Since the introduction of coronary artery bypass surgery (CABG), medicine has made great strides in the treatment of coronary heart disease (CHD). As surgical experience accumulated, it became obvious that candidates for surgical treatment were elderly patients with a large number of risk factors, more severe forms of coronary artery disease, and those who had previously undergone cardiac bypass surgery. Studies have shown that in approximately 25% of cases, the diameter of the coronary vessels is insufficient for effective bypass surgery [1]. Moreover, some of the vessels have diffuse atherosclerotic changes, and they also cannot be bypassed. An equally important problem remains the determination of treatment tactics for patients who have undergone multiple myocardial revascularization procedures. The above problems have forced researchers to look for new ways for adequate myocardial revascularization.
With the beginning of the active introduction of direct methods of myocardial revascularization, attempts to find new methods of indirect revascularization continued. The use of a laser for transmyocardial laser revascularization (TMLR) is based on the characteristics of the myocardial circulation. During evolution, mammals and humans retained some features of the blood circulation of reptiles and more primitive creatures. The blood supply to the myocardium is carried out not only through the coronary arteries (CA), but also through the arteriolaminar canals and myocardial sinusoids. It has also been found that under conditions of stress there is an increase in these alternative pathways [2].
The authors developed the possibility of oxygenated blood flowing from the cavity of the left ventricle into the ischemic myocardium by creating artificial transmyocardial channels using acupuncture [3, 4]. The use of a laser made it possible to avoid harsh mechanical effects on the myocardium when creating tunnels [5, 6].
The successful clinical use of transmyocardial mechanical acupuncture was first reported by White in 1967. The work of S. Jacques in 1969 on the use of lasers in cardiovascular surgery gave a new impetus to research on this topic.
In 2000, K. Allen et al. reported a multicenter randomized study using holmium laser, which also demonstrated the safety and effectiveness of these operations.
In the world literature, unfortunately, there are not enough studies of combined CABG and TMLR, in which transmyocardial laser revascularization was performed using a CO2 laser; most of the data presented concern operations in which TMLR was performed using a holmium laser [7–9].
In this study, we assessed the safety and effectiveness of transmyocardial revascularization in combination with coronary artery bypass grafting in patients not amenable to complete revascularization.
Material and methods
In the period from 2007 to 2013, at the Department of Cardiac Surgery No. 2 of the Rostov Regional Clinical Hospital (Rostov-on-Don), more than 5,000 coronary bypass surgeries were performed, of which 60 patients underwent CABG in combination with TMLR. Informed consent was obtained from each patient. The criteria for inclusion in the study were diffuse lesions of the coronary artery, atherosclerotic changes in the distal bed or the presence of small coronary arteries unsuitable for bypass surgery, and preservation of viable myocardium in the surgical area. If direct revascularization of at least one coronary artery was possible, CABG was performed, which was supplemented by TMLR in those areas that were not accessible to revascularization. Exclusion criteria were severe chronic obstructive pulmonary disease (forced expiratory volume in 1 s <55% of the predicted value); acute period of myocardial infarction; severe rhythm disturbances; decompensated heart failure.
The study group consisted of 52 men and 8 women aged from 46 to 81 years (average age 65.9±7.3 years). Most patients ( n
=44) had angina pectoris IV F.K. The general summary characteristics of the patients are presented in Table. 1.
Table 1. General characteristics of patients Note.
