Varicocele is a common urological disease in which a man experiences dilatation of the veins of the pampiniform plexus of the spermatic cord of the testicle. As a rule, the pathology occurs in men who have a predisposition to varicose veins. The weakness of the venous wall is genetically determined, so patients with varicocele very often have concomitant venous diseases - varicose veins and hemorrhoids.
Dilation of the veins of the testicle interferes with the normal outflow of blood, which can result in complete atrophy of the testicle over time. In many men with varicocele, due to impaired spermatogenesis, the spermogram has deviations, from minimal abnormalities to the complete absence of living, motile sperm suitable for fertilization. Therefore, treatment of varicocele is important in the prevention of male infertility.
Varicocele cannot be treated conservatively; the man requires surgery.
There are several options for the operation:
- Ivanissevich operation - through inguinal access;
- Marmara operation - through an infrainguinal incision;
- retroperitoneal access;
- laparoscopic clipping;
- transvenous embolization.
Varicocele causes
Varicocele does not cause pain, and only occasionally can be manifested by aching or pulling sensations in the testicle . This is the insidiousness of this disease, because it can be difficult to convince a patient who is not in pain to go under a knife (although today it is, of course, not a knife, but a microsurgical instrument ). But it is necessary to undergo surgery, because due to varicose veins of the spermatic cord, blood stagnation occurs in the testicle , its blood supply suffers and the local temperature rises. All these factors, acting gradually and imperceptibly, lead to disruption of the process of formation and maturation of sperm, and in advanced cases - to a decrease in the size and atrophy of the testicle . The sooner varicocele , the greater the chance of preventing negative consequences for the man’s body.
In patients with varicocele, pathological changes in the spermogram are often detected. The most common are oligozoospermia (a decrease in the concentration of sperm to less than 15 million per ml), asthenozoospermia (a decrease in the concentration of progressively motile sperm to 32% or less), teratozoospermia (a large number of pathological forms of sperm, exceeding 96%). Varicocele is characterized by damage and fragmentation of sperm DNA .
Several studies in recent years have confirmed the relationship between varicocele and decreased testosterone levels and erectile dysfunction . Thus, in 2011, a group of Indian scientists led by Sathya Srini V. published the results of treatment of 200 patients with hypogonadism and erectile dysfunction in combination with varicocele. Some of these patients received hormone replacement therapy, while others underwent surgical treatment of varicocele. In 78% of patients who underwent surgery to eliminate varicocele, normalization of testosterone levels was achieved with improvement in erectile function. Similar results were demonstrated by the Polish urologist D. Paduch. In his study of infertile men with varicocele and hypogonadism, 76% achieved normalization of testosterone and improvement in sexual function after surgical treatment of varicocele.
Degrees of varicocele
Varicocele grades (according to the criteria of the European Association of Urology):
| STAGE | CHARACTERISTIC |
| Subclinical varicocele (0) | non-palpable (even with the Valsalva maneuver) dilation of veins, determined only using Doppler ultrasound |
| First stage varicocele | expansion palpable during the Valsalva maneuver, disappearing with rest |
| Second stage varicocele | expansion palpable at rest and during the Valsalva maneuver, but not visually detectable |
| Third stage varicocele | visually detectable dilatation, determined both at rest and during the Valsalva maneuver |
The second and third stages may be accompanied by a decrease in size (hypotrophy) of the corresponding testicle.
TREATMENT OF VARICOCELE
Varicocele surgery
Varicocele in men treatment
As I already mentioned, conservative methods of treating varicocele are ineffective . A weak and stretched vein wall cannot be strengthened with medications. Therefore, the only effective treatment for varicocele is surgery. There are various options for operations for varicocele . Dilated veins can be ligated in the inguinal canal, above or below it. An endovascular approach is possible - embolization and sclerosis of dilated veins. However, the “gold standard” is microsurgical infrainguinal (subinguinal) ligation - the Marmara operation. Let's consider the features of each of these operations used to treat varicocele .
Indications
Treatment of varicocele using the Ivanissevich method is indicated for people of all ages at any degree of development of the disease. As a rule, the intervention is performed under local anesthesia, but for younger patients it is possible to use general anesthesia.
It is important to know. The essence of any surgical treatment for varicose veins is to stop blood circulation through varicose vessels, after which blood flows through healthy veins.
