Idioventricular rhythm - what is it?
Idioventricular rhythm appears when the muscle fibers of the heart begin to contract more actively, accelerated impulses lead to active contraction of the myocardium. Their frequency is faster than the normal rhythm - more than 40 beats per minute. This is caused by an imbalance or dysfunction of the autonomic system.
Gradually, pathological processes begin to occur in the human body - cell depolarization. They lose their activity and cease to support atrial contraction.
Idioventricular rhythm in adults and children indicates the development of trigger activity, ischemia, digitalis intoxication and other pathological processes in the heart, structural changes in muscle tissue. The first symptoms occur when an occluded coronary artery opens and extensive myocardial damage occurs.
How does the circadian rhythm work?
The main trigger element of the biological clock is the suprachiasmatic nucleus of the hypothalamus (SCN). When there is a change from light to darkness, the optic nerves give it a signal to release melatonin, the main sleep hormone.
From 12 at night, the concentration of melatonin begins to gradually increase, provided that not a single ray of light falls on the visual analyzer. By 4 am we get a peak in hormone synthesis. When the sun starts to rise, it starts to fall.
Melatonin plays a responsible role in our body; it:
— Is one of the main antioxidants;
— Promotes the inclusion of mechanisms of cellular apoptosis during cell mutation;
— Participates in neuroregulation;
— Models the activity of the reproductive system;
— Reduces emotional reactivity.
The main advantage of the biological clock is that during normal operation of circadian rhythms, human physiology adapts to changes in the environment. In the morning, metabolism, muscle mass, and body temperature increase, so the body prepares for its main activity. And at night, metabolic pathways, damaged areas of tissue and cells are restored, and an energy reserve is created. Circadian rhythms give humans a huge selective advantage in the struggle for existence.
Symptoms
Idioventricular rhythm is characterized by the following symptoms:
- heart rate decreases to 40 beats per minute;
- contractions become weak, the efficiency of the heart muscle decreases;
- a threadlike pulse is absent or faintly audible.
Diagnostics makes it possible to detect characteristic signs of idioventricular rhythm - clinical manifestations of arrhythmia, arrhythmic contraction of the atria. During an electrocardiogram, symptoms of a disrupted impulse of the sinus node of the heart are recorded. The ECG records the symptoms of deformed ventricular complexes and the output of the impulse from the sinus node.
Be sure to check the condition of the ventricular QRS complexes, which, in the presence of pathological processes, become deformed and the cavity becomes wide. During an ECG, active contractions of 0.12 seconds are diagnosed. As the idioventricular rhythm progresses, the frequency of RR scars increases to 35 beats per minute, and there are no R scars on the ECG diagram.
The essence of the phenomenon
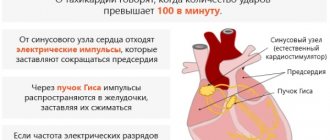
The transmission of nerve impulses to the heart of every healthy person occurs through the conduction system. The main generator of these impulses is the right atrium appendage, where the sinus node is located. Further, the path lies through the Purkinje fibers and the His bundle, through which the nerve impulse enters the fibers of the ventricles.
Conduction system of the heart
Despite the fact that such propagation of impulses ensures satisfactory functioning of the heart, there are conditions in which this becomes difficult. Various pathological processes in the body lead to the fact that the sinus node cannot cope with the initiation of excitation. Then the process of triggering impulses in the heart changes significantly.
The work of the heart, as the main muscle of the human body, must be preserved, and for this, rhythms arise that compensate for the weakened focus. These rhythms are called ectopic. The medical term “ectopia” translated from Greek means “displacement, change in the place of habitual residence.”
PEER
To determine where the nerve impulses come from and which area of the myocardium is currently triggering the heart rhythm, it is necessary to record an ECG. The ratio of the R waves to the ventricular QRS complexes determines how excitation moves through the atria.
Below are electrocardiographic criteria for different heart rate variations:
- Sinus. With it, characteristic H waves appear above the isoline in standard lead II before each QRS; all P waves are present in each lead, they are constant and do not differ in shape. All subsequent variants are non-sinus and, accordingly, represent a deviation from the norm.
Atrial. It comes from the underlying sections of the atria and is characterized by P waves located under the isoline and running in front of the entire ventricular complex; Each P is followed by a constant QRS complex.- Atrioventricular. The usual P waves do not appear on the ECG; they can join the unchanged QRS or be under the isoline, following the normal QRS complexes.
- Idioventricular rhythm. This is an extrasystolic rhythm from the ventricles. It is characterized by slow (less than 40 beats per minute) contraction of the ventricles; The electrocardiogram shows a widening of the QRS (more than 0.16 s) and deformation of the complexes; P waves occur regardless of the QRS complexes.
Provoking factors, causes
The following factors lead to the development of idioventricular rhythm:
- Myocarditis. An inflammatory process occurs in the chest area, which spreads to the heart muscle and affects it.
- Large-scale blood loss. Occurs with open limb injuries after surgery.
- Ischemic process. The pathology provokes a deficiency of oxygen supply to healthy myocardial fibers.
- Cardiosclerosis. When the disease occurs, the heart muscle becomes scarred. Damage to healthy tissue leads to subsequent death of muscle fiber cells.
- Cardiac tamponade. The disease leads to fluid gradually accumulating in the pericardial cavity, which subsequently provokes pinching of the heart and excessive compression.
- Myocardial infarction. This is a clinical manifestation of coronary heart disease, when blood flow to the heart muscles is disrupted or completely stopped. Pathological processes lead to the gradual death of cells.
- Pathologies of the thyroid gland. They are characterized by a lack of iron in the body. Provoking factors are genetic predisposition, when the disease is transmitted from one generation to another.
- Hormonal imbalance. It occurs when a person takes oral contraceptives for a long time. Negative factors - smoking, sudden weight loss, frequent stressful situations, overexertion.
- Intoxication of the body. Occurs when uncontrolled use of anesthetics, digoxin in the wrong dosage.
Idioventricular rhythm is the only disease that does not lead to other heart diseases. Impaired contractions appear as a result of necrotic processes in soft tissues and severe forms of pathological processes.
Classification
The following classification of ventricular rhythm is distinguished:
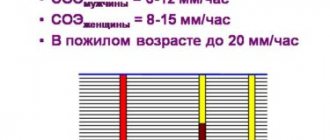
- By heart rate. Ventricular tachycardia develops when the heart rate decreases to 100 beats per minute.
