Heart transplant - indications
Diseases that are indications for transplantation:
- cardiomyopathy - replacement of myocardial fibers with scar tissue;
- inoperable heart defects of congenital and acquired nature;
- tumor processes in the area of the heart muscle;
- angina pectoris and heart rhythm disturbances that cannot be corrected with medication;
- congenital disorders of the development of the heart muscle that are not subject to plastic correction;
- end-stage heart failure.
Heart transplantation is indicated in extreme cases. When all other options for correcting the patient’s condition have already been tried and have not given the desired result.
4 Consequences of the operation
The early postoperative period is the most difficult in terms of adaptation of the new organ to the changed operating conditions. If the outcome of the operation is positive and there are no serious complications, normal heart function returns in about 3-5 days. It is during this period that complications such as:
- donor heart rejection;
- thrombosis of the heart arteries;
- dysfunction of the brain;
- disruption of the lungs, liver, kidneys and other organs.
In the next 7-10 days, complications such as:
- infectious infection;
- coronary artery disease;
- internal bleeding;
- pneumonia;
- arrhythmia;
- development of oncological tumors against the background of immunosuppressive drugs in the preoperative period.
All these consequences can appear in different orders and at different time intervals after the operation. Complications after transplantation occur in more than 90% of cases, most often arrhythmia, coronary artery disease and internal bleeding. Any complications, to one degree or another, can cause the patient’s death.
World experience and prices
As practice shows, a transplanted heart, if all medical recommendations are followed, can work without interruption for 5-7 years. However, the aging process in the donor organ proceeds faster than in its own, and therefore sooner or later the patient will note the return of all symptoms of heart failure.
The actual practice of heart transplantation differs significantly from country to country. In some countries, these operations are not carried out at all because they are not regulated at the legislative level. In other countries, such operations are clearly regulated and both residents of the country itself and foreign citizens can resort to it. For example, in the Republic of Belarus, organ transplantation is carried out in accordance with the law, which is based on the “presumption of consent”: organ collection from a donor can be carried out after declaring brain death, unless wishes to the contrary are expressed by the patient before death. The organ can be used for further patients in need.
SELECT A FREE CLINIC FOR HEART TRANSPLANTATION
What may interfere with the operation?
Unfortunately, not every patient will be able to receive a donor heart. There are many different reasons for this:
- Very small number of donors. This can only happen to a person who has registered brain death and whose heart is absolutely healthy.
- There is a very long queue to receive this organ (waiting list), this is most important for children. The organ must fully comply with all the stated requirements and, perhaps, several dozen more patients who are much earlier on the list will have such parameters.
- Sometimes the donor organ cannot be delivered to the right place on time, since the operation must be performed no later than six hours after removal.
- Many people do not agree to undergo a transplant due to ethical or religious reasons. For example, in Christianity a person is alive as long as his heart beats.
- The patient can be stopped by the fear of long and rather expensive rehabilitation.
- Advanced age. Typically, operations are not performed on people over 60 years of age, but there are exceptions.
In addition to the listed obstacles, transplantation will not be performed for a number of other diseases not related to cardiology. It can be:
- pulmonary hypertension in severe form;
- diabetes mellitus at a stage in which negative changes in the retina, blood vessels or kidneys have already begun;
- infectious diseases in the acute stage;
- HIV and tuberculosis;
- autoimmune diseases - rheumatism, arthritis, lupus erythematosus, etc.;
- severe liver or kidney failure;
- chronic severe forms of lung disease;
- oncology;
- addiction to alcohol or drugs;
- severe mental disorders.
What does preparation for cardiac transplantation include?
Before a heart transplant, the recipient should undergo the following examinations:
- general clinical analysis of blood and urine;
- biochemical screening, coagulogram;
- blood test for group and Rh factor;
- tissue typing;
- examination for hepatitis B and C, Epstein-Barr virus, cytomegalovirus, herpes simplex virus;
- tuberculin skin test;
- serological tests for fungi;
- prostate-specific antigen test for men, mammography and cervical smear for women;
- thyroid hormones;
- pulmonary artery pressure measurement;
- ultrasound scanning of the heart, daily ECG monitoring;
- chest x-ray;
- spirometry;
- myocardial biopsy - according to indications.
