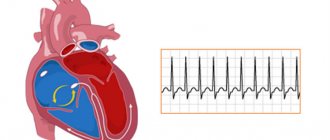
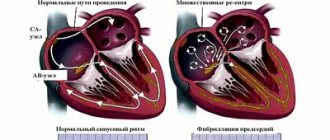
Under normal conditions, the human heart beats smoothly and regularly. The heart rate per minute ranges from 60 to 90 beats. This rhythm is set by the sinus node, which is also called the pacemaker. It contains pacemaker cells, from which excitation is transmitted further to other parts of the heart, namely to the atrioventricular node, and to the His bundle directly in the tissue of the ventricles.
This anatomical and functional division is important from the point of view of the type of a particular disorder, because a block in the conduction of impulses or acceleration of impulses can occur in any of these areas.
Disturbances in heart rhythm and conduction are called arrhythmias and are conditions when the heart rate becomes less than normal (less than 60 per minute) or more than normal (more than 90 per minute). Arrhythmia is also a condition when the rhythm is irregular (irregular, or non-sinus), that is, it comes from any part of the conduction system, but not from the sinus node.
Classification
All rhythm and conduction disorders are classified as follows:
- Heart rhythm disturbances.
- Conduction disorders in the heart.
In the first case, as a rule, there is an acceleration of the heart rate and/or irregular contraction of the heart muscle. In the second, the presence of blockades of varying degrees with or without slowing of the rhythm is noted.
In general, the first group includes disorders of the formation and conduction of impulses:
- In the sinus node, manifested by sinus tachycardia, sinus bradycardia and sinus arrhythmia - tachyarrhythmia or bradyarrhythmia.
- According to the tissue of the atria, manifested by atrial extrasystole and paroxysmal atrial tachycardia.
- At the atrioventricular junction (AV node), manifested by atrioventricular extrasystole and paroxysmal tachycardia.
- Along the fibers of the ventricles of the heart, manifested by ventricular extrasystole and paroxysmal ventricular tachycardia.
- In the sinus node and along the tissue of the atria or ventricles, manifested by flutter and fibrillation (fibrillation) of the atria and ventricles.
The second group of conduction disorders includes blockades in the path of impulses, manifested by sinoatrial block, intraatrial block, atrioventricular block of 1, 2 and 3 degrees and bundle branch block.
Certain types of blockades
Atrioventricular (AV) block
There are 1st, 2nd and 3rd degree AV blocks. 1st degree AV block does not manifest itself clinically; the diagnosis is made by ECG (when the PQ interval on the ECG exceeds 0.20 seconds). 1st degree AV block often occurs normally, for example in athletes. Some drugs are contraindicated in this case, which can lead to higher degrees of AV block.
With 2nd degree AV block, loss of individual heart contractions is observed. There are two types of 2nd degree AV block, called Mobitz I and Mobitz II. Mobitz type I block is more benign in nature; implantation of a pacemaker is almost never indicated for it. Mobitz type II AV block indicates more serious damage to the cardiac conduction system and is sometimes treated with a pacemaker due to the risk of complete AV block.
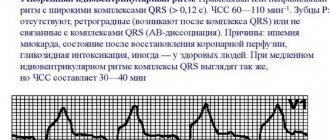
3rd degree AV block is complete AV block. Impulses from the atria to the ventricles are not conducted, the ventricles work due to the fact that the AV node generates its own impulses, their frequency, however, is lower than that which the sinus node is capable of creating, and this rhythm is generally less reliable. Therefore, complete AV block, even asymptomatic, is often an indication for the installation of a pacemaker.
Bundle branch blocks
Bundle branch blocks are also diagnosed by ECG. Incomplete blockade of the right bundle branch is a normal variant. Of all the variety of bundle branch blocks, only complete blockade of the left bundle branch deserves special attention. Firstly, it may indicate an anterior myocardial infarction; secondly, it itself leads to asynchronous (non-simultaneous) contraction of the walls of the left ventricle and can lead to heart failure. In recent years, a special type of cardiac pacing has been developed; it is called biventricular (two-ventricular) cardiac pacing (see below).
Sick sinus syndrome
This disease of the conduction system of the heart usually occurs in older people. It is manifested by fainting and pre-syncope (often during physical activity), and the so-called tachy-brady syndrome: a rare pulse is replaced by a frequent one when the patient experiences atrial fibrillation. At the same time, it is difficult to treat atrial fibrillation itself (atrial fibrillation), since most antiarrhythmic drugs slow down the heart rhythm. For sick sinus syndrome, pacemaker implantation is indicated.