- By analysis of the QRS complex. This pathology is characterized by a monomorphic rhythm (premature myocardial contractions).
- By period and time of reductions. More than 30 seconds per minute - stable tachycardia, more than 30 seconds - unstable tachycardia.
Idioventricular rhythm can be slow – when the heart rate decreases to less than 55 beats per minute. With a fast heart rate, the pulse exceeds 100 beats.
Cardiac arrhythmia - what is it and how to treat it? Make an appointment with a cardiologist at MEDSI Clinic
Table of contents
- Causes
- Classification
- Symptoms
- Arrhythmia during pregnancy
- Diagnostics
- Treatment
- Drug treatment of cardiac arrhythmia
- Cardiac arrhythmia: treatment with surgery
- Consequences
- Prevention
- Forecast
- Advantages of treatment at MEDSI
Cardiac arrhythmia
is a pathology associated with disturbances in the rhythm, frequency and sequence of heart contractions. The disease can be a consequence of both diseases of the heart itself and disturbances in the functioning of other organs and systems. Malfunctions of the heart are very dangerous, as they can cause both serious health problems and death of the patient. That is why treatment of arrhythmia should begin as early as possible, when the first attack occurs. You should not think that it is a one-off and will never happen again!
Causes
To the main causes of arrhythmia
heart problems include functional dysregulation and anatomical changes. Very often, rhythm disturbances are a sign of illness.
Arrhythmia can be provoked
:
- Coronary heart disease
- Injuries
- Surgical interventions
- Heart defects
- Myocarditis, etc.
There are also third-party (non-cardiac) factors that can cause rhythm disturbances.
These include:
- Addiction to drinks and foods containing large doses of caffeine
- Energy drink craze
- Excessive alcohol consumption
- Frequent smoking
- Stress
- Metabolic disorders
- Fungal infections
- Excessive exercise
- Infections
- Climax
- Brain pathologies
In most cases, the causes of cardiac arrhythmia are quickly identified, allowing treatment to begin immediately. In some situations, it is impossible to identify factors contributing to the development of pathology. Such conditions are called idiopathic.
Classification
Today, experts have identified several types of arrhythmias:
- Sinus tachycardia.
With this pathology, the heart rate is more than 90 beats per minute. The patient experiences unpleasant sensations; he literally feels how hard his heart is beating. Some call this condition “the heart is jumping out of the chest” - Sinus arrhythmia
. With this pathology, heart contractions alternate incorrectly. Typically this form of the disease is diagnosed in children and adolescents - Sinus bradycardia
. This pathology is characterized by a pulse rate of less than 55 beats per minute and can occur even in completely healthy people during sleep or rest. - Atrial fibrillation
. This pathology is characterized by a regular rhythm with a very rapid (up to 240 beats per minute) heartbeat. Patients suffer from weakness and increased sweating. Some patients become faint during an attack - Paroxysmal tachycardia
. With this pathology, the heart rate increases (up to 140-220 beats per minute). The attack begins suddenly and ends just as quickly - Extrasystole
. This pathology is characterized by premature contractions of the heart. During an attack, the patient feels freezing or tremors of the heart muscle
Symptoms
Symptoms of arrhythmia largely depend on its type and are determined by the rhythm and frequency of the heart.
To the main features
pathological conditions include:
- Feeling of heart failure
- Increased heart rate
- Weakness
- Dizziness
In some cases, attacks are accompanied by suffocation, fainting and general discomfort.
Important! In some cases, “silent” arrhythmias are diagnosed. With this pathology, the patient does not experience any symptoms. The disease is discovered accidentally, usually during an ECG examination during medical examination or diagnosis of other pathological conditions.
Arrhythmia during pregnancy
Pregnancy is a special state of the body, which is characterized by various changes in the functioning of both individual organs and entire systems. While carrying a child, a woman may experience heart rhythm disturbances. Almost 20% of pregnant women, for example, experience tachycardia and extrasystole. At the same time, we cannot talk about heart pathologies.
If you suffer from a disease, but still want to become a mother, you should:
- Strictly follow all doctor's recommendations
- Maintain a rest and work schedule
- Take all prescribed medications
- Receive inpatient therapy in a timely manner
Childbirth in women with arrhythmia usually takes place in specialized departments, where immediate assistance can be provided for cardiac pathologies.
Diagnostics
Diagnosis of cardiac arrhythmia, as well as treatment, is always carried out comprehensively.
The examination includes:
- Audition at the first appointment
- Taking an ECG
- Taking blood and urine tests
The initial examination allows us to determine the heart rhythm, the sequence and frequency of heart contractions, the general health of the patient, and the presence of factors that could trigger the development of the pathological condition.
If arrhythmia occurs spontaneously and does not depend on activity and time of day, Holter monitoring is performed. This technique involves recording the heartbeat around the clock using special equipment. Studies are also carried out under load (on a treadmill or other exercise machine).
To clarify the diagnosis and identify the causes of the pathology, other studies may be carried out.
These include:
- Ultrasound of the heart
- Dopplerography of blood vessels
- Echocardiography, etc.
If necessary, the patient is referred for consultation to other specialists (endocrinologist, gynecologist, etc.).
Treatment
Treatment of cardiac arrhythmia is always carried out in accordance with:
- The cause of the pathology
- A form of rhythm disturbance
- General condition of the patient
- Identified concomitant pathologies
In some cases, it is very important to correct the underlying disease. Only after this can therapy be carried out directly.
Drug treatment of cardiac arrhythmia
Therapy is carried out using drugs such as:
- Calcium and sodium channel blockers
- Beta blockers
- Vitamin complexes
- Means to improve the functioning of the entire cardiovascular system
Important! It is strictly forbidden to attempt therapy on your own! Arrhythmia, which is treated at home, can cause serious complications and even cause the death of the patient.
Cardiac arrhythmia: treatment with surgery
Operations are performed in cases where medication methods do not give the desired result, and in cases of pronounced changes in the functioning of the heart.
Today can be held:
- Cardiac pacing, which involves applying an electric current to the heart muscle
- Implantation of a special device to regulate heart rate
- Catheter ablation, in which sources of false impulses are cauterized and the heartbeat is normalized
Important! Treatment of cardiac arrhythmia, regardless of the cause, is carried out only by a cardiologist. Even standard medications are often selected under the supervision of a specialist. In severe cases, the selection of medications is carried out in a hospital setting. The patient's condition is constantly monitored, and numerous examinations are carried out regularly. This allows you to prevent deterioration in health and the occurrence of complications, and significantly reduces the risk of death of the patient.