The heart donor must meet the following criteria:
- recorded brain death;
- age under 65 years;
- ejection fraction according to ultrasound results - more than 50%;
- absence of ischemic disease and other myocardial pathologies.
The selection of a donor-recipient pair when planning a transplantation is carried out according to the blood type and size of the transplanted organ.
How much does a heart transplant cost?
All citizens of the Russian Federation have the right to free high-tech medical care, which includes transplant operations. Based on this, if a suitable heart is available, it will not cost the patient anything. But, in addition to the heart transplant operation, the patient will face long and expensive rehabilitation. This period may drag on and require the recipient to pay at least 50 thousand dollars. For children, such a transplant will cost much more, since both the selection of a donor and the operation itself will have to be performed in a foreign clinic.
ROSTOV REGIONAL CLINICAL HOSPITAL
From the editor. It has been written more than once that the Regional Clinical Hospital has had a transplantology program for three years. The implementation of the program and 68 operations performed, with low mortality, 40 operations planned for 2018 - this is a huge amount of work and huge risks, this is the responsibility of the Minister of Health of the Republic of Uzbekistan T.Yu. Bykovskaya and the head physician of the Regional Clinical Clinical Hospital V.L. Box, this is the decision of Governor V.Yu. Golubeva to continue funding the program. But we won’t talk about all this and “to whom we thank” today. Let's talk about what lies behind all this - factually and emotionally. So to speak, the very top cut.
Heart transplant is not the most difficult operation in transplantology
The most difficult one is transplanting the right lobe of a related liver. It was this kind of operation that was successfully performed for the first time in the history of Rostov transplantology. And then there were several more...
Vyacheslav Leonidovich Korobka, chief physician of the Rostov Regional Clinical Hospital (40 organ transplant operations):
– Transplantation of the right lobe of a related liver for quite a long time in the world practice of transplantology was the most difficult and the most risky. It remains the most difficult to this day. It is much easier to perform a whole liver transplant operation. To put it briefly and primitively, so that everyone understands: this is due to a certain structure of the organ and the fact that when transplanting the right lobe of the liver, it is necessary to sew together many more vessels, their diameter is smaller, technically it is more difficult; There are other significant nuances. The donor, a relative who donates a share of the liver, is also at quite a high risk; For him, the operation is fraught with bleeding and a number of complications.
Many surgeons around the world tried to develop their own technologies for this operation and improve them. Did not work. The optimal technology, which the whole world uses today, was developed by the Russian surgeon Sergei Vladimirovich Gauthier. He could not help but understand that he had made a breakthrough in transplantation, but he did not make any fuss about it. I just made a report at one of the international conferences, confirming it with already accumulated material. The report created a sensation. On that day, the name S.V. Gauthier went down in the history of world transplantology.
When S.V. Gauthier’s anniversary happened; many of the best surgeons in the world flew to Moscow to congratulate him (without any invitations).
The second heart transplant operation in our Republican Clinical Hospital was performed (and, I hope, many more will be performed) by Mikhail Yuryevich Kostrykin, deputy. Chief physician for surgery, cardiovascular surgeon. How did he go about this? How did we all go to transplant surgeries? Over the past, probably, two years, Mikhail Yuryevich has had many business trips - to the best clinics in Russia and abroad. This is serious study. He studied the technology of heart transplant operations, stood behind the surgeon, assisted, participated in the pre- and postoperative analysis of the patient’s condition, and discussed the progress of the operation.
Not every world-class surgeon is ready to share his secrets with everyone who comes to study or train with him; We have established friendly relations with the best specialists in Russia, and this probably indicates that they appreciated our professional, human, and personal qualities. Kirill Olegovich Barbuhatti, who today is one of the best surgeons in the country, provided great assistance. (K.O. Barbuhatti – Head of Cardiac Surgery Department No. 2 of the Krasnodar Regional Clinical Hospital No. 1 named after Prof. Ochapovsky - editor’s note). Mikhail Yuryevich has been to this clinic many times to watch heart transplant operations.