If the disease is not treated, there is a risk of developing infertility
How to treat varicocele
Operation Palomo
In this operation, a 5-6 cm long incision is made in the lower lateral part of the abdomen, above the inguinal canal. In this place, the testicular vein is usually a single trunk, running along with the testicular artery and lymphatic vessels. The surgeon isolates, ligates and cuts the vascular bundle as a single block. General or spinal anesthesia is most often used. The disadvantage of the Palomo operation is the intersection of the testicular artery that supplies the corresponding testicle, which can worsen its functional state. The intersection of lymphatic vessels can lead to the formation of hydrocele (hydrocele). Recovery and rehabilitation after Palomo surgery takes about 2 weeks.
Operation Ivanissevich
The length of the incision is approximately the same as during the Palomo operation, but the incision itself is made lower, directly in the area of the inguinal canal. The spermatic cord (containing dilated veins) lies quite superficially in this place, which makes it possible to isolate it. Typically, the operation is performed under general or spinal anesthesia, although local anesthesia is also possible.
During the Ivanissevich operation, the surgeon tries to preserve the testicular artery and lymphatic vessels, but the lack of optical magnification makes this task difficult. In case of ligation of the artery and lymphatic vessels, the complications described above may occur (testicular atrophy, hydrocele formation). The recovery period after Ivanissevich's surgery lasts about 2 weeks .
Operation Marmara
Marmara operation (subinguinal microsurgical ligation of the veins of the spermatic cord). This technique was first described by American urologist Joel Marmar in 1985. Through a small (about 2 cm) skin incision in the groin area (below the inguinal canal), the spermatic cord is isolated. Using optical magnification (operating microscope or binoculars) and microsurgical techniques, the elements of the spermatic cord (vas deferens, testicular artery, tributaries of the internal spermatic vein and lymphatic vessels) are separated. Venous vessels with a diameter of more than 2 mm are ligated (ligated) and divided. All other elements remain intact. The operation ends with the application of a cosmetic suture.
In 1992, another American urologist-andrologist Mark Goldstein modified the Marmara operation, proposing to cross not only the branches of the internal spermatic vein, but also the veins of the scrotum (branches of the external spermatic vein and gubernacular veins), for which it is necessary to remove the testicle into the surgical wound. The Goldstein modification is still actively used by urologists around the world, especially for recurrent forms of varicocele.
The Marmara operation can be performed under general or spinal or local anesthesia. The minimal incision length and microsurgical technique make it possible to perform this operation on an outpatient basis, without hospitalization.
In most cases, the patient can leave the clinic within 1-2 hours after surgery. Complications during the Marmara operation are much less common than with other types of operations used for varicocele. The functional and cosmetic results of Marmara surgery are also significantly better than other techniques. The number and motility of sperm increases to a greater extent. It is natural that the Marmara operation is currently considered as the “gold standard” for the surgical treatment of varicocele.
Scrotal access
Varicose testicular veins can also be divided at the level of the scrotum. Through a small incision of about 1-2 cm, the spermatic cord is isolated, followed by the intersection of varicose veins. The main stages of the operation correspond to the Marmara technique . The main difficulty with scrotal access is that the internal spermatic vein at the level of the scrotum is represented by a network of veins of different sizes, forming a pampiniform (or pampiniform) venous plexus. To achieve a good effect, it is necessary to cross each of these branches, which, of course, increases the operation time. The scrotal approach is currently rarely used for the treatment of varicocele.
Laparoscopic ligation of the testicular vein
Like any other laparoscopic surgery, ligation of the testicular vein is performed through punctures in the anterior abdominal wall. The operation is performed only under general anesthesia. Instruments and an optical system are introduced through punctures into the abdominal cavity. The testicular vein is isolated near the internal opening of the inguinal canal, metal clips are applied to it, and the vein is divided. The functional results of laparoscopic surgery for varicocele are generally close to the results of the Ivanissevich operation.
The postoperative period is easier than during the operations of Palomo and Ivanissevich , punctures in the abdomen heal quite quickly. Typically, the patient is discharged home the next day after laparoscopic ligation. The only advantage of laparoscopic surgery for varicocele, in my opinion, is the ability to cross the testicular veins on both sides (for bilateral varicocele) through the same access. The disadvantages of the laparoscopic approach are the need for general anesthesia, as well as the risk of complications associated with the introduction of instruments into the abdominal cavity.