Consequences
Any arrhythmia can be complicated by pathological conditions such as ventricular flutter and fibrillation
. These conditions are equivalent in severity to circulatory arrest and can lead to the death of the patient. In the very first seconds of the attack, weakness develops, and the patient experiences dizziness. Then he loses consciousness and convulsions occur. During an attack, breathing stops, and pulse and blood pressure are not recorded. Clinical death occurs. If resuscitation is not performed, the patient will die.
Complications of arrhythmia are especially dangerous for patients with chronic circulatory failure
. During an attack, the patient experiences shortness of breath and may develop pulmonary edema.
Thromboembolic complications are also common
associated with blockage of important arteries. Such conditions lead to cerebral stroke.
Prevention
To prevent arrhythmia it is necessary:
- Do regular morning exercises or simple sets of exercises throughout the day
- Stick to a proper diet. It is important to saturate the body with the full range of nutrients and eat a nutritious and varied diet. At the same time, you should avoid fried, salted and smoked foods, which place additional stress on the body.
- Maintain a normal weight
- Monitor your blood pressure levels
- To refuse from bad habits
- Track sugar levels
- Lead a calm lifestyle, avoiding stress
- Maintain a work and rest schedule
It is very important to regularly consult a doctor and undergo at least a minimal examination to determine the general condition of the body and existing risk factors for the development of pathological issues.
When the first signs of arrhythmia appear, you need to make an appointment with a cardiologist.
Forecast
Arrhythmias not associated with organic cardiac pathologies are not a threat to the health and life of the patient. The prognosis for them is always favorable. The patient can live with this form of the disease, often without even noticing it (if he follows all the doctor’s recommendations). Atrial fibrillation and a number of other forms are dangerous because they can provoke severe pathologies, including not only heart failure, but also stroke. Atrial flutter and ventricular fibrillation pose an immediate threat to life. The prognosis for such pathologies is the most unfavorable. In numerous cases, without proper medical supervision, the patient dies.
Advantages of treatment at MEDSI
- Qualified specialists. Our doctors (not only cardiologists) regularly undergo training and study new methods of treating arrhythmias
- Possibilities for quick diagnostics. We have our own laboratory, where test results can be obtained in CITO (urgent) mode. We also have modern equipment for instrumental diagnostics
- Opportunities for drug therapy and surgical interventions. Our specialists are ready to select means to stabilize the heart, allowing you to avoid relapses of the disease and complications. Our clinics also have operating rooms for performing endovascular interventions and installing pacemakers and defibrillators
- Using only proven methods and drugs. Treatment of arrhythmia in Moscow in our clinics is carried out using products that meet international standards and have proven their effectiveness
- Attentive attitude towards all patients
- Individual approach
- Comfortable atmosphere in clinics
To make an appointment with a cardiologist, just call +7 (495) 7-800-500. We will schedule you to see a specialist at a convenient time. You don't have to wait in line!
Clinical picture
The diagnosis is confirmed by the following data:
- The appearance of pain in the chest area, shortness of breath. These symptoms indicate the development of myocardial ischemia. The body changes the effects of reperfusion after coronary artery surgery.
- Peripheral edema, cyanosis. These symptoms relate to the development and progression of cardiomyopathy, myocarditis, and congenital heart defects.
- Changes in the intensity of the heart murmur. Irregular heart rhythm occurs when there is a competing sinus rhythm.
The clinical picture of idioventricular rhythm is associated with progression of hypotension, AV asynchrony, or high ventricular rate.
Diagnostics
The main method for determining a change in rhythm towards pathology is an electrocardiogram. Idioventricular rhythm is spoken of when the following signs appear on the ECG:
- Expansion (more than 0.12 s) and deformation of the ventricular QRS complexes, which is also observed during blockade of the His bundle and its branches.
Reducing the frequency of RR intervals to 30-40 per minute, because the ventricles are not able to contract with a greater amplitude.- Loss of P waves, which usually should be located above the isoline and recorded before the new ventricular complex.
- Unrelated and uncoordinated contraction of the atria and ventricles.
To clarify the diagnosis and rationally select therapy, the attending physician may need to prescribe additional examinations. The most commonly used are EchoCG and 24-hour Holter monitoring. In difficult cases, transesophageal ECG or echocardiography is used for diagnostic purposes.
Diagnosis of atrioventricular dissociation
Atrioventricular dissociation is diagnosed based on the ECG information obtained.
Differential diagnosis is carried out for the following pathologies:
- slow ventricular tachycardia;
- complete AV block;
- nodal rhythm with aberration;
- supraventricular tachycardia with aberration;
- slow atrioventricular tachycardia.
Accelerated idioventricular rhythm - contractions of the ventricular rhythm with wide QRS complexes, heart rate in the range of 40-130 beats per minute.
ECG with idioventricular rhythm. Example and transcript
On the ECG, the ventricular complexes are widened, are in a deformed state, and follow in their own rhythm ="700″ height="377″[/img]
Explanation: complete AV block with heart rate 37 beats per minute. The P-P interval is very low, therefore it indicates concomitant weak sinus node syndrome, combined with AV block.
Segments and waves of a normal ECG
Waves and intervals within the normal range:
- P – 0.05-0.25 mv;
- Q – 0.00-0.20 mv;
- R – 0.30-1.60 mv;
- S – 0.00-0.03 mv;
- T – 0.25-0.60 mv.
The ECG records cardiac activity in twelve leads - 6 from sensors located on the limbs, 6 chest leads. The P wave demonstrates the process of excitation, relaxation of the atria, Q and S – the depolarization phase of the interventricular septum. The R wave - displays the state of depolarization of the lower chambers of the heart, and T - the process of relaxation of the myocardium.
QRS complex waves
When studying the QRS complex, the duration of ventricular depolarization is monitored. The PR interval measures the time it takes for an electrical impulse to travel from the SA and AV nodes.
The QRS complex is the name for the combination of three graphical abnormalities that are observed on a typical electrocardiogram. They reflect the depolarization of the right and left ventricles, the degree of compression of the large ventricular muscle.
The normal value for adults is 0.06-0.10 seconds. In children and during physical activity, the indicator decreases to 0.05 seconds. The waves of the QRS complex alternate in rapid succession.