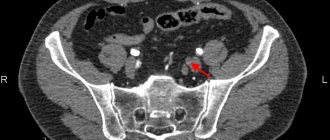
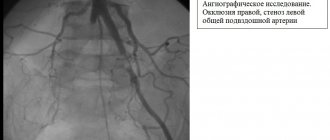
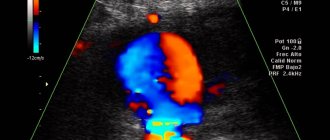
LVEF - left ventricular ejection fraction, MI - myocardial infarction, CHF - chronic heart failure. To objectify the condition, patients underwent coronary angiography and Holter ECG monitoring. Determination of angina class was carried out according to the recommendations of the Canadian Cardiovascular Society and the modified Bruce protocol. Before surgical treatment, patients were unable to perform stress tests (treadmill test) due to severe angina. To diagnose myocardial viability, myocardial scintigraphy and echocardiography were performed. All operations were performed in a standard manner: under conditions of artificial circulation and pharmacocold cardioplegia with Custodiol solution. In all cases, CABG was first performed, then TMLR was performed after the application of shunts and restoration of blood flow in the coronary artery under conditions of artificial circulation (CPB). In all cases, laser revascularization was performed using the domestic ECG-synchronized laser device Perfocor. After positioning the manipulator handle above the surface of the heart, a pulse was applied, synchronized with the patient’s ECG relative to the R wave. Penetration of the entire thickness of the myocardium using a 500 W CO2 laser occurred in one pulse, which was confirmed by the appearance of a pulsating stream of blood from the transmyocardial channel, as well as by transesophageal echocardiography data in in the form of gas bubbles in the cavity of the L.Zh. In this case, no rhythm disturbances occurred, and bleeding from the canal stopped on its own or by pressing with a gauze pad or napkin for 2 minutes. An active drain was installed in the pleural cavity, and the chest was sutured using standard techniques.
In all patients, in-hospital, long-term and overall mortality rates were assessed, as well as the dynamics of such clinical parameters as angina FC, the need for nitroglycerin, exercise tolerance, myocardial contractility, LVEF, myocardial perfusion. The dynamics of quality of life were determined using SF-36 questionnaires, and the psycho-emotional and physical state of patients was assessed at various times after surgery. Survival rates, freedom from recurrence of angina and myocardial infarction in the long term were calculated.
Patients were under clinical observation in the immediate postoperative period (in hospital or 30 days outpatient) and long-term period: 3, 6 and 12 months after surgery and then selectively up to 10 years after surgery (on average 7.5±0.9 years ). At each interval, patients were assessed for major adverse cardiac events, angina class, LVEF, and the need for repeat revascularizations.
In the first hours after surgery, invasive hemodynamic monitoring, ECG monitoring, blood gas composition, acid-base status and biochemical parameters, including enzyme markers of myocardial necrosis, were carried out. Analysis of the ECG in the first hours after TMLR showed that, despite the effect of the laser on the myocardium, there was no evidence of myocardial damage or ischemia.
Basic techniques for restoring blood circulation in the heart
There are two options for surgical myocardial revascularization techniques. The first involves minimally invasive percutaneous coronary intervention (PCI) aimed at eliminating the underlying cause of impaired blood flow. The second method is aimed at creating additional vascular connections (shunts) bypassing the affected area.
In the case of PCI, access is performed directly to the coronary vessels through the introduction of a thin catheter with a guide (diameter up to 6 mm) into the femoral or radial artery. The movement of the wire is monitored using an x-ray imaging method with a contrast agent.
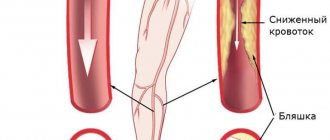
- Coronary myocardial revascularization using angioplasty . When entering the area of the stenotic lumen, a thin catheter is passed through the thickness of the atherosclerotic plaque. At this moment, a special balloon is inflated at the end of the electrode under a pressure of up to 20 atmospheres. The application of high force expands the lumen of the vessel, after which air is released from the balloon and the catheter is removed.
- Stenting involves repeating the previous technique with one difference - on the inflating balloon there is a cylindrical mesh - a “stent” made of special metal alloys, which prevents thrombus formation. After balloon angioplasty, relapses develop, the frequency of which decreases with the use of stents.
Less common options for intravascular intervention: laser burning or cutting off the atherosclerotic plaque with special instruments.