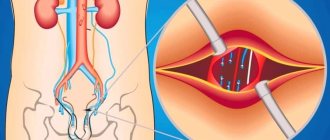
Testicular vein embolization for varicocele
This technique is the least invasive among all those used to treat varicocele . The absence of an incision allows embolization to be performed under local anesthesia (or without anesthesia at all!). Naturally, there is no need for seams. A thin catheter with a flexible guide is inserted through a needle into the femoral vein. Contrast is injected through the catheter into the vasculature, and the location and movement of the guidewire and catheter are monitored using fluoroscopy. The catheter is passed retrogradely (from the renal vein towards the testicle) into the internal spermatic (testicular) vein. The structure and features of the testicular vein are assessed, and possible additional branches and tributaries are identified. After this, a coiled spiral is inserted through the catheter into the lumen of the vein. In the lumen of the vein, the spiral expands, firmly pressing against the walls of the vein and fixing itself inside. Then an embolic substance is injected into the lumen of the vein, completely closing the lumen of the vein. A control study of blood flow through the vein is performed. If there is no blood flow, the operation is completed.
The patient can leave the clinic within two hours after the operation . Recurrence of varicocele after embolization is very rare. Another advantage of embolization for varicocele is that during the procedure, fluoroscopy of the veins is performed, which makes it possible to diagnose various anatomical anomalies, additional branches connecting the testicular vein with the vein of the same name on the opposite side, and other vascular features leading to relapses of varicocele. In this regard, embolization may be particularly effective in cases of recurrent varicocele. Like any method, testicular vein embolization is not without its drawbacks.
One of the significant ones is the need to administer a contrast agent (usually the same as is administered during computed tomography). Some people have an allergic reaction to contrast and cannot undergo embolization. In addition, the administration of contrast is contraindicated in renal failure. Therefore, before this operation, the blood creatinine level must be checked.
Another limitation for embolization is right-sided varicocele. Right-sided localization is uncommon with varicocele. But, due to anatomical features, inserting a catheter and guide into the right testicular vein is often very difficult. Therefore, for right-sided (or bilateral) varicocele, it is better to resort to surgical treatment methods rather than embolization.
The high cost and relatively low availability of embolization are also of particular importance. The cost of embolization for varicocele, as a rule, is several times higher than the cost of surgical treatment (including the Marmara operation). This is due to the use of expensive disposable consumables and the need to work in an endovascular operating room equipped with high-resolution fluoroscopic equipment (angiograph). Embolization is a highly operator-dependent technique, the effectiveness and safety of which largely depends on the surgeon (human factors).
Complications from testicular vein embolization are rare . These include an allergic reaction to contrast, impaired renal function, bleeding from the puncture site, and perforation of the vein wall. A rare specific complication is migration (displacement) of the installed coil and its movement along the vascular bed with the occurrence of embolism in various organs.
Comparison of different operations for the treatment of varicocele :
| Cut length | Anesthesia | Rehabilitation period | Relapse rate | |
| Operation Palomo | 5-6 cm | spinal | 2 weeks | 29 % |
| Operation Ivanissevich | 5-6 cm | spinal | 2 weeks | 13,3 % |
| Operation Marmara | 2 cm | local/general | 7-10 days | up to 4% |
| Laparoscopy | 3 punctures | anesthesia | 5-7 days | 3-7 % |
| Embolization | No incision | local | 1 day | to 10 % |
, in accordance with the recommendations of the European Association of Urology , I perform on my patients the most modern operation for varicocele - microsurgical subinguinal ligation of varicose veins according to Marmar, and I have extensive experience in this operation.
Treatment of varicocele without surgery
Many of my patients, who are faced with such a problem as varicocele for the first time, are primarily interested in whether it is possible to treat varicocele without surgery. Of course, it would be very tempting to do without surgery, or even better to cure varicocele with folk remedies. Unfortunately, I have to disappoint them. There are currently no effective methods for treating varicocele without surgery. A temporary positive effect can be provided by some herbal remedies that increase the tone of the veins (horse chestnut tincture, grape leaves), as well as medications (for example, Aescusan, Detralex, Phlebodia, etc.). Varicoceles, of course, will not go away with these medications, but the symptoms may decrease. To reduce the symptoms of varicocele, adherents of traditional medicine recommend limiting physical activity and wearing tight-fitting underwear (so that the scrotum does not sag, but is pressed against the perineum). Temporary relief can be expected from these measures, but the varicocele itself will not disappear. Therefore, I must state that attempts to cure varicocele without surgery only waste precious time.