ECG analysis
When analyzing an electrocardiogram, the following indicators are considered:
- heart rate – normal value: not higher than 85 beats per minute;
- J-scar (in the absence of pathologies, it is absent);
- ST interval – (norm 320 milliseconds);
- RR interval is normally 0.6-1.2 seconds;
- PR interval – normal 120-120 milliseconds;
- QT interval is normally 420 milliseconds or less.
These are the norms for adults.
When analyzing an electrocardiogram for serious disorders, pathological processes are indicated by the following parameters:
- Sinus arrhythmia. Indicates the development of physiological disorders in the body.
- Sinus bradycardia. The pathology is characterized by heart contractions with a frequency of 50 beats per minute. In 45% of all cases, athletes are diagnosed.
- Extrasystole. A rhythm defect is associated with a chaotic contraction, a rare heartbeat. Characteristic symptoms of the pathology are discomfort in the chest area, tingling, sharp sensations of sudden fear and anxiety.
- Sinus tachycardia. With this pathology, the heart rate is more than 90 beats. Characteristic clinical manifestations are periodic increases in heart rate even at rest, with complete relaxation.
- WPW syndrome. This is a type of supraventricular tachycardia. Patients' heart rate and number increase. The main signs are a feeling of lack of air, periodic heart palpitations, increased heartbeat, fainting, shortness of breath, dizziness.
- Atrial fibrillation. As the disease progresses, the pathology is periodic and permanent. Patients complain of anxiety and panic attacks.
When analyzing electrocardiogram data, indicators such as segments, waves, and intervals are taken into account.
ECG interference
During the study of the electrocardiogram of the heart, the following interference may occur that interferes with the diagnosis of idioventricular rhythm on the ECG:
- Inrush currents. Characterized by regular vibrations, the frequency of which does not exceed 50 Hz. They correspond to the frequency of alternating electric current.
- Swimming. Interference occurs when there is poor contact between the electrode and the skin surface.
- Muscle tremors. The electrocardiogram displays frequent fluctuations of an irregular, uncharacteristic shape.
Interference interferes with the learning of segments, teeth, and intervals.
ECG diagnostics of dysfunctions of sinus node automatism, replacement complexes and rhythms
The sinus node (sinoauricular node, Keys–Flac node) (SU) is the normal pacemaker of the heart. Pacemaker cells of the SG (first order pacemaker) have the greatest automaticity; they generate 60–90 impulses per minute. Disorders of the automatism function of the SG can be divided into types that have and do not have hemodynamic significance, which, in turn, makes their timely and correct diagnosis extremely important, which makes it possible to prescribe adequate therapy and avoid (including iatrogenic) errors in the process treatment, to prevent the development of sudden death and other complications. Table 1 presents the classification of rhythm and conduction disorders [1–5].
According to the etiology, heart rhythm disturbances can be divided into the following main types: 1. Dysregulatory or functional: associated with disorders of neuroendocrine regulation, autonomic dysfunction, psychogenic influences, fatigue, reflex influences (gastritis, peptic ulcer, aerophagia, Roemheld syndrome, cholelithiasis, nephroptosis, urolithiasis, colitis, constipation, flatulence, pancreatitis, intervertebral hernia, embolism in the pulmonary artery system, mediastinal tumors, bronchopulmonary processes, pleural adhesions, chest surgery, genital diseases, skull injuries, brain tumors, multiple sclerosis). 2. Myogenic or organic: associated with myocardial diseases (cardiomyopathy, myocarditis, post-myocardial cardiosclerosis, myocardial dystrophy), with damage to cardiomyocytes that occurs against the background of coronary heart disease (myocardial infarction, ischemic cardiomyopathy), hypertension, heart defects. 3. Toxic: occurring under the influence of drugs (cardiac glycosides, anesthetics, tranquilizers, antidepressants, neuroleptics, aminophylline and its analogues, adrenomimetics (adrenaline, nor-adrenaline, mesaton, dobutamine, dopamine, salbutamol), acetylcholine, vagolytics (atropine), glucocorticosteroids, ACTH, antiarrhythmic drugs, cytostatics, antiviral drugs, antifungal drugs, antibiotics, diuretics, ether, alcohol, caffeine, nicotine, heavy metal salts, benzenes, carbon monoxide, mushroom poisoning, infections, endogenous intoxication in oncopathology, uremia, jaundice and etc. 4. Electrolytic: hypokalemia, hyperkalemia, hypocalcemia, hypercalcemia, hypomagnesemia 5. Dyshormonal: thyrotoxicosis, hypothyroidism, pheochromocytoma, puberty, menopause, pregnancy, hypopituitarism, ovarian dysfunction, premenstrual syndrome, tetany 6. Congenital: congenital atrioventricular (AV) conduction disorders, long QT syndrome, ventricular preexcitation syndromes (WPW, CLC, etc.). 7. Mechanical: cardiac catheterization, angiography, cardiac surgery, cardiac trauma. 8. Idiopathic. ECG diagnosis of arrhythmias caused by dysfunction of the automatism of the sinus node is carried out using an electrocardiographic study, which allows us to identify the following main types [1, 2, 4–16]. 1. Sinus tachycardia
– this is a regular rhythm with unchanged ECG waves (P wave, PQ interval, QRS complex and T wave do not differ from the norm) from the sinus node with a frequency of > 90 per minute. Sinus tachycardia at rest rarely exceeds 150–160 beats per minute (Fig. 1) [1, 16].
Differential diagnosis:
– supraventricular non-paroxysmal tachycardia;
– supraventricular paroxysmal tachycardia; – atrial flutter 2:1; – atrial fibrillation with ventricular tachysystole; – ventricular paroxysmal tachycardia. Etiology
: – physiological tachycardia: physical activity, emotions, fear, orthostatic, congenital features;
– neurogenic tachycardia: neurosis, neurocirculatory asthenia; – CVD: inflammatory and degenerative myocardial diseases, valve defects, collapse, heart failure, cor pulmonale, myocardial infarction, arterial hypertension; – drug and toxic tachycardia: vagolytics (atropine), sympathicotonics (adrenaline, norepinephrine, mesaton, dobutamine, dopamine), aminophylline, corticosteroids, ACTH, caffeine, coffee, tea, alcohol, nicotine; – infectious diseases: ARVI, sepsis, pneumonia, tuberculosis, etc.; – other: blood loss, anemia. 2. Sinus bradycardia
– slowing of the sinus rhythm with heart rate < 60 per minute due to reduced automaticity of the sinus node. Sinus bradycardia with a heart rate <40 beats per minute is rare (Fig. 2) [1, 16].