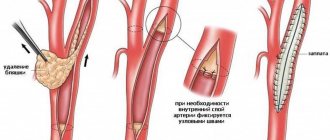
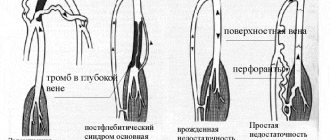
The second option of revascularization involves open heart surgery using a heart-lung machine. Depending on the vessel used to create a “bypass” blood supply, the following methods are distinguished:
- coronary artery bypass grafting (CABG) – the bloodstream of the affected coronary artery is connected to the lumen of the aorta through an additional vessel (most often the large or small saphenous vein of the lower limb is used);
- mammary coronary bypass surgery – the internal mammary artery is used as a source of blood supply.
results
Immediate mortality (in hospital or in the first 30 days) after combined CABG and TMLR was 1.6% (1/60). The cause of death was multiple organ failure. According to our data, the mortality rate was lower compared to the data given in the literature (1.6% versus 6.3%).
Postoperative complications are presented in table. 2.
Table 2. Postoperative complications (in hospital or within 30 days)
3 (5%) patients experienced rhythm disturbances (atrial fibrillation), which were treated with medication. The postoperative period in these patients was uneventful, and they were discharged from the hospital on time.
All patients were extubated on the 1st day after surgery. The length of stay of patients in the intensive care unit was 2.2±0.7 bed days. The use of intra-aortic balloon counterpulsation was not required in any case. The total length of hospitalization was 11.1±2.9 bed days. Before discharge, LVEF increased from 48.8±4.97 to 54.9±4.08%.
Thus, analysis of the immediate postoperative period showed that TMLR is quite safe for the patient and does not require an expansion of the standard volume of intensive care in the intensive care unit.
Long-term follow-up
Clinical follow-up of patients in the long-term period was carried out 3, 6 and 12 months after surgery and then selectively up to 10 years after surgery (on average 7.5±0.9 years). At each interval, patients underwent clinical and instrumental examination. The clinical status of the patient was assessed based on the dynamics of angina FC and treadmill test. Transthoracic echocardiography was performed to monitor the effect on global and segmental myocardial contractility.
The dynamics of angina FC in patients after combined CABG and TMLR are presented in the figure.
Dynamics of the functional class of angina before and after surgery.
All patients were admitted to the clinic with an initially high angina FC. By the 12th month after surgery, a sharp decrease in angina FC was detected. This trend was followed up to 5 years, then a slight increase in angina FC was noted, which required an increase in nitrate intake.
All patients showed an increase in exercise tolerance after 12 months of observation.
In the long-term period, on average 7.5±0.9 years after surgical treatment, 2 patients required treatment for angina (percutaneous transluminal coronary angioplasty was performed), which is associated with the progression of the atherosclerotic process in the coronary vessels.
Survival rate after 7.5±0.9 years was 91.6% ( n
=55).
Discussion
Transmyocardial laser revascularization has received approval for the treatment of patients with grades III and IV angina at five cardiac surgery centers in the United States (St. Luke's Hospital in Milwaukee, New York-Presbyterian Columbia-Cornell University Hospital, Mayo Clinic, Duke University Hospital, Massachusetts General Hospital), where it was performed. Prospective randomized studies. St. Hospital was involved in the implementation of the first stage of the protocol. Luke's in Milwaukee. The patients underwent combined myocardial revascularization—CABG and laser recanalization using a holmium laser. The second phase of clinical trials involved the use of TMLR both as a stand-alone procedure and in combination with CABG. 4 other centers were involved in this work. After surgery, patients were assessed for the frequency and intensity of angina, episodes of unstable angina, myocardial infarction and other clinical indicators, such as stress tests, myocardial scintigraphy with thallium [10]. Taking into account the clinical success of both isolated TMLR and in combination with CABG, at the VII Annual Conference of Cardiothoracic Surgeons in Barcelona (1993), TMLR received final recognition as an alternative method of myocardial revascularization, the third after CABG and percutaneous transluminal coronary angioplasty. The US Society of Thoracic Surgeons (STS) and the Society of Minimally Invasive Surgeons (ISMICS) came to the conclusion that the evidence of the effect of combined operations indicates the validity of their use in this severe category of patients [11-13].