The first heart transplant operation in our hospital was performed by K.O. Barbuhatti; This is how it is accepted: the first operation is always performed in all medical institutions by a recognized specialist; why take the risk? We were all in the operating room, of course; Mikhail Yuryevich assisted; everyone understood: the second heart transplant and subsequent ones would be performed by Kostrykin. He did it no less successfully.
Of course, all this happened thanks to the many years of work of Prof. A.A. Dyuzhikov, under whose leadership the team of the cardiocenter of the Rostov Regional Clinical Hospital, the Rostov School of Cardiac Surgery and close contacts with many clinics in our country were formed.”
Mikhail Yurievich Kostrykin, Deputy Chief Physician of the Regional Clinical Clinical Hospital for Surgery (28 organ transplant operations):
– As initially expected, we carried out the second operation on our own; no one stood behind him to belay. Of course, everyone was preparing. But before the operation, and even before going to the operating room, we repeatedly called Kirill Olegovich, discussed the patient, possible options and nuances, and consulted. In general, it is wrong to refuse someone’s advice and help if there is such an opportunity. Both operations went smoothly. The patients were discharged in December, before the New Year, both feel well and themselves assess how dramatically their well-being has changed. The patients are quite young people: one is 33 years old, the other is 39 years old, both have families, children, and their whole lives ahead. If not for these operations, their chances of surviving more than a year were extremely low. There was no alternative to surgery. Today we believe that their biggest problems are behind them.
Of course, both these patients and others who have undergone organ transplantation are under our constant supervision; they regularly appear with us for routine control laboratory tests. They undergo immunosuppressive therapy to suppress and prevent rejection reactions of the transplanted organ. They will have to take these drugs for the rest of their lives, but over time the dosage regimen changes downward. Patients have 24-hour contact with us - they also contact us regarding medical problems that are completely unrelated to the operation performed; It's better to play it safe.
– What kind of nerves do you need to have? I look at Vyacheslav Leonidovich - he is a very calm person, I look at you - you are also calm, you both speak quietly and measuredly; I understand, maybe you’re forcing yourself to be like this, because if you let yourself go, you might even end up shaking...
– The main stage of a heart transplant operation lasts from 1.5 to 3 hours; in total, taking into account the preparatory and final stages, about 5-6 hours. It is very important that this is a team effort. When performing a heart transplant, there is always a fairly strict time limit, and in order to save it, we logistically carefully structure the work at all stages. The operating surgeon is responsible for everything that happens in the operating room. At the same time, a team of about 10-15 people works with him, sometimes a little more. If the operating surgeon does not control his emotions, he will not be able to control everything that happens in the operating room, and the situation may change during the operation; Not everything always goes as planned, you must be as composed as possible so that in case of surprise you can react adequately and quickly and make the right decisions.
Everything went smoothly for us. In our hospital, transplant surgery has a low mortality rate, and in 2017 there were no losses at all.
This does not mean that we work better than our other colleagues. Perhaps this is due to the fact that we select patients and donors more carefully and are afraid of making mistakes. And we still have fewer organ transplant operations than other clinics. Life will tell what will happen next. Besides, I repeat: teamwork is important. In recent years, more than 100 specialists have undergone appropriate training, and repeatedly. Transplantation programs began in many clinics across the country, and then it all died out - something went wrong. Perhaps the team didn't work out.
...I can’t say I was very nervous. I thought through the operation plan and sequence of actions several times. Another specificity is that every action performed during this operation is our daily work. You just need to put these actions together in a certain sequence to get another operation - a heart transplant.
– Vyacheslav Leonidovich said that human relationships with those from whom you learn are important. But you can just watch...
– Many are ready to share knowledge, but a human, friendly professional conversation is structured in a completely different way, there is a discussion of nuances, a person will not hesitate to talk about difficulties, non-standard situations, when something went wrong, not according to the planned scenario, and it was necessary to undertake non-standard action, and quite quickly. You can’t tell everyone about this, as well as about your mistakes.