Differential diagnosis:
– AV block II stage.
2:1 or 3:1; – AV block, stage III; – atrial rhythms; – nodal rhythm; – atrial fibrillation with ventricular bradysystole, Frederick’s syndrome; – atrial flutter with conduction 4:1, 5:1; – SA blockade, SA failure; - atrial extrasystole. Etiology
: – physiological bradycardia: constitutional, in athletes and people engaged in physical work, during sleep, during vagal tests (pressure on the eyeballs, solar plexus and carotid sinus, Valsalva test), during breath holding, sometimes with fear, emotions , in the second half of pregnancy, with vomiting and hypothermia;
– extracardial vagal bradycardia: neurosis with vagotonia, depression, peptic ulcer, increased intracranial pressure with cerebral edema, meningitis, brain tumor, cerebral hemorrhage, labyrinth diseases, Meniere’s syndrome, hypersensitive carotid sinus, shock, increased blood pressure, vago-vagal reflexes for renal, biliary, gastric and intestinal colic, intestinal obstruction, myxedema, hypopituitarism; – drug and toxic bradycardia: cardiac glycosides (digoxin, strophanthin), opiates, acetylcholine, quinidine, beta blockers, cordarone, sotalol, calcium antagonists, anesthetics, tranquilizers, antipsychotics, pilocarpine. Uremia, jaundice, mushroom poisoning, hyperkalemia; – infectious diseases: viral infections (viral hepatitis, influenza), typhoid fever, diphtheria, cholera; – CVD: ischemic heart disease, diphtheria myocarditis, rheumatism, cardiomyopathies. 3. Sinus arrhythmia
– irregular activity of the sinus system, leading to alternating periods of increased and decreased rhythm.
There are respiratory and non-respiratory sinus arrhythmia [1, 16]. With respiratory sinus arrhythmia, the heart rate gradually increases when inhaling, and slows down when exhaling. Non-respiratory sinus arrhythmia persists during breath-holding and is not associated with the phases of breathing. Non-respiratory sinus arrhythmia, in turn, is divided into 2 forms: periodic (periodic, gradual alternation of acceleration and deceleration of cardiac activity) and aperiodic (lack of gradual alternation of phases of acceleration and deceleration of cardiac activity) (Fig. 3). Etiology
: – physiological arrhythmia: adolescents, elderly people;
– extracardiac diseases: infectious diseases, temperature reactions, obesity, pleuro-pericardial adhesions, increased intracranial pressure; – CVD: rheumatism, ischemic heart disease, heart defects, heart failure; – drug and toxic arrhythmia: opiates, cardiac glycosides, vagotonics. Differential diagnosis:
– AV block II stage;
– SA blockade, SA failure; – migration of the pacemaker through the atria; – atrial fibrillation; – atrial flutter (irregular shape); - atrial extrasystole. 4. Stopping the control system
(failure of the control system, sinus arrest, sinus pause, sinus-inertio) – periodic loss of the control system’s ability to generate impulses. This leads to loss of excitation and contraction of the atria and ventricles [1, 16, 17]. There is a long pause on the ECG, during which the PQRST waves are not recorded and the isoline is recorded. The pause when stopping the ultrasound is not a multiple of 1 RR (PP) interval (Fig. 4).
Etiology
: – reflex: sensitive carotid sinus, vagal tests;
– medicinal and toxic arrest of sinusitis: cardiac glycosides (digoxin, strophanthin), opiates, acetylcholine, quinidine, beta blockers, calcium antagonists. Hypokalemia, intoxication; – CVD: coronary artery disease, myocarditis, cardiomyopathies, surgical damage to the sinus, weakness of the sinus. Differential diagnosis:
– AV block II-III stage;
– blocked atrial extrasystoles; – SA blockade, stage II; – atrial fibrillation with ventricular bradysystole, Frederick’s syndrome; – nodal rhythm; – sinus arrhythmia; – sinus bradycardia; – atrial asystole. 5. Atrial asystole
(partial asystole) – absence of atrial excitation, which is observed during 1 or (more often) more cardiac cycles [1, 12, 16]. Atrial asystole can be combined with ventricular asystole, in such cases complete cardiac asystole occurs. However, during atrial asystole, pacemakers of the II, III, IV order usually begin to function, which cause excitation of the ventricles (Fig. 5).
Etiology
: – reflex: sensitive carotid sinus, vagal tests, intubation, deep breathing, due to irritation of the pharynx;
– medicinal and toxic: cardiac glycosides (digoxin, strophanthin), opiates, acetylcholine, quinidine, beta blockers, calcium antagonists. Hyperkalemia, intoxication, hypoxemia; – CVD: ischemic heart disease, myocarditis, cardiomyopathies, surgical damage to the sinus, weakness of the sinus, terminal cardiac condition. Differential diagnosis:
– AV block II-III stage;
– SA blockade, stage II; – blocked atrial extrasystoles; – atrial fibrillation with ventricular bradysystole; – Frederick's syndrome; – nodal rhythm; – sinus arrhythmia, sinus bradycardia; – SU stop. 6. Sick sinus syndrome
(SSNS) (sinus sinus syndrome dysfunction, bradycardia and tachycardia syndrome, sick sinus syndrome, Short syndrome, sick sinus syndrome, lazy sinus syndrome, sluggish sinus syndrome) is the presence of one or more of the following signs [1, 3–5 , 11, 12, 16, 17]: – persistent severe sinus bradycardia (Fig. 2); – the minimum heart rate determined during daily ECG monitoring for 1 day is <40 per 1 min, and its increase during physical activity does not exceed 90 per 1 min; – bradysystolic form of atrial fibrillation; – migration of the atrial pacemaker (Fig. 12); – stopping the SU and replacing it with other ectopic rhythms (Fig. 6–10, 13); – sinoauricular block; – pauses >2.5 s that occur as a result of the arrest of the sinus system, SA blockade, or rare replacement rhythms (Fig. 6);
– tachy-brady syndrome, alternating periods of tachycardia and bradycardia (Fig. 6); – rarely attacks of ventricular tachycardia and/or ventricular fibrillation; – slow and unstable restoration of the function of the suture system after extrasystoles, paroxysms of tachycardia and fibrillation, as well as at the moment of termination of stimulation during electrophysiological examination of the heart (post-tachycardial pause, which normally does not exceed 1.5 s, in case of suction systolic systolic activity can reach 4–5 s); – inadequate reduction in rhythm when using even small doses of beta blockers. Presence of bradycardia during the administration of atropine and exercise testing.
