Tonometer indicators are considered one of the most important in identifying the quality of human health. There are two main meanings. Systolic blood pressure is noted at the moment of cardiac output, that is, the maximum contraction of a muscular organ. Diastolic or inferior - when the cardiac structures relax.
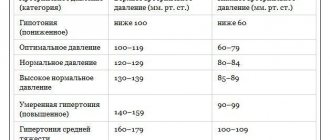
110/80 mm Hg. Art. blood pressure itself is normal, if you look at purely formal calculations. According to the World Health Organization, an adequate blood pressure level is considered to be between 100 and 139 per 60 to 80 or so. All other numbers are pathological.
This scheme does not take into account one point, it is called pulse pressure (abbreviated as PP). The indicator is calculated as the difference between systolic and diastolic levels.
According to national cardiology societies, a value between 40-50 mmHg is considered acceptable. In the case described, we are talking about 30, which is slightly below the norm.
The condition is often caused by dangerous diseases of the cardiovascular system, there are exceptions. A differential, thorough diagnosis puts an end to the issue.
What does 110 to 80 mean?
The blood pressure level itself within the specified limit is considered normal. Doctors proceed from this when checking a patient’s health status as part of a diagnosis or preventive examination. PD remains on the sidelines, which is fundamentally wrong.
With a formally acceptable tonometer value, an organic process is observed. Low pulse pressure indicates that the heart is unable to function normally. Myocardial contractility falls within moderate limits.
This may be due to insufficiency, coronary disease, or defects. In some cases, the reasons have nothing to do with the heart at all and affect it indirectly.
Thus, a pressure of 110 over 80 is not normal due to an indication of myocardial dysfunction. This leads to complications: decreased hemodynamics, tissue ischemia and hypoxia, problems with organs and distant systems, including the brain, kidneys and liver.
With pulse 80-90
A heart rate of up to 90 beats per minute is considered normal. It does not require any correction.
With an adequate heart rate against the background of a drop in pulse pressure within 30 mm Hg, there are most likely no pronounced functional changes in the myocardium.
The pathological process is in early, not yet advanced stages. This means that the prospects for a cure or at least partial correction to ensure life expectancy are good.
There are exceptions; you need to look at the data of ECG, ECHO-CG and 24-hour Holter monitoring.
With a pulse of 100 or more
Tachycardia indicates the development of pronounced changes in cardiac structures. A pressure of 110 over 80 with a pulse of 100-110 may indicate a malfunction of the sinus node or paroxysms due to blockade of the His bundles.
Recovery is difficult. This is a relatively rare variant of the clinical picture. The reverse process is more common.
Less than 80 beats per minute
The so-called bradycardia. Makes it clear that the myocardium cannot cope with the load or is not receiving enough nutrition or oxygen.
A decrease in heart rate poses a great danger to life, sudden death is possible. There can be a lot of clinical options: from bundle branch block to severe insufficiency.
Is 90/50 pressure adequate in different cases?
When assessing the adequacy of such an indicator, you need to take into account a lot of factors. Among them are gender and age characteristics, general health status, hormonal levels and some other points. We should consider them in more detail.
Children, teenagers
For children under 8-9 years of age, a blood pressure level of 90 to 50 is quite normal, but if we are talking about the youngest patients, it may even be elevated. Children have their own norm, you need to talk about this with a pediatric cardiologist.
For teenagers the situation is different. In most cases, this level of blood pressure is acceptable, but not desirable.
The age of 12-19 years is the phase of puberty: a very complex state from a physiological point of view. Your health worsens, your blood pressure fluctuates and can be either low or high during the day.
It is extremely difficult to manage such patients, since there is no clear clinical picture.
A thorough examination and correction of the condition in extreme cases is necessary. In most clinical situations, you don’t need to do anything; everything goes away on its own at a certain point.
In the elderly
Hypotension in elderly patients is an extremely rare phenomenon, indicating problems with the cardiovascular system. This is not an absolute truth, but a common occurrence.
Hypertension is more common in old age. That is, the reverse process, an increase in blood pressure, sometimes to levels leading to a hypertensive crisis.
Patients of this kind need to be carefully monitored and therapy must be constantly adjusted. Conducting early screening for pathologies of the cardiovascular system is the key to a normal quality of life.
During pregnancy
Hypotension in pregnancy is common. Even at such a pronounced level. There is no need to do anything; in rare cases, if your health does not allow you to live a full life, it is recommended to contact a specialist.
