or symptoms, in combination with a healthy lifestyle, decisive and unconditional cessation of bad habits (primarily smoking) and active sports is the best set of preventive measures at any age. You should also pay attention to the functioning of the gastrointestinal tract, and take care to exclude fatty, fried and spicy foods from your diet. Clothing should be comfortable and not constrict the genitals. It is important to remember that hypothermia of the body is an additional provoking factor for the occurrence of varicocele or its progression.
Stages of development of testicular varicose veins
Varicocele begins with a mild form and gradually progresses. At the same time, the pathology does not always reach its climax; varicose veins can stop developing, remaining undetected.
The disease occurs in 4 stages:
- Symptoms of varicocele are hidden.
The veins of the testicle are not visible or palpable. Dilatation of the veins is detected on ultrasound of the scrotum. That is why preventive ultrasound examination is recommended for all young men at the age of 17-18 years. - The veins are palpated in a horizontal position.
In the supine position no changes are noticeable. - Veins can be palpated in any position.
- Dilated veins are greatly enlarged and visible
. If severely disturbed, they may even hang down. Pain appears.
Spermagenesis is disrupted gradually, which leads to infertility. The brighter the signs, the more reasons to suspect a male factor in infertility.
Complications
The most important complication of varicose veins in the spermatic cord is infertility. It occurs against the background of impaired thermoregulation of the testicles, which leads to the cessation of sperm production.
Other dangerous consequences of varicicole are:
- heart valve malfunction;
- phimosis or flat feet.
When to see a doctor
Often varicose veins are one of the signs of the presence of malignant tumors. That is why it is not recommended to postpone visiting a doctor for a preventive examination when symptoms of the disease appear.
The slightest signs of pathology of the veins of the spermatic cord should be a reason for an unscheduled visit to the doctor. It is recommended to visit a urologist or phlebologist for varicicol.
JSC “Medicine” (academician Roitberg’s clinic) employs doctors from 66 specialties, trained at the highest level. You can make an appointment and choose a doctor on the website, by phone or from the administrators at the clinic at the address: Moscow, 2nd Tverskoy-Yamskaya Lane, 10, in the immediate vicinity are the Novoslobodskaya, Belorusskaya, Chekhovskaya, Tverskaya metro stations.
Male infertility and varicocele
Varicose veins of the testicles affect sexual function from several sides at once, so infertility can occur very quickly.
Varicocele reduces fertility due to the following factors:
- Increased testicular temperature
. Testicular temperature in healthy men is lower than body temperature. With varicose veins, the flow and flow of blood through the veins is disrupted. As a result, thermoregulation changes - the testicles heat up, which leads to a deterioration in the properties of sperm. Sperm motility and quantity decrease. - Compression of the testicles
. Enlarged veins compress the testicles, reducing spermatogenesis. Tissues atrophy. - Antibody production
. With varicocele, the immune system may begin to work erroneously, perceiving testicular tissue as foreign. The result of this is autoimmune inflammation of the scrotal organs and infertility. - Testicular hypoxia
. This is a syndrome of oxygen starvation, leading to tissue death. - Oxidation
. Due to impaired blood flow, free radicals accumulate in the tissues of the scrotum, causing tissue aging and cell death. - Throwing of biologically active substances
produced for the kidneys back from the adrenal glands into the testicles.
Urologists have proven the effect of testicular varicose veins on infertility in men, so the disease should be treated without waiting for problems.
However, there is no need to panic - the connection between testicular varicose veins and infertility
not always found:
- varicocele accompanies male infertility in 40%;
- in men with varicose veins, a deterioration in the quality and quantity of sperm is observed in 60% of cases.
Only a urologist can establish a connection between testicular varicose veins and decreased fertility. In any case, the pathology must be treated.