Meanwhile, such conversations are very important, and everyone understands this. By the way, in recent years there have even been conferences, international and Russian, with this specific theme and appropriate titles, for example, “My Nightmares in Surgery.” We are talking about non-standard situations with extremely seriously ill patients, non-standard solutions, and even those cases where everything ended negatively. Anyone who has such a sad experience then repeatedly analyzes the situation and asks himself: will everything that should have been done be repeated? And it is more useful to discuss such situations in a professional circle. This is a sensitive topic and rarely is anyone willing to discuss it publicly. Therefore, other options are also practiced. At congresses of cardiothoracic surgeons, one of the sections is devoted specifically to non-standard situations. Famous surgeons are presented with a conditional non-standard situation, they discuss it, express different views, and argue.
...Many monographs have been written on how to do it. But what to do if something doesn’t go according to plan - such a conversation is possible if the relationship between colleagues is trusting.
...Transplantology is not always a predictable process; everything depends on a large number of factors. These are always emergency operations, often outside of working hours, at any time of the day; We all almost always change our plans. When we flew to Moscow to see these operations and take part in them, we often had to live there for several days waiting for them. It’s the same with trips to Krasnodar: it became known about a possible operation, all plans changed, I got into the car and drove.
I say this because in our hospital, sometimes at inopportune times there is an urgent need for consultation with those who have more experience. At any hour we can call our colleagues who helped us introduce organ transplant operations into everyday practice, we can consult with them even at night. It is important; It’s better to double-check yourself; why take the risk.
In general, everything related to negative outcomes in transplantation is viewed by society through a magnifying glass. When something goes wrong in other areas of surgery, they reason like this: well, life is life, a difficult patient... But here everything is different. And we see that there is also a social problem in this.
– What if the operating surgeon comes to work and feels unwell? My head hurts. Or stomach...
- Well, how bad is it? If it’s really bad, you need to get treatment. And if there is a common malaise, a person is designed in such a way that he mobilizes and does his job.
– This is a bad question, I’m even afraid to formulate it. On average, how do these surgeries help people?
– The question is absolutely correct. A person must know what he is doing, whether it makes sense to take risks or whether it is better to live, how much is allotted. The lifespan of a donor organ varies, depending on many factors. There is a very famous photograph that has spread all over the world: an incredibly tired cardiac surgeon in the operating room, immediately after a heart transplant, which lasted more than 20 hours. And the second picture shows the same patient, years after the operation. His surgeon died long ago, but the patient lived fully after the transplant for almost 30 years and died last year at an old age.
Another famous story: Rockefeller, who died not so long ago at the age of 101, underwent 6 heart transplants, the first one took place at a respectable age - he was about 60. If you calculate arithmetically, each “new heart” lasted him an average of 6 years. But I think that he hardly restrained himself in his desires, hoping that they would do what he wanted, when he needed it.
It's different for everyone. There are patients who live a long time. But there are completely inexplicable situations; rejection of the heart or liver cannot be justified or explained, first of all – for oneself. This happens in both Russian and world practice - at different time periods after the operation, although according to all data nothing happens, everything is going well, he should live and live, but some currently inexplicable mechanisms are triggered. Thank God this doesn't happen often.
We had one case. Kidney transplant. The kidney started working perfectly, but then, gradually, over 2 weeks, the function faded, and we saw no explanation: everything was going as normal. We consulted with more experienced colleagues, told us everything in detail, and they answered us: yes, this happens; Even in world practice, according to statistics, 8-10% of such cases.
...There are statistics: 10 years – survival rate is about 70%. But everything is very individual.
– Your thick newspapers are in English. How fluent are you in the language?
- To a sufficient extent. Not all necessary literature is in Russian. Reading English is one thing; If something is not clear, you can dig around and use the links to understand it. And another thing is, when there is live communication or a lecture, there is no way to clarify what is not clear in the current mode. I studied extra and now I’m trying to study the language; this is a necessity.
– Courses, internships abroad – how useful are they?