Endocrine factors
In healthy patients with normal hormonal levels, an upper pressure of 90 may be normal. A diastolic level of 45-50 is always pathological. It is necessary to understand the situation. Perhaps this is due to hormonal imbalances.
Are such numbers dangerous?
Yes, these indicators pose a threat to life and health. Close to them, 110 to 85, 105 to 75, when the pulse pressure is identical, have the same forecasts. But the others, 105 to 80 as an example, are much more serious, since the PD is even lower.
What are the possible consequences:
- Heart failure. In the event of urgent resuscitation, there is still a chance to return the patient.
- Heart attack. Acute death of muscle organ structures.
- Stroke. Brain nutritional disorder. Necrosis of nerve tissue leads to severe neurological deficits. The prospects for recovery depend on the extent of the damage.
- Shock resulting from a sharp drop in blood pressure and blood output.
- Impaired cognitive and mnestic functions as a result of insufficient supply to the brain. May result in vascular dementia.
- A general decrease in the quality of life, a decrease in working capacity and other important biological and social indicators.
However, the risks are at an average level. This is not a critical condition yet, but it is not the first phase either. Most likely, the pathological process is already underway, and it will be noticeable in instrumental diagnostics and even to the patient himself. If you listen to your own body.
Reasons for reduced PD
Low pulse pressure does not always develop due to damage to the cardiovascular system. But more often than not it turns out that way. An approximate list of development factors:
Heart attack
Especially if the left ventricle is affected. Usually we are talking about a slight extent of damage to cardiac structures (microinfarction). Therefore, the indicator drops insignificantly, being within 25-30 mm Hg or a little more.
Contractility is still present, so the body is supplied with blood to an acceptable extent.
With a large area of damage, intense disruption of the release into a large circle occurs. Cardiac shock and death are possible. In such a situation, pulse pressure drops to critical levels.
The pathological process needs to be viewed in exactly this way. Accordingly, a slight decrease in PP is associated with a relatively favorable prognosis for recovery after an emergency condition.
Aortic stenosis
Usually at valve level. There is an impossibility of normal blood ejection into the largest artery. Blood stagnation occurs in the left ventricle. This leads to constant overstrain of cardiac structures.
As it progresses, dilatation (expansion) of the organ chambers occurs. Contractility is insufficient, the volume of liquid connective tissue drops significantly for a whole group of reasons: not only stenosis is to blame, but also changes in the anatomy of the heart.
Pulse pressure decreases as a result of incomplete contraction, with short periods of rest between each cycle. Over time, the process only gets worse, so the likelihood of recovery depends on the moment the defect is discovered. The later, the worse the prognosis.
Neurological abnormalities
To a small extent, cardiac activity is controlled by the brain. If the functioning of cerebral structures is impaired, arrhythmias and insufficiency of myocardial contractility may develop.
This is a characteristic feature of vegetative-vascular dystonia. In origin it is a symptomatic complex, and not an independent diagnosis.
The diagnostic task becomes more complicated: when identifying VSD, it is also necessary to discover its cause.
Mitral valve insufficiency
It delimits the left atrium and ventricle, passing blood in measured quantities strictly in one direction. When an anatomical structure is disrupted, a reverse current or regurgitation occurs, which ends in a well-known manner.
Dilatation occurs, followed by cardiomyopathy, a decrease in myocardial contractility, a drop in blood output, and therefore pulse pressure. And there is already one step before progression, cardiac arrest and death.
The scenario is excluded with timely surgical treatment with restoration of the integrity of the mitral valve or prosthetics (preferably).
Heart failure
Both in the first and second stages. The patient feels minimal discomfort, but the process actively continues, destroying the system. Diagnostics is carried out using instrumental methods.
Recovery requires combating the root cause, as well as symptomatic therapy to eliminate manifestations.
Other heart defects, congenital and acquired
They require timely surgical treatment. They are not always detected immediately, and therapy is not needed in all cases.
In order not to miss an important point, it is recommended to undergo preventive examinations with a cardiologist every six months to a year, as well as an ECG and ECHO to detect any abnormalities. The need for therapy is decided on an individual basis.
How can you help yourself at home?
You can increase the pressure 90 to 50 yourself. But with further negative dynamics of the process, if the pressure drops further, you need to call an ambulance.
Before the arrival of doctors or as initial measures, the following must be done:
- Lie down, calm down. Do not make sudden movements. Moreover, do not jump out of bed.