Advantages of Marmara microsurgery:
- A small cosmetic incision in the groin area, in the hair growth area (the scar is almost invisible)
- The greatest efficiency of the operation is achieved through the use of operating binoculars and microsurgical instruments
- Lowest percentage of relapses and complications (less than 5 percent)
- Can be performed on an outpatient basis, without hospitalization
- Short and easy postoperative and recovery period
I am aware of my responsibility for preserving the main thing that my patient trusts me, and I will do everything to justify the trust!
How is varicocele treated?
Varicose veins of the testicles cannot be cured with pills, folk methods or wearing various devices. In most cases, surgery is necessary; sometimes the doctor limits himself to monitoring the man’s condition.
The indications and methods of treatment for testicular varicose veins are determined by the surgeon. A direct indication for surgery will be a set of symptoms:
- male infertility associated with varicocele;
- poor sperm count;
- cessation of testicular growth;
- testicular pain;
- aesthetic unattractiveness - knotty, protruding veins.
It is believed that to prevent infertility, surgery should be performed on all young men with varicose veins. In young men, intervention is necessary when reducing the size of the affected testicle. If a man has children and varicose veins do not bother him, you can postpone the operation and see a urologist.
The operation can be performed using different methods:
- Percutaneous embolization.
X-rays are used to occlude the affected vein without making any incisions. The method is considered risky, since x-rays are dangerous in themselves. - Classic operation
. The urologist makes an incision in the skin, reaching the testicular vein. The affected vein is ligated in two places and excised. The reverse flow of blood through this vein stops and the load is redistributed to healthy vessels. - Microsurgical ligation.
The microequipment necessary to occlude the affected vein is used. The operation is possible if the spermatic cord is well visualized. - Laparoscopic surgery.
The intervention is carried out using a modern laparoscope - a device equipped with micro-instruments and a video camera.
The effectiveness of the operation is high: urologists eliminate more than 90% of cases of varicocele. But varicose veins can recur even after intervention. Therefore, after treatment for testicular varicocele, you need to be constantly monitored by a urologist and follow all postoperative recommendations of doctors.
Treatment at the Innovative Vascular Center
The Innovative Vascular Center uses endovascular technology to eliminate varicoceles. We perform retrograde venography of the testicular vein and embolize this dilated vein with special coils and sclerosants. This operation for varicocele does not require incisions or hospitalization for treatment, but reliably eliminates venous hypertension in the left testicle.
Early diagnosis and treatment are important for the outcome of these patients. The need for timely intervention is indicated by the fact that among patients operated on before the age of 21, the risk of infertility is minimal, and before the age of 30, the probability of childlessness increases 4 times! The earlier surgery is performed for varicocele in men, the greater the likelihood of avoiding complications. This is all the more important because modern technologies are highly effective and completely painless and have low prices.
Traditional methods
Many people ask the question of how to cure varicocele at home, so the following set of measures has already become traditional:
- tinctures and decoctions for oral use;
- compresses for external use;
- medicinal baths;
- massage;
- aromatherapy;
- physiotherapy.
You can choose 3-4 suitable methods. The main thing is that there is a regular and comprehensive impact on the problem.
Herbs that help get rid of varicocele:
- horse chestnut;
- yarrow;
- Oak bark;
- St. John's wort;
- calendula.
These plants have analgesic, venotonic and anticoagulant effects.
It is also worth remembering herbs that are strictly contraindicated for varicocele:
- valerian;
- motherwort;
- hawthorn.
Home treatment can be carried out for unilateral varicocele. The bilateral process is usually abrupt and complicated. In this case, urgent surgery is required.
Tinctures and decoctions
Infusions, tinctures and decoctions are widely used as folk remedies for testicular varicocele. The most popular of them.
Chestnut flower tincture
Pour 100 grams of chestnut flowers into a bottle of vodka. Infuse for two weeks in a cool place. Take ten drops three times a day. Contraindication: kidney disease.
Oak bark decoction
Pour 100 grams of dry oak bark extract into a liter of water and boil. After this, simmer in a water bath. Then strain the mixture and take it, diluting 50 ml of decoction in 200 ml of water. Use in courses of one month. This is one of the most effective remedies for the treatment of varicocele.