– There is benefit and expediency. At the same time, I was very pleased to understand (for example, in Germany) that we are no worse professionally, and in some moments even better. One day I went into the operating room with one of the German surgeons, operated with him, and it turned out that my preparation was better. And without asking, he signed me up for all his operations while I was in Germany. His goal was clear - to learn. My goal was different, I had to politely apologize and study according to my plan. But, of course, there is a lot to learn from them too.
...Vyacheslav Leonidovich touched on this topic, I want to continue it: not only we study abroad; There are stories widely known in narrow circles when foreign surgeons learned from our great doctors what no one else in the world could do. Christian Barnard performed the first heart transplant operation in South Africa, overnight made history and became a very rich man. And he learned everything from our Vladimir Petrovich Demikhov, an experimental scientist who, in an experiment, performed all possible operations in transplantology. The first monograph on transplantology is his work. And Demikhov is known, even today, in a fairly narrow circle of professionals. Why is that? And why is this still the case today?
There are also a number of Soviet scientists and surgeons who were the first to develop and perform unique operations. And these methods became widely known abroad and then came back to us as their methods. The peculiarity of our history and mentality is that they did not receive the fame and recognition that our people should have received. It's not fair; but that's one question. Another question is that we learn lessons from history.
Governor Vasily Golubev and Minister of Health of the Rostov Region Tatyana Bykovskaya at a meeting with transplantologists of the Rostov Regional Clinical Hospital on December 3, 2021.
...Indeed, hundreds of thousands of people have never heard the name, for example, Barbuhatti. Only specialists know about Voskanyan. And the Box? About twelve years ago I heard a true story. The man, a high-ranking military pensioner, had been operated on six or seven times - in Moscow, abroad; oncology. As a result, I heard: “We can’t do anything else.” In Rostov they told him the name of Vyacheslav Leonidovich and said that he was working miracles (he already worked at the Republican Regional Clinical Clinical Hospital). The patient had nothing to lose. The operation was successful, and the patient then lived and lived; maybe he still lives... There are many such stories.
Irina Nesterenko, Forum on Don magazine, February-April 2018
Carrying out a heart transplant operation
Heart transplantation requires modern equipment and highly qualified doctors to perform the operation.
For this reason, transplantation is carried out in special research centers equipped with specific equipment.
- What do diabetics need to know about using the Fit Parade sugar substitute?
The operation is performed by several teams of surgeons who replace each other. During the procedure, the patient's condition is monitored by a team of anesthesiologists.
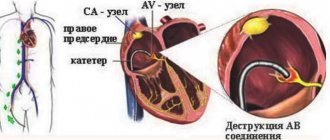
There are two methods used for heart transplantation:
- biatrial - the patient’s heart is partially removed, preserving the atria, to which the donor organ is brought;
- bicavia - the donor heart is brought to the superior and inferior vena cava, without preserving the recipient's atria.
Progress of the operation
- The working field is disinfected. The sternum is cut along the chest using an electric knife.
- An expander is inserted into the surgical access area, fixing the tissue. The folds of the pleura shift.
- The pericardium is opened and a device is brought to the vena cava to stimulate blood circulation. The heart is restricted with clamps to exclude it from the circulatory system.
- It is removed along the lines corresponding to the chosen method of transplantation.
- The donor's organ is prepared for transplantation.
- The donor heart is introduced into the recipient's body and sutures are placed according to the previously chosen technique.
- Blood flow is restored by removing the clamps on the vessels.
- If the heart has not begun to function on its own, it is started with a cavity defibrillator or rhythmic compressions.
- The chest cavity is cleared of blood.
- The expander is removed, and the bones are fixed with wire sutures or plates. Soft tissues are sewn together.
Annual cash payment to persons awarded the “Honorary Donor of Russia” badge
Receiving the “Honorary Donor of Russia” badge allows you to receive social support measures listed in Art. 23 Federal Law No. 125 dated July 20, 2012, one of them is an annual cash payment.
The amount of such payment is 10,557 rubles (see Article 24 of the Federal Law dated July 20, 2012 No. 125). It is indexed once a year on January 1, based on the inflation rate, which is established by the Federal Law on the federal budget for the appropriate financial year and planning period. This compensation is not subject to personal income tax. The annual payment in 2021 is RUB 15,109.46.