- Take one tablet of a tonic: Citramon or aspirin. But no more, otherwise the pressure will jump sharply. The drugs do not act immediately, but after half an hour to forty minutes. One tablet in this period of time is enough. The daily maximum is 6 tablets.
- Drink coffee, tea or a salty product (of your choice) to normalize the condition.
- Assess and record pulse and blood pressure for reporting to the attending physician or paramedic upon arrival of the ambulance.
Before the ambulance arrives or until you feel better, you should avoid showers, baths, and excessive water consumption. The condition may worsen.
Noncardiac causes
Represented by a group of heterogeneous processes:
- Iron deficiency and megaloblastic anemia. Associated with an insufficient amount of hemoglobin in the blood. Lead to the development of disorders of the cardiovascular system.
Mortality is relatively low, because the process can continue for a long time with the same symptoms, without dynamics. A drop in pulse pressure is a possible option. The sign is not always observed.
- Kidney failure and other diseases of the excretory system. If the filtering function is impaired, an increase in the amount of circulating blood occurs. This leads to increased stress on the heart. Possible drop in PD. This is a response to overstimulation.
- Liver failure. Including against the background of hepatitis, cirrhosis and other pathologies of a destructive nature.
Attention:
Changes in pulse pressure are almost not directly related to bad habits or lifestyle. This is an indirect process. What distinguishes the disease from simple forms of hypertension or hypotension.
Symptoms that require you to see a doctor
Manifestations of low PP are nonspecific. In the early stages, the patient may not feel any changes at all until the level drops to critical levels. Still, if you listen to your own body, you can detect signals.
- Dizziness. Against the background of a pressure of 110 to 80, vertigo develops as a result of insufficient supply of cerebral structures with nutrients and oxygen. Ischemia (oxygen starvation) of the cerebellum begins. The greater the volume of violation, the more significant the deterioration. There is a decrease in the efficiency of orientation in space.
- Cephalgia. The pain is localized in the occipital region, temples, and parietal zone. The nature of the discomfort is pressing, pulsating. Unpleasant sensations intensify in time with heart contractions. This syndrome can be falsely mistaken for a manifestation of migraine and vice versa. The duration of a headache episode with a pressure of 110 over 80 is from a couple of hours to a whole day.
- Loss of concentration. The result of the same hypoxia. In the early stages it has the form of slight absent-mindedness. Then it becomes more threatening. Patients with a progressive pathological process fall into a state of vascular dementia, which is very similar to Alzheimer's disease. Fortunately, a similar observation occurs when pulse pressure is below 30 mmHg. There are exceptions.
- Change in heart rate. A heart rate of 100 indicates impaired myocardial contractility. The problem can be localized both in the sinus node and in the ventricles, atria (paroxysmal type of tachycardia). A pulse of 80-90 is considered normal, lower indicates heart failure.
- Weakness, drowsiness, decreased performance. Up to the inability to perform everyday duties at home. Not to mention professional activities.
Symptoms requiring an ambulance call
Such signs occur in emergency conditions. Transportation to a cardiology hospital is indicated.
- Intense, unbearable headache.
- Vertigo, in which the patient is unable to navigate in space at all. Respiratory dysfunction. May indicate swelling or other dangerous conditions.
- Critical change in heart rate (more than 150 or below 60 beats per minute).
- Paresis, paralysis, sensation of goose bumps running through the body.
- Facial distortion.
- Loss of consciousness, repeated over several hours while symptoms persist.
Reasons for a one-time drop in blood pressure in patients
A single decrease in blood pressure rarely indicates complex pathologies of any profile. More often there are natural, physiological factors.
Among them:
- Overwork. As a result of increased stress on the body, cerebral circulation is impaired with inhibition of the regulatory centers of cerebral structures responsible for normal vascular tone. Usually the violations are not critical and are completely reversible.
- A sharp change in body position in space, unreasonably rapid movements. They cause so-called orthostatic hypertension. It is not only temporary, but also lasts no more than a few seconds or minutes. After the attack ends, everything returns to normal. But there may be adverse consequences such as fainting or dizziness and falling.
- Menstrual cycle. Lasts for different periods of time. Throughout the entire cycle, changes in the nature of cerebral circulation are observed. The decrease and increase in pressure is not one-time, but temporary, short in duration, therefore it cannot be classified as a pathology.