Classification
There is no unified classification of SSSU.
Depending on the nature of the lesion, true (organic), regulatory (vagal), medicinal (toxic) and idiopathic SSS are distinguished (Fig. 6). According to clinical manifestations, the following are distinguished:
– latent SSSU: there are no changes on the ECG, and the pathology of the SS is detected by additional functional research methods (EFI);
– compensated SSSU: no clinical changes, there are changes on the ECG; – decompensated SSSU: there are clinical and ECG manifestations of the disease. Based on ECG signs, the following are distinguished: – bradyarrhythmic variant of SSSS. – tachycardia-bradycardia syndrome. Etiology
: – CVD: ischemic heart disease, myocarditis, cardiomyopathies, surgical damage to the sinus, rheumatism, congenital defects; – reflex: sensitive carotid sinus, vagal tests, reflex effects in peptic ulcers, cholelithiasis, hiatal hernia; – medicinal and toxic: cardiac glycosides (digoxin, strophanthin), opiates, acetylcholine, quinidine, beta blockers, calcium antagonists. Hyperkalemia, intoxication, hypoxemia; – idiopathic forms.
Passive ectopic complexes and rhythms
Reduced activity of the sinus sinus or complete blockade of sinus impulses due to functional or organic damage to the sinus system causes the activation of automatic centers of the second order (cells of atrial pacemakers, AV connection), third order (His system) and fourth order (Purkinje fibers, ventricular musculature).
Automatic centers of the second order produce unchanged ventricular complexes (supraventricular type), while centers of the third and fourth order generate dilated and deformed ventricular complexes (ventricular, idioventricular type). The following rhythm disturbances have a substitutive nature: atrial, nodal, migration of the pacemaker through the atria, ventricular (idioventricular rhythm), jumping contractions [1, 5, 16]. 7. Atrial rhythm
(slow atrial rhythm) - a very slow ectopic rhythm with foci of impulse generation in the atria (Table 2).
Right atrial ectopic rhythm is the rhythm of an ectopic focus located in the right atrium. The ECG shows a negative P wave in leads V1-V6, II, III, aVF. The PQ interval is of normal duration, the QRST complex is not changed. Coronary sinus rhythm (coronary sinus rhythm) - impulses to excite the heart come from cells located in the lower part of the right atrium and the coronary sinus vein. The impulse propagates through the atria retrogradely from bottom to top. This leads to the registration of negative P waves in leads II, III, aVF. The PaVR wave is positive. In leads V1-V6 the P wave is positive or 2-phase. The PQ interval is shortened and typically <0.12 s. The QRST complex is unchanged. The coronary sinus rhythm may differ from the right atrial ectopic rhythm only by shortening the PQ interval. Left atrial ectopic rhythm - impulses to excite the heart come from the left atrium. In this case, a negative P wave is recorded on the ECG in leads II, III, aVF, V3-V6. The appearance of negative P waves in I, aVL is also possible; the P wave in aVR is positive. A characteristic sign of left atrial rhythm is the P wave in lead V1 with an initial rounded dome-shaped part, followed by a pointed peak - “shield and sword” (“dome and spire”, “bow and arrow”). The P wave precedes the QRS complex with a normal PR interval of 0.12–0.2 s. Atrial rate is 60–100 per minute, rarely <60 (45–59) per minute or >100 (101–120) per minute. The rhythm is correct, the QRS complex is not changed (Fig. 7).
Regular rhythm with a negative wave PI, II, III, aVF, V3-V6 before the QRS complex. The P wave in lead V1 has an initial rounded dome-shaped portion followed by a pointed peak—a “shield and sword.” Normal PR interval = 0.12-0.2 s. Inferior atrial ectopic rhythm is the rhythm of an ectopic focus located in the lower parts of the right or left atria. This leads to the registration of negative P waves in leads II, III, aVF and a positive P wave in aVR. The PQ interval is shortened (Fig. 8). Differential diagnosis:
– sinus arrhythmia;
– nodal rhythm; – migration of the pacemaker through the atria; – atrial flutter; – polytopic atrial extrasystole; – atrial rhythms (right atrial, left atrial, lower atrial, coronary sinus rhythm). 8. Nodal rhythm
(AV rhythm, replacing AV nodal rhythm) - heart rhythm under the influence of impulses from the AV junction with a frequency of 40–60 per minute. There are 2 main types of AV rhythm [1]: – junctional rhythm with simultaneous excitation of the atria and ventricles (junctional rhythm without P wave, junctional rhythm with AV dissociation without P wave): the ECG shows an unchanged or slightly deformed QRST complex, P wave absent (Fig. 9);
– junctional rhythm with different-time excitation of the ventricles and then the atria (junctional rhythm with a retrograde P wave, isolated form of the AV rhythm): an unchanged QRST complex is recorded on the ECG, followed by a negative P wave (Fig. 10).
Differential diagnosis:
– sinus bradycardia;
– atrial rhythm; – migration of the pacemaker through the atria; – polytopic atrial extrasystole; – idioventricular rhythm. 9. Migration of the pacemaker through the atria
(wandering rhythm, sliding rhythm, migrating rhythm, migration of the cardiac pacemaker, wandering pacemaker). There are several variants of the wandering (wandering) rhythm [1, 5,15]: Wandering rhythm in the SU. The P wave is of sinus origin (positive in II, III, aVF), but its shape changes with different heart contractions. The PR interval remains relatively constant. Severe sinus arrhythmia is always present. Wandering rhythm in the atria. The P wave is positive in II, III, aVF, its shape and size change with different heart contractions. Along with this, the duration of the PR interval changes. Wandering rhythm between the sinus and atrioventricular nodes. This is the most common variant of the wandering rhythm. With it, the heart contracts under the influence of impulses that periodically change their location: they gradually move from the suture block, atrial muscles to the AV junction and return to the suture block again. ECG criteria for pacemaker migration in the atria are ≥ 3 different P waves in a series of cardiac cycles, a change in the duration of the PR interval. The QRS complex does not change (Fig. 11, 12).