Causes of cardiac arrhythmia
The causes of arrhythmia (the occurrence of heart rhythm disturbances) are so diverse that listing absolutely everything is a very difficult task. However, in many cases, the safety of the arrhythmia for the patient’s life and further treatment tactics depend on the cause of the arrhythmia.
Many different classifications of the causes of arrhythmia have been proposed, but none of them is currently generally accepted. We consider the following classification to be the most acceptable for the patient. It is based on the presence or absence of primary heart disease in the patient. If there is heart disease, the arrhythmia is called organic, and if there is no heart disease, it is called inorganic. Inorganic arrhythmias are also commonly called functional.
Organic arrhythmias
Organic arrhythmias include:
- Arrhythmias arising from coronary heart disease (myocardial infarction, angina). Arrhythmia is caused by damage to the heart muscle. It makes it difficult for electrical impulses to propagate correctly through the conduction system of the heart. Sometimes damage can even affect the cells of the main pacemaker - the sinus node. In place of the dead cells, a scar of connective tissue (cardiosclerosis) is formed, which is not able to perform the functions of a healthy myocardium. This, in turn, leads to the formation of arrhythmogenic foci and the appearance of rhythm and conduction disturbances.
- Rhythm disturbances that occur after an inflammatory process in the heart muscle - myocarditis. As a consequence, after suffering from inflammation, the myocardium is also replaced by connective tissue (cardiosclerosis).
- Arrhythmias observed in cardiomyopathies. For an unknown reason, myocardial cells are damaged, the pumping function of the heart is disrupted, and heart failure develops. In addition, various rhythm disturbances are very often associated.
- Arrhythmias that appear with various heart defects (congenital and acquired during life). It should be noted that there are congenital primary diseases of the conduction system of the heart itself.
Functional arrhythmias
This is also a fairly large group, including:
- Rhythm disturbances of neurogenic origin It is known that the heart is under the influence of the autonomic nervous system, which controls the activity of all internal organs. It consists of sympathetic and parasympathetic nerves. Their effect on the heart is opposite. An increase in the tone of the vagus nerve (this is a parasympathetic nerve) inhibits the work of the heart, and an increase in the tone of the sympathetic nervous system, on the contrary, stimulates its activity. Usually the influence of the vagus nerve and the sympathetic nerves are in a state of balance. However, during the day the activity of the sympathetic division of the autonomic nervous system prevails, and at night - the parasympathetic one. Excessive activation of sympathetic tone is promoted by stress, strong emotions, intense mental or physical work, smoking, drinking alcohol, strong tea and coffee, and spicy foods. The arrhythmias that arise at these moments are called sympathodependent. Often such rhythm disturbances occur in patients with neuroses. Activation of sympathetic tone also occurs in diseases of the thyroid gland, intoxication, feverish conditions, and blood diseases.
- Another group consists of vagus-dependent arrhythmias (from the Latin nervus vagus - vagus nerve). In such patients, interruptions in heart function occur at night. Diseases of the gastrointestinal tract: intestines, gallbladder, peptic ulcer of the stomach and duodenum, and diseases of the bladder can lead to an increase in the parasympathetic effect on the heart and, accordingly, to the appearance of gastrointestinal rhythm disturbances. Reflexes are formed in diseased organs, as a result of which the activity of the vagus nerve increases.
HAT Medicine
Case from practice.
When I was about 36 years old, I returned from visiting, where I drank a little. The mood was good. But I felt some kind of inner excitement. I don’t know what it was connected with. Suddenly, atrial fibrillation suddenly appeared. It did not go away and lasted about an hour, after which I decided to call an ambulance. I was given an injection of Novocainamide intravenously, after which the rhythm was restored right during the injection. I did not carry out any further special treatment. There were no rhythm disturbances. Subsequently, once or twice more I experienced atrial fibrillation, which lasted 10 and 40 minutes. Extrasystoles appeared very rarely. At one time they occurred when moving to a horizontal position during sleep, but then quickly passed.