- Abuse of antihypertensive pharmaceutical drugs. The problem of patients with hypertension. If the dosage is incorrect, the pressure will begin to jump and become unstable.
- Post-stroke or post-infarction condition. During the rehabilitation period, a decrease in the tonometer reading is acceptable, but it is necessary to constantly monitor blood pressure levels and the general condition of the patient.
This is not a complete list, but the reasons presented are the most common in clinical practice. They are not dangerous and are reversible.
Examinations that need to be completed
Diagnosis is carried out on an outpatient or inpatient basis. Depending on the patient's condition.
Full list of studies:
- Orally questioning a person about his complaints.
- Anamnesis collection. Lifestyle, existing diseases, not necessarily those of the cardiovascular system, family history, and other factors are taken into account.
- Measurement of blood pressure and heart rate. Calculating PD does not present any great difficulties. Heart rate will additionally indicate the nature of the activity of cardiac structures.
- Electrocardiography. Allows you to assess the functional state of the myocardium. Makes it possible to identify developmental defects, as well as various types of arrhythmias. The ideal moment for this is the peak of the pathological condition.
- Daily monitoring. Blood pressure and heart rate are to be examined. The only difference is that they are recorded over 24 hours, over time. While the patient lives in familiar conditions, his health status is recorded.
- Echocardiography. Ultrasound research technique. Used to detect anatomical defects. Against the background of defects, congenital and acquired, these are obvious.
- General blood test, hormones and biochemical.
- Urine examination as needed.
- MRI of the brain.
- EEG.
- Scintigraphy.
It is possible to expand the presented list. Not only the cardiologist is involved in the diagnosis. If a cardiac origin of the drop in pulse pressure is excluded, other specialists are involved.
Blood pressure 100/60 – normal or pathological
Blood pressure 100/60 is the maximum acceptable lower normal value. For most people, this is the optimal pressure at which a person feels comfortable, does not make any complaints, and remains functional.
However, in some cases, such systolic and diastolic indicators indicate the presence of the disease.
Most often, the tonometer records numbers of 100/60 in slender girls or with orthostatic hypotension. This condition appears in the morning when abruptly getting out of bed, manifests itself as dizziness, flashing spots before the eyes, and threatens loss of balance and injury. Orthostaticity is also impaired in the postoperative period or after taking a number of medications.
Treatment
{banner_banstat9}
Therapy is carried out under the supervision of specialized doctors. The basis is medication. The drugs are applicable in all cases: they stabilize the patient’s condition before possible surgery, relieve symptoms and sometimes the cause, and prevent further aggravation of the process or its relapses.
List of drug groups:
- Cardioprotectors and means for improving metabolism in cardiac structures. Mildronate.
- Beta blockers. As needed, with great care. There may be a drop in blood pressure, and subsequently pulse pressure. Anaprilin or Carvedilol.
- Nitroglycerin for pain in the chest.
- Antiarrhythmic for pulse irregularities. If the change in heart rate is not stopped by other means (for example, the same beta blockers). Quinidine, Amiodarone.
Other groups are prescribed as part of extended individual therapy. Cases vary. The medications described are of symptomatic action.
For etiotropic influence (treatment of the underlying disease), a combination of drugs is required. The question falls on the shoulders of a specialized specialist, not necessarily a cardiologist.
Surgery is required in a limited number of cases. For example, to eliminate heart defects (stenosis, prolapse of the mitral, aortic valves and others).
In the same way, severe atherosclerosis with the deposition of calcium salts on the cholesterol plaque is stopped. This is an extreme measure, sometimes you cannot do without it. The drugs are used as a supportive technique.
Lifestyle changes at the onset of the pathological process do not play a big role. If you give up smoking, alcohol and adjust your diet towards fortification, your chances of recovery are greater. But it all depends on the main diagnosis and the effectiveness of the treatment.
If the pressure is 110 over 80, this means that an organic process is taking place: hormonal or cardiac. We need to figure it out.
The treatment regimen is developed by doctors. What you definitely shouldn’t do is resort to independent actions or take folk remedies.
Recommendations
Next, we consider the recommendations of specialists in the case of hypotension in elderly patients and pregnant women, as well as in cases of hypertension in children under 5 years of age.
For pregnant
If hypotension is physiological in nature and does not manifest itself as a violation of the woman’s condition, then the patient does not need treatment. It is imperative to monitor your blood pressure levels every time you visit an obstetrician-gynecologist or therapist. To normalize blood pressure, pregnant women will benefit from morning exercises, physical therapy exercises, water procedures (showers, douses, contrast foot baths), and massage. It is important to normalize sleep, the duration of which should be at least 9-10 hours a day.