Treatment of varicocele - operations
As I already mentioned, conservative methods of treating varicocele are ineffective.
Positive and negative aspects of this technique
For a long time, Ivanissevich’s operation remained practically no alternative for the removal of varicocele (not counting identical techniques, for example, Palomo), but in modern practice new, less traumatic methods of treatment have appeared using micro-access, magnifying imaging equipment, a computer and other innovations.
These operations are becoming increasingly popular, and classical abdominal interventions are gradually becoming a thing of the past. However, the simplicity and accessibility of surgery according to Ivanissevich keeps this method in the top of frequently used ones.
For the sake of objectivity, we will indicate the positive and negative aspects of such therapy, starting with the positive ones:
- The lowest price;
- A regular operating room is suitable for the intervention; there is no need for special equipment;
- The technique does not require special specialized training (unlike laparoscopy or sclerotherapy);
- Suitable for removing varicocele of any degree and regardless of the patient’s age.
However, the negative aspects significantly outweigh, which forces progressive clinics to abandon the use of this technique and switch to more effective methods for eliminating varicocele.
Among the main negative characteristics we highlight the following:
- Highly traumatic;
- Significant likelihood of developing postoperative complications or relapse (30-40%);
- Treatment requires hospitalization from 8 to 14 days, depending on the individual characteristics of the patient;
- Sutures are removed on the 8th day;
- Long rehabilitation period. Full recovery is possible no earlier than six months;
- Severe pain syndrome;
- The operation leaves a large scar (similar to an appendicitis scar).
The procedure is quite painful
Advantages of Marmara microsurgery:
- A small cosmetic incision in the groin area, in the hair growth area (the scar is almost invisible)
- The greatest efficiency of the operation is achieved through the use of operating binoculars and microsurgical instruments
- Lowest percentage of relapses and complications (less than 5 percent)
- Can be performed on an outpatient basis, without hospitalization
- Short and easy postoperative and recovery period
I am aware of my responsibility for preserving the main thing that my patient trusts me, and I will do everything to justify the trust!
Postoperative complications
As already mentioned, this technique has a high probability of developing relapses and complications. According to statistics, out of ten men who underwent surgery, at least three will encounter postoperative consequences of a different nature, and the likelihood of a relapse is estimated to be significantly higher (30-40%) than the manifestation of other postoperative complications.
Recurrence of varicocele
The occurrence of relapse is explained by the fact that the surgeon is not able to examine the entire vein because only a small section of it is accessible to him. At the same time, possible branches of the vessels, also affected by varicose veins and located outside the incision, remain invisible.
Under such circumstances, it is impossible to talk about a relapse, as such, in its pure understanding, but it would be more accurate to call it technical shortcomings or limited technical capabilities during surgery. There is another option when the veins remain unligated or, more precisely, only part of them is ligated, which occurs with the so-called loose varicocele.
The surgeon may not notice inflammation of the veins, since in a supine position some of them will be in a dormant state, especially if the lesion is not severe, and the doctor naturally does not have the opportunity to see them. Such vessels remain unligated.
After treatment, blood begins to circulate through them somewhat more intensely than before, and the re-development of varicocele occurs.
Complications
Complications do not refer to relapses, although often many do not share these concepts. When the integrity of nearby tissues is damaged, complications arise that are caused precisely by the surgical intervention and have nothing to do with the original disease.
When operating using the Ivanissevich method, complications are not frequent, but the following are still possible:
- hematomas and bleeding;
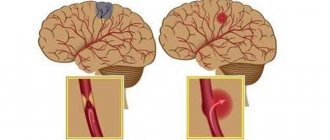
- dropsy of the testicle (hydrocele);
- disruption of the innervation of certain areas;
- secondary infection.
The mechanisms of occurrence of the first three complications have already been described above. The introduction of infection is explained by a violation of antisepsis both during surgery and when changing sterile dressings during dressings.
Schematic representation of a hydrocele