They usually arose in cases where the activity of clinical attractors was observed in the gastric attractor. Since these were sporadic cases, I did not carry out specific NAT treatment for myself. I just strengthened my relaxation techniques at this time. Often walking around the room, I relaxed my fingers, my hands themselves. I paid special attention to relaxation in the esophagus area. To do this, taking a small sip of warm water, I imagined how the water passes through the esophagus, causing it to relax. At the same time, the diaphragm also relaxed. If you belch after this, then this is evidence of good relaxation.
Irregular heart rhythm (arrhythmia)
Irregular heartbeat is an arrhythmia. Your heart rate may also be irregular. The normal heart rate is from 50 to 100 beats per minute. Arrhythmia and abnormal heart rate do not necessarily occur simultaneously. Arrhythmia can occur against a background of a normal heart rate or even a slow rate (called bradyarrhythmia - less than 60 beats per minute). Arrhythmia can also occur against the background of an accelerated heart rate (called tachyarrhythmia - more than 100 beats per minute). In the United States, more than 850,000 people are hospitalized each year due to arrhythmias.
What causes arrhythmia?.
Arrhythmia can occur due to many different factors, including the following (common beliefs):
- Cardiac ischemia.
- An imbalance of electrolytes in your blood (such as sodium or potassium).
- Changes in your heart muscle.
- Damage due to cardiac risk.
- Recovery processes after heart surgery.
- Abnormal heart rhythms can also occur in a “normal healthy” heart.
The cause of arrhythmia from the perspective of HAT medicine.
Although it seems to us that our heart rate is rhythmic, this is not entirely true. If we determine the heart rate not per minute, but at another longer time interval, we will notice that the rhythm is not rhythmic. It is known that sinus arrhythmia in young people is associated with breathing and is completely normal. When you inhale, the heartbeat increases, and when you exhale, it decreases. Sinus arrhythmia decreases with age but persists in healthy hearts. These are manifestations of healthy chaos. That is, normal ri. It is with this rhythm that the heart better adapts to various loads and better tolerates stress. In cases of severe heart disease (in the absence of arrhythmia as a disease), as scientists have shown, the pulse is very rhythmic and does not change for a long period of time. This is a poor prognostic symptom. According to the NAT system, arrhythmia occurs either when there is a violation of the gastrointestinal tract or the genitourinary tract. We haven't clearly decided on this yet. When we have more experience, we will be able to treat rhythm disturbances very quickly (not too advanced, of course). We don't do that yet.
What types of arrhythmias are there?
Extrasystoles Premature atrial contractions. These extrasystoles occur in the atria (upper chambers of the heart). They do not cause harm and do not require treatment.
Ventricular extrasystole . This is the most common type of arrhythmia and occurs in people with and without heart disease. We all feel those missed heartbeats sometimes. In some people, they occur due to stress, excess caffeine, nicotine, or too much exercise. But sometimes ventricular extrasystoles can occur due to heart disease or electrolyte imbalance. People who experience these episodes frequently and/or are bothered by associated symptoms should be evaluated by a cardiologist. However, for most people, ventricular premature beats do not cause harm and rarely require treatment.
Atrial fibrillation . This is a very common type of heart rhythm disorder in which the atria (upper chambers of the heart) contract abnormally.
Atrial fibrillation (atrial flutter ). This arrhythmia occurs due to the impulse circulating too quickly through the atrium. Atrial flutter is usually more orderly and regular than atrial fibrillation. It most often occurs in people with heart disease and in the first week after heart surgery. Also, flutter often turns into atrial fibrillation.
Paroxysmal supraventricular tachycardia (SVT) .
This is a rapid heart rate, most often regular and comes from the upper parts of the ventricles. Paroxysmal SVT occurs and ends suddenly. Ventricular tachycardia. The accelerated heart rate comes from the lower parts of the heart (ventricles).
It prevents the heart from filling adequately with blood, so the heart pumps less blood into the body. This arrhythmia can be severe, especially in people with heart disease, and may be associated with other symptoms. People with such arrhythmia should be seen by a cardiologist. Ventricular fibrillation. This is a continuous, disorganized flow of impulses from the ventricles. The ventricles flutter, as a result of which they cannot contract and pump blood throughout the body.
Ventricular fibrillation is a very serious complication of heart disease that can lead to death. Immediate defibrillation is required.