For insomnia, the doctor may prescribe mild sedatives, but not barbiturate-based sleeping pills, as they are dangerous for the child. You should also diversify your diet. It should be rich in protein foods, fruits and vegetables. You can drink tea or coffee with milk only in the morning or afternoon; it is not recommended in the evening so as not to disturb your sleep. Women are also advised to take a closer look at herbal medicine recipes.
Important! The use of any remedies (both traditional medicinal and folk) during pregnancy should be discussed with an obstetrician-gynecologist.
For the elderly
The recommendations are as follows:
- Every day it is necessary to measure readings on both hands and record the data in a personal diary.
- You should get out of bed slowly so as not to provoke the development of orthostatic hypotension.
- It is important to have a hearty breakfast and drink a cup of weak coffee. Your daily diet must include foods rich in vitamins and minerals. If there are no contraindications, you need to drink enough liquid; you should not completely give up salt unless your doctor says otherwise.
- It is necessary to avoid prolonged stay in stuffy rooms, protect yourself from stress and significant physical exertion.
- Make time for walking and light exercise every day.
- If significant symptoms of hypotension appear, seek help from specialists.
Before using folk remedies to normalize blood pressure, it is necessary to exclude the presence of contraindications
For children
It is important to conduct a comprehensive examination to identify the cause of the pathology and select the necessary treatment, trying to return the numbers on the tonometer to normal without medications. What do we have to do? First of all, non-drug methods are used: changing the daily routine, adjusting the child’s menu, normalizing the ratio of rest and physical activity, etc.
Forecast
{banner_banstat10}
It is difficult to say exactly what a patient can expect. A group of factors is taken into account:
- Age.
- Floor.
- The nature of professional activity.
- History of somatic pathologies (concomitant).
- Duration of the condition.
- His reaction to the treatment.
- Degree of physical activity.
- Family history.
- Blood pressure level in general, over a longer period of time.
- Main diagnosis.
In general, an indicator of 30 mmHg against a background of blood pressure of 110 over 80 has good prospects in terms of preserving life. This is not yet a critical level, although it is an alarming signal. If treatment is prescribed, there is a high probability of full recovery.
A blood pressure of 110 over 80 in an adult is not normal due to low PP levels. This is an indication of pathology; natural factors do not lead to a decrease in the indicator. Diagnostics will put an end to the issue. Treatment methods and prognosis are determined after.
Is this blood pressure normal for pregnant women?
In women, a pressure of 100 over 70 during the period of bearing a child is perceived as quite normal, especially if at such indicators the pregnant woman feels well, and tests indicate the correct formation of the fetus. The female body is more changeable in terms of hormonal status and blood pressure due to the fact that its main functions are bearing children and childbirth.
Therefore, changes in hormonal levels affect the tonometer readings, especially since an additional circle of blood circulation appears in the body. An increased load is placed on the heart and blood vessels of the expectant mother, as a result of which pressure indicators also change. As the fetus develops in the womb and grows, the body tries to independently ensure relaxation of the uterus and prevent increased muscle tone and premature birth.
Therefore, the tonometer readings are recorded as underestimated, even if before pregnancy the normal blood pressure for a woman was 120/80 or 130/90. If the fetus is feeling well and is developing properly, there is no reason for concern in such a situation. The expectant mother should be wary if her blood pressure range is constantly fixed at 102-103 over 65 or 95 over 60.
Such symptoms of hypotension signal a threat of premature delivery or early miscarriage. If blood pressure drops to such limits and remains at this level, the child may have a heart attack in utero, oxygen starvation may begin, a blood clot may form in the placental tissue, or internal organs may not form properly.
If such symptoms occur, doctors try to monitor the pregnant woman in a hospital setting, where they can take emergency measures to stabilize the woman’s blood pressure and well-being. Moreover, with low blood pressure, she constantly has a headache, lethargy, drowsiness and tinnitus.
Do not think that blood pressure of 100/70 for a pregnant woman is a bad diagnosis. In the first trimester of pregnancy, such indicators are observed in most women, since during this period the hormone progesterone is intensively produced. It is necessary for the normal functioning of the uterus, full access to it of oxygen, vitamins and microelements. After a while, the pressure may return to normal levels and the woman’s condition will stabilize.