Etiology
: – reflex: healthy people with vagotonia, sensitive carotid sinus, vagal tests, intubation, deep breathing;
– medicinal and toxic effects: cardiac glycosides (digoxin, strophanthin), quinidine. Infectious diseases, intoxication; – CVD: ischemic heart disease, rheumatism, heart defects, heart surgery. Differential diagnosis:
– SA blockade II degree, failure of the SA;
– AV block II stage; – atrial fibrillation; – sinus arrhythmia; – polytopic atrial extrasystole. 10. Idioventricular (ventricular) rhythm
(intrinsic ventricular rhythm, ventricular automatism, intraventricular rhythm) - ventricular contraction impulses arise in the ventricles themselves. ECG criteria: widened and deformed QRS complex (>0.12 s), rhythm with heart rate < 40 per 1 min (20–30 per 1 min). Terminal idioventricular rhythm is very slow and unstable. The rhythm is often correct, but may be incorrect if there are several ectopic foci in the ventricles or the presence of one foci with varying degrees of impulse formation or exit block. If an atrial rhythm is present (sinus rhythm, atrial fibrillation/flutter, ectopic atrial rhythm), it is independent of the ventricular rhythm (AV dissociation) (Fig. 13, 14) [1, 5, 16, 17].
Differential diagnosis:
– AV block, stage III;
– SA blockade II-III stage; – atrial fibrillation with ventricular bradysystole, Frederick’s syndrome; – nodal rhythm; – sinus bradycardia; – jumping contractions. Etiology
: – medicinal and toxic effects: cardiac glycosides (digoxin, strophanthin), quinidine.
Infectious diseases, intoxication; – CVD: ischemic heart disease, myocarditis, cardiomyopathies, surgical damage to the sinus, weakness of the sinus, terminal cardiac condition. 11. Jumping contractions
(replacement systoles, escape systoles, ersatzsystolen, echappements ventriculaires, individual automatic contractions of the ventricles) - single impulses from the AV junction or ventricles. The difference between jumping contractions and nodal or idioventricular rhythm is the absence of a long period of contractions [1, 16]. Nodal jump-out contractions (the QRS complex is not changed and is the same in shape as the rest of the ventricular complexes. A jump-out contraction can be recognized by the position of the negative P wave or its absence) (Fig. 15). Ventricular jump contractions (the QRS complex is deformed and widened) (Fig. 16).
ECG criteria: the RR interval before the jumping contraction is always longer than 1 whole interval, and not shortened, as with extrasystole. The RR interval after the pop-up contraction is of normal length, rather than lengthened as with extrasystole, and in all cases shorter than the interval preceding the pop-up contraction. Etiology
: – medicinal and toxic effects: cardiac glycosides (digoxin, strophanthin), quinidine.
Infectious diseases, intoxication; – CVD: ischemic heart disease, myocarditis, cardiomyopathies, surgical damage to the sinus, weakness of the sinus, terminal cardiac condition. Differential diagnosis: – sinus arrhythmia;
– atrial extrasystole; – ventricular extrasystole; – migration of the atrial pacemaker; – SA blockade, stage II, failure of the SU; – AV block II stage; – nodal rhythm; – idioventricular rhythm.
Conclusion
The variety of dysfunctions of the automatism function of the control system significantly complicates their diagnosis. Nevertheless, the relevance of adequate assessment of SU dysfunction is beyond doubt.
AV dissociation
AV dissociation is a condition in which the ventricles and atria do not work synchronously. Contractions occur in a chaotic manner in the body. The rhythm of contractions of the ventricles coincides with the rhythm of contractions of the atria. Atrioventricular arrhythmia occurs with heart disease - myocardium, ischemic disease.
AV dissociation is a benign phenomenon. A common complication is the development of pathological cardiac arrhythmia.
Causes of AV dissociation:
- in the dominant pacemaker or sinus node, impulse formation slows down;
- acceleration of nodal or ventricular rhythm;
- pathological processes in the sinus node;
- vagal activity and neurocardiogenic syncope;
- ventricular pacing and tachycardia;
- myocardial infarction, structural heart disease.
As AV dissociation progresses, patients complain of shortness of breath even with slight exertion, dizziness, a feeling of strong pulsation in the body, increased heart rate, and fatigue.
Circadian rhythm of sleep
In addition to the above functions, melatonin at night activates or, conversely, suppresses the work of other hormones. For example, the production of prolactin, cortisol, and growth hormone is suspended. But if the optic nerve detects even the slightest glimpse of light, then the hypothalamus urgently stops the production of melatonin and all processes of the circadian rhythm are abruptly stopped. Thus, biological ri are “turned off” with the help of light.
They work best when we go to bed before midnight. Thanks to night sleep, the human body carries out the most important processes:
- Cerebrospinal fluid removes toxic compounds;
- The myelin sheaths necessary for transmitting signals between neurons are restored;
- Defense mechanisms are restored.
AV dissociation with interference
AV dissociation with interference is a syndrome of weakness or dysfunction of the sinus node. With this pathological process, a decrease or complete absence of the sinus node occurs. Characteristic signs are the appearance of severe sinus bradycardia, which leads to ischemia of the heart and muscles.
Idioventricular rhythm on ECG
This form of dissociation with interference can be persistent or transient. The pathological process develops as a result of infarction of the posterior diaphragmatic wall, myocarditis, progression of cardiosclerosis, and cardiomyopathy.
Violations
Ignoring biological rhythms disrupts the harmony of vital processes, which leads to the following consequences:
— Emotional tension is not relieved, which is the main generator for stress.
— The risk of neuropsychiatric disorders increases.
— The processes of free radical damage are intensified.
— Cell membranes are damaged.
- Metabolism is disrupted.
— Plasma leptin levels decrease, and glucose and insulin levels increase.
— Shifts occur in the endocrine system.
Also, studies on rodents have shown that disruption of circadian rhythm genes affects the early manifestation of “senile” diseases and illnesses, reduces the efficiency of the immune system and even reduces life expectancy.
Even after one day of failure of the biological clock, we become lethargic, incapacitated, feel constant fatigue and decreased attention and concentration. As a result, we wake up tired and unprepared for serious intellectual work.
The main enemies of circadian rhythms are artificial light sources, night work or lifestyle, and jet lag.