We have all heard about the sudden death of young people. These could be football players, boxers. In some cases, this happens because they receive a strong blow to the chest, where the left ventricle is located. They develop ventricular fibrillation. Only in 15% of cases is it possible to quickly defibrillate and save the person. They may have had a long QT symptom. QT is the area on the electrocardiogram (ECG) that reflects the time the heart muscle spends contracting and then recovering. Long QT syndrome is inherited. Heart block. Slowing or complete blocking of the passage of electrical impulses on the way from the sinoatrial node to the ventricles. The level where the impulse is slowed or blocked may be in the atrioventricular node or in the His-Purkinje system. In this case, the heart may beat irregularly and often at a slower rate. If the heart block is severe, then implantation of a pacemaker is necessary.
What are the symptoms of arrhythmias?
Ari and not show any symptoms. Your doctor can detect an irregular heartbeat by feeling your pulse during a physical examination or by examining an electrocardiogram (ECG). If symptoms occur, they may include:
- Palpitations (the feeling of the heart skipping beats, fluttering or tumbling in the chest, or the feeling that the heart is jumping out of the chest).
- Sensation of dull knocks in the chest.
- Dizziness or feeling of confusion.
- Fainting.
- Dyspnea.
- Discomfort in the chest.
- Weakness or fatigue (feeling very tired).
Treatment depends on the type and severity of your arrhythmia. Some people with arrhythmias do not need treatment. Others are treated with medications, lifestyle changes, and surgical procedures.
What medications are used to treat arrhythmias?
Antiarrhythmic drugs. These medications control your heart rate and include beta blockers. Anticoagulant or antiplatelet therapy. Drugs in this group reduce the risk of blood clots and stroke. These include warfarin (a "blood thinner") or aspirin. Because these medications work quite individually, it may take time to try several medications and find the dose that is optimal for you.
What lifestyle changes do I need to make?.
- If you notice that your irregular heart rhythm most often occurs during certain types of exercise, then try to avoid them.
- If you smoke, you should definitely quit smoking.
- Limit your consumption of alcohol and other microbial fermentation products (NAT diet).
- Limit your caffeine intake.
- Stay away from stimulants used for coughs and cold medications. Some of these medications contain substances that can cause abnormal heart rhythms.
- Naturally, physical exercise is necessary for prevention and treatment: walking.
- A special place should be given to relaxation. Normalize your sex life. An incorrect rhythm can provoke arrhythmia.
What is a pacemaker?
A pacemaker is a device that sends low-intensity electrical impulses to the heart muscle to maintain an adequate heart rate. Pacemakers are usually used to prevent the heart from beating too slowly. They consist of a generator (which contains batteries and a small computer) and a conduction system (wires) through which impulses travel from the pulse generator to the heart muscle. Electrical cardioversion, anti-tachycardia pacing, defibrillation, catheter ablation, and cardiac surgery are also used. We do not treat arrhythmias with HAT medicine.
Leave your comment
- Comments
Comments
- No comments found
Pinned
Liked
Do cardiac arrhythmias manifest themselves in the same way?
All rhythm and conduction disorders clinically manifest themselves differently in different patients. Some patients do not feel any symptoms and learn about the pathology only after a scheduled ECG. This proportion of patients is insignificant, since in most cases patients note obvious symptoms.
Thus, rhythm disturbances accompanied by rapid heartbeat (from 100 to 200 beats per minute), especially paroxysmal forms, are characterized by a sharp sudden onset and interruptions in the heart, lack of air, pain in the sternum.
Some conduction disorders, such as fascicular blocks, do not show any signs and are recognized only on an ECG. Sinoatrial and atrioventricular blockades of the first degree occur with a slight decrease in heart rate (50-55 per minute), which is why clinically they can manifest only slight weakness and increased fatigue.
Blockades of the 2nd and 3rd degrees are manifested by severe bradycardia (less than 30-40 per minute) and are characterized by short-term attacks of loss of consciousness.
In addition, any of the listed conditions may be accompanied by a general severe condition with cold sweat, intense pain in the left half of the chest, decreased blood pressure, general weakness and loss of consciousness. These symptoms are caused by impaired cardiac hemodynamics and require close attention from a doctor.
How to make a diagnosis?
Types of arrhythmias
Most people by arrhythmia mean erratic contractions of the heart muscle (“the heart beats as it wants”). However, this is not quite true. The doctor uses this term for any disturbance of cardiac activity (decreased or increased heart rate), so the types of arrhythmias can be presented as follows:
- Sinus arrhythmia, which may be associated with cycles of respiratory activity (increased rhythm during inhalation and slower rate during exhalation) or occur independently of breathing, but indicate some kind of cardiovascular pathology (coronary artery disease in old age) or be a consequence of autonomic dysfunction, for example, in teenagers. This type of arrhythmia is harmless and does not require special treatment measures. The ECG shows a difference between cardiac cycles (> 0.05 s).