Infusion of a mixture of herbs for varicocele
Pour 1 teaspoon of yarrow, chamomile flowers, chestnut, string, raspberry leaves, dried wort, St. John's wort into a liter of boiling water. Infuse for one day. Take 150 g twice a day for three weeks in a row.
Compresses and lotions
Applying compresses for testicular varicocele is a more complicated procedure than taking a decoction, but the effect is worth the effort.
Compresses and lotions help:
- relieve pain
- improve blood circulation;
- reduce swelling.
It is important to do the compress correctly - apply gauze soaked in the medicine, then a plastic bag or cling film. Cotton wool is placed on top and everything is bandaged with a bandage.
Common and effective compress recipes for the treatment of varicocele.
Oatmeal compress
Mix one tablespoon each of strawberry leaves, birch leaves, dandelion roots, sweet clover, and chopped oat straw. Take a tablespoon of the resulting mixture and pour 600 ml of boiling water. Leave for half an hour. The compress is made daily before bedtime according to the above scheme for three weeks.
Alcohol compress on acacia flowers
5 tbsp. l. acacia flowers pour 100 ml of vodka. Leave for 2 weeks in a cool, dark place. The recommended frequency of use of this compress is 3 times a week. Apply a compress before going to bed.
Oil lotion with St. John's wort
Pour one tablespoon of St. John's wort into 100 ml of vegetable oil. Simmer in a water bath for three hours. Make lotions with the resulting mixture four times a day. The product gives good results in a relatively short period of time.
Therapeutic baths
Hot baths for vein pathology are contraindicated. Therefore, we will talk about sitz baths only for the genitals. A deep basin is suitable for these purposes.
You can consider the following herbal bath recipes for varicocele.
- From a decoction of calendula. Pour boiling water (1 liter) over a handful of dry calendula and leave in a warm place for 2 hours. Strain and mix in a bowl of cold water. Take this bath for 15 minutes.
- From angelica. Pour 100 g of herb into a liter of boiling water. Leave for 14 hours. Pour into a bowl, dilute with cool water. The procedure time is 30 minutes.
- With oak leaves, wormwood, calendula and chamomile. Take the herbs in equal proportions, pour boiling water over them and let it brew. Then dilute with cold water. Bath duration is 20 minutes.
If you have varicocele, you should avoid saunas, steam baths and hot baths. The temperature of the therapeutic baths is not higher than 40°C.
Complementary therapy
Treating varicocele with compresses and decoctions alone is not enough. It is best to combine it with exercise, massage and wearing compression garments.
Physiotherapy
Exercises that improve pelvic circulation and make blood vessels more elastic will help. These include:
- alternate walking on toes and heels;
- bending forward;
- swing your legs;
- rotation of the pelvis.
Before performing the exercises, you should warm up. Each of them needs to be repeated 10-15 times. It is advisable to perform gymnastics 2-3 times a day.
Massage
After therapeutic exercises, it is recommended to massage the testicles. You can perform either self-massage or contact a massage therapist.
The specifics of self-massage are as follows: lying in a comfortable position, you need to rub the testicles with light circular movements, gradually increasing the pressure. Movements should be clockwise. Duration of massage for varicocele – up to 10 minutes
The procedure should not be painful. You should immediately stop manipulation if there is pain or discomfort.
Aromatherapy
A relaxing procedure with an aroma lamp has a good effect on the healing process. Suitable natural essential oils:
- mint;
- lemon balm;
- lemongrass;
- sandalwood;
- tea tree.
You can choose from this list what you like best or create your own aromatic composition. This will not reduce the therapeutic effect.
Rules for the procedure:
- light the aroma lamp and drop 5-7 drops of the selected oil into it;
- dim the lights;
- turn on relaxing music;
- relax, lying on your back.
20 minutes for such a procedure will be enough. Can be done every other day.