In 2000, the results of combined operations in 20 patients in whom TMLR was performed using a holmium laser were presented by G. Actis Dato et al. from the University of Cardiac Surgery in Turin (Italy) [14]. In 2004, J. Van der Sloot et al. published a randomized trial using the XeCl laser [15]. In 2010, S. Pratali et al. published long-term results (up to 12 years) of using a holmium laser [16]. All these works showed a temporary (up to 1 year) improvement in the condition of patients with subsequent return of angina.
In Russia, a number of studies were carried out at the Scientific Center for Cardiovascular Surgery named after. A.N. Bakulev, Novosibirsk Research Institute of Circulatory Pathology named after. acad. E.N. Meshalkin [17] on the topic of surgical treatment of patients with coronary artery disease using CABG in combination with and without TMLR. The results of using a CO2 laser were evaluated. The data obtained in both studies are quite comparable with ours: angina FC in patients after CABG + TMLR significantly decreased by more than 2 classes in all studies. The need for nitrates has also decreased. In the long-term period, up to 10 years, a significant increase in LVEF and an improvement in the quality of life of patients was revealed.
In the world literature, sufficient attention has been paid to evaluating the results of combined CABG and TMLR, but the authors used different lasers: CO2 laser, Ho:YAG, XeCl. Also, in most reports, the assessment of results is based on a small number of observations. This applies to systematic reviews, randomized trials, meta-analyses, and large non-randomized single-center studies. Each of these works has certain disadvantages. For example, in the largest of them [16–18], the results of combined coronary artery bypass surgery with transmyocardial laser revascularization are compared with the data of isolated CABG in a group of patients with uncomplicated coronary artery disease without diffuse coronary artery disease, or the results are summarized in centers performing a small number of operations.
O. Howard et al., using a CO2 laser, observed a decrease in the size of myocardial infarction and an improvement in regional contractility after TMLR. They explain the benefits of TMLR, which have been verified histologically. Endocardium undergoing laser revascularization in dogs also demonstrated preservation of myocardial function during acute ischemia due to improved perfusion through the laser channels.
Long-term benefits on angina and exercise capacity are more difficult to assess after combined CABG and TMLR due to the strong beneficial effects of bypass surgery. In our study, in the long-term period, the patients' condition significantly improved, angina FC decreased by more than 2 classes in all patients, and exercise tolerance increased.
Yet the mechanism of TMLR remains controversial and may be multifactorial. There are currently no convincing theories. Functioning shunts make a certain contribution to improving the condition of patients. The clinical effectiveness of TMLR requires further research.
Alternative techniques for surgical revascularization
Modern medicine has various means of minimally invasive revascularization. They are alternatives to classical surgical methods of excision of arteries (arteriectomy) - but are by no means methods of alternative medicine. These means have been adopted by official medicine, which today practically no longer gives preference to the classical means of vascular surgery.
Modern minimally invasive techniques are commonly called endovascular surgery. She is given preference. Endovascular surgery meets the interests of patients: the treatment is less painful, less traumatic, and postoperative rehabilitation is faster. The only question is whether this or that surgical clinic has equipment for minimally invasive endovascular operations and therapeutic actions, and whether its staff has the necessary experience.
Endovascular procedures involve the use of vascular catheters placed along the internal lumen of the artery not through an external incision, but through small “punctures” made in the shallowest areas of the artery (for example, in the groin). Attachments on catheters make it possible not only to catch a blood clot to remove it out, but also to expand the vessel from the inside (balloon dilatation) and implant a stent (a vascular frame that prevents its narrowing).
The modern technique of interventional thrombolysis (chemical decomposition of a blood clot) is based on the catheter administration of decomposing substances that treat the body of the blood clot. If the position of the blockage site is sufficiently “convenient,” substances for thrombolysis (streptokinase, urokinase, rt-PA drug) can be administered directly at the site where the artery is punctured.
Thrombectomy immediately frees the internal lumen of the artery. This means that blood flow is immediately restored. It takes time for the blood clot to chemically break down. Therefore, thrombolysis can be performed when the artery is not completely blocked. Or with simultaneous bypass of the blocked area (establishment of temporary bypass blood flow).