- Sinus tachycardia is diagnosed if the heart rate exceeds 90 beats/min, of course, for no apparent reason (running, exercise, excitement). Typically, with such tachycardia, the heart rate does not exceed 160 beats per minute under calm conditions, and only during intense exercise can it reach up to 200 beats. It is caused by many factors associated with pathological processes in the body, therefore the treatment of such tachycardia is aimed at the underlying disease.
- Sinus bradycardia is characterized by a regular but slow sinus rhythm (less than 60 beats/min), associated with a decrease in the automaticity of the sinus node and resulting from excessive physical exertion (in professional athletes), pathological changes (not necessarily cardiovascular, for example, peptic ulcer). ), taking certain medications (digitalis, antiarrhythmic and antihypertensive drugs). Therapy is also aimed at eliminating the cause that caused bradycardia, that is, the underlying disease.
- Extrasystoles that occur with premature excitation and contraction of one part of the heart or all of them at once, therefore, depending on where and in what place the impulse was formed that disrupted the normal sequence of heart contractions, extrasystoles are divided into atrial, ventricular and those coming from the atrioventricular node. Extrasystolic arrhythmia is dangerous if it is group, early and frequent, since it poses a threat to hemodynamics, and as a result can “develop” into ventricular tachycardia or ventricular fibrillation, which will have serious consequences. During myocardial infarction, extrasystolic arrhythmia is recorded in 100% of cases.
- Paroxysmal supraventricular (supraventricular) tachycardia, which develops suddenly and also suddenly stops, is characterized by a regular, strict rhythm, although the contraction frequency can reach 250 beats/min. Such tachycardias include: atrial tachycardia, AV nodal tachycardia and tachycardia with WPW syndrome.
- Arrhythmias associated with conduction disturbances (blockades) are usually well recorded on the ECG, are a companion and symptom of various pathologies and are treated by influencing the underlying disease. Blockades that quite often produce (sinoauricular and atrioventricular) bradycardia (40 beats per minute and below) are considered life-threatening and require the installation of a pacemaker that compensates for cardiac activity.
- Atrial fibrillation, in terms of frequency of occurrence, follows immediately after extrasystole and holds 2nd place in prevalence. It is characterized by the formation of excitation and contraction only in certain areas (fibers) of the atrium, when these processes are absent as a whole. Such chaotic and disorderly excitation of individual fibers prevents the passage of impulses into the atrioventricular node, as well as into the ventricles, to which single impulses nevertheless reach, causing excitation there that responds with random contractions.
Based on heart rate, there are 3 forms of atrial fibrillation:
- Heart rate less than 60 beats/min – bradysystolic;
- 60-100 beats/min – normosystolic;
- Heart rate exceeds 100 beats/min – tachysystolic.
On an ECG with AF, the P wave is not recorded because there is no excitation of the atria, and only atrial f waves are detected (frequency 350-700 per minute), which are characterized by irregularity, differences in shape and amplitude, which gives the electrocardiogram a unique appearance.
The cause of MA may be:
- Organic damage to the heart muscle;
- Age-related changes (coronary heart disease, often in combination with arterial hypertension);
- In young people: rheumatism, valve defects (mitral valve stenosis, aortic valve disease);
- Thyroid dysfunction;
- Congenital pathology (heart defects);
- Acute and chronic heart failure;
- Myocardial infarction;
- Acute cor pulmonale;
- Myocarditis, pericarditis;
- Cardiomyopathy.
The incidence of atrial flutter (AF) is 20-30 times lower than AF. It is also characterized by contractions of individual fibers, but a lower frequency of atrial waves (280-300 per minute). On the ECG, atrial waves have a greater amplitude than in AF.
It is interesting that on one ECG you can see the transition of flicker to flutter and vice versa.
The causes of atrial flutter are similar to the causes of fibrillation.
Symptoms of flickering and fluttering are often absent altogether, but sometimes there are some clinical manifestations caused by erratic activity of the heart or symptoms of the underlying disease. In general, such a pathology does not give a clear clinical picture.
Irregular heart rhythm (arrhythmia)
An irregular heartbeat is an arrhythmia (also called dysrhythmia). Your heart rate may also be irregular. The normal heart rate is from 50 to 100 beats per minute. Arrhythmia and abnormal heart rate do not necessarily occur simultaneously. Arrhythmia can occur against a background of a normal heart rate or even a slow rate (called bradyarrhythmia - less than 60 beats per minute). Arrhythmia can also occur against the background of an accelerated heart rate (called tachyarrhythmia - more than 100 beats per minute). In the United States, more than 850,000 people are hospitalized each year due to arrhythmias.
What causes arrhythmia?
Arrhythmia can occur due to many different factors, including:
- Cardiac ischemia.
- An imbalance of electrolytes in your blood (such as sodium or potassium).
- Changes in your heart muscle.
- Damage due to cardiac risk.
- Recovery processes after heart surgery.
Abnormal heart rhythms can also occur in a “normal healthy” heart.
What types of arrhythmias are there?
Arrhythmia is divided into the following types:
- Premature atrial contractions (extrasystoles).
These extrasystoles occur in the atria (upper chambers of the heart). They do not cause harm and do not require treatment.
- Ventricular extrasystole.
This is the most common type of arrhythmia and occurs in people with and without heart disease. We all feel those missed heartbeats sometimes. In some people, they occur due to stress, excess caffeine, nicotine, or too much exercise. But sometimes ventricular extrasystoles can occur due to heart disease or electrolyte imbalance. People who experience these episodes frequently and/or are bothered by associated symptoms should be evaluated by a cardiologist. However, for most people, ventricular premature beats do not cause harm and rarely require treatment.
- Atrial fibrillation.
This is a very common type of heart rhythm disorder in which the atria (upper chambers of the heart) contract incorrectly.
- Atrial flutter.
This arrhythmia occurs due to the impulse circulating too quickly through the atrium. Atrial flutter is usually more orderly and regular than atrial fibrillation. It most often occurs in people with heart disease and in the first week after heart surgery. Also, flutter often turns into atrial fibrillation.
- Paroxysmal supraventricular tachycardia (SVT).
This is a rapid heart rate, most often regular and comes from the upper parts of the ventricles. Paroxysmal SVT occurs and ends suddenly. SVT is divided into two main types: accessory bundle tachycardia and AV node re-entry tachycardia (see below).
- Tachycardias, the mechanism of which is associated with additional bundles.
An accelerated heart rate is associated with the presence of additional impulse pathways or connections between the atria and ventricles. The impulses travel along additional paths in the same way as along the normal path. This allows them to travel faster throughout the heart, causing the heart to beat faster.
- Tachycardia due to the mechanism
of re-entry of the AV node.
An accelerated heart rate occurs because there is more than one pathway passing through the AV node. This may lead to palpitations, fainting, or heart failure. In many cases, tachycardia can be controlled by a simple procedure, medication, or implantation of a pacemaker by a medical professional. - Ventricular tachycardia.
The accelerated heart rate comes from the lower parts of the heart (ventricles). It prevents the heart from filling adequately with blood, so the heart pumps less blood into the body. This arrhythmia can be severe, especially in people with heart disease, and may be associated with other symptoms. People with such arrhythmia should be seen by a cardiologist.
- Ventricular fibrillation.
This is a continuous, disorganized flow of impulses from the ventricles. The ventricles flutter, as a result of which they cannot contract and pump blood throughout the body. This is an emergency condition that requires treatment in the cardiopulmonary resuscitation department and defibrillation as soon as possible.
- Long QT syndrome.
The QT interval is an area on the electrocardiogram (ECG) that reflects the time the heart muscle spends contracting and then recovering, or the time it takes from the creation of an electrical impulse, its passage through the heart, to recharging. When the QT interval is longer than normal, it increases the risk of developing torsade de pointes, a life-threatening form of ventricular tachycardia. Long QT syndrome runs in families and can cause sudden cardiac death in young people. Treatments for this condition include antiarrhythmic drugs, pacemaker implantation, electrical cardioversion, defibrillation, implantable cardioverter/defibrillator implantation, or ablation.
- Bradyarrhythmias.
These are arrhythmias against the background of a slow heart rate caused by diseases of the electrical conduction system of the heart. For example, sinus node dysfunction and heart block.
- Sinus node dysfunction.
This is a slow heart rate that occurs due to problems in the sinoatrial (SA) node. To treat sinoatrial node dysfunction, a pacemaker is implanted.
Next »