Features in children
Idioventricular rhythm is diagnosed in children during the first 10 days after birth. The pathology is transient in nature. In 9% of children, the pathology develops into a stable pathological process.
At older ages, after 8 years, the following forms of pathology are diagnosed:
- 4% of patients have sinus bradycardia;
- 10% of children were diagnosed with ectopic atrioventricular rhythm;
- in 12% of all cases, pacemaker migration or atrial extrasystoles are detected.
Idioventricular rhythm in children occurs due to organic damage to the heart - congenital malformations, degenerative processes, inflammatory processes in the myocardium, tumors of various etiologies in the heart. Pathology occurs during metabolic changes when hypo or hyperthermia is present.
Methods of therapy, treatment and recommendations of doctors
Methods of therapy for treating patients diagnosed with idioventricular rhythm - prescribing medications, performing ablation.
Drug therapy
The drugs that are most often prescribed to patients for heart rhythm disturbances are presented in the table:
| A drug | Purpose |
| Amiodarone | The drug is administered intravenously - into a central vein or as a bolus. Dosage: 150-300 mg over 20 minutes in case of emergency. For long-term therapy, 200 mg of the drug is prescribed daily. The treatment period is 14 days. |
| Digoxin | The drug is administered intravenously. For emergency treatment, 0.25 mg every 2 hours is indicated for the first 2-3 days. As maintenance treatment, no more than 0.375 mg per day is prescribed. |
| Metoprolol | The drug is indicated for emergency treatment at a dosage of 5 mg intravenously every 5-10 minutes. The total dosage is not more than 15 mg. As maintenance therapy, 100-200 mg is prescribed during the day. |
Antiarrhythmic drugs exhibit proarrhythmic effects. Their effect is aimed at restoring supraventricular or ventricular rhythm. Treatment with these drugs is prescribed to patients with severe coronary disease, organic disorder, and hypokalemia.
Invasive techniques (surgical procedures)
Effective invasive methods include:
- Percutaneous ablation. A catheter is inserted into the heart muscle. With its help, the doctor isolates the pulmonary veins, which lead to an increase in the frequency of impulses.
- Implantation of a cardioveterar defibrillator. This is an automatic device that helps restore normal heart rhythm. It can be programmed for each patient so that the defibrillator will perform antiarrhythmic stimulation of the heart.
After the invasive procedure, patients are hospitalized for inpatient recovery.
Emergency care and resuscitation
Emergency care is provided to patients who have a frequent idioventricular rhythm, which is combined with atrial dysfunction, tachycardia. Doctors advise calling an ambulance if you experience pressing or acute pain in the heart area.
Before their arrival, you need to take a horizontal position. To provide first emergency care, a solution of potassium chloride at a concentration of 4% or novocainamide (10%) is administered to the patient. Improvement in well-being is observed after 15 minutes. After hospitalization on the first day, patients are shown the drug Adenosine. It is administered at a dosage of 6 mg every 2 hours. The medicine is not intended for long-term therapy.
Idioventricular rhythm requires treatment, because during a pathological process in the heart, a disruption of the normal rhythm of myocardial contractions occurs. Lack of therapy leads to a worsening of the situation, the appearance of symptoms of tachycardia and shortness of breath.
To prevent the occurrence of idioventricular rhythm, you need to stop smoking, abuse alcoholic beverages, and eat well and properly. You should visit a cardiologist at least once a year. Diagnostics allows timely detection of idioventricular rhythm deviations on the ECG.
Heart rhythm disturbances
Heart rhythm disturbances are based on a change in the conditions for the formation of excitation of the heart muscle or an anomaly in the paths of its propagation. Arrhythmias can be caused by both functional disorders and severe organic lesions of the heart. In some cases, the cause of heart rhythm disturbances is the congenital characteristics of the conduction system of the heart. The state of the nervous system plays a certain role in the occurrence of arrhythmia. For example, mental and emotional stress causes changes in the pace, and often in the rhythm, of heart contractions, including in healthy people. Arrhythmia often occurs in people with diseases of the central and autonomic nervous system.
Various diseases, accompanied by a violation of the anatomical structure of the heart or the metabolic processes occurring in it, cause types of arrhythmia of different duration and nature, and only a doctor can make a diagnosis, whose conclusions are based on clinical and electrocardiographic data.
Symptoms of arrhythmias
Quite often, patients do not feel the presence of arrhythmias. In these cases, arrhythmia is detected during a routine clinical examination. However, many patients experience a variety of sensations in the chest, which most often include:
- feeling of palpitations and chest pains;
- very rapid heartbeat;
- extremely slow heartbeat (“fading” of the heart);
- chest pain;
- dizziness;
- loss of consciousness or a feeling close to fainting.
Classification of arrhythmias
1. Automatic disorders:
a) nomotopic (pacemaker - in the sinus node):
- sinus tachycardia;
- sinus bradycardia;
- sinus arrhythmia;
- sick sinus syndrome (SSNS).
b) heterotopic (pacemaker - outside the sinus node):
- lower atrial rhythm;
- atrioventricular rhythm;
- idioventricular rhythm.
2. Excitability disorders:
a) extrasystoles:
- by source: atrial, atrioventricular, ventricular;
- by number of sources: monotopic, polytopic;
- by time of occurrence: early, interpolated, late;
- by frequency: single (up to 5 per minute), multiple (more than 5 per minute), paired, group;
- according to order: disordered, allorhythms (bigeminy, trigeminy, quadrigeminy).
b) paroxysmal tachycardia (atrial, AV, ventricular)
3. Conduction disorders
:
a) increased conductivity (WPW syndrome); b) decreased conductivity (blockades: sinoauricular, intraatrial, AV, bundle branch block).
4. Mixed (atrial flutter/fibrillation, ventricular fibrillation)
Diagnostics
ECG is the main method for diagnosing arrhythmias. However, it is not always possible to detect arrhythmia when taking a resting ECG. In such cases, the K+31 clinic performs 24-hour ECG monitoring (Holter monitoring). Some arrhythmias are provoked by physical activity; in such cases, stress tests (treadmill) are used to diagnose them.
Complications
A number of rhythm disturbances can lead to the development of severe complications. If the rhythm of contractions in the heart is abnormal, blood flow slows down, which leads to the formation of blood clots in the atria. In the absence of adequate therapy, these blood clots can spread through the bloodstream throughout the body, leading to blockage of the arteries of the brain (stroke), intestinal arteries, and lower extremities. Long-term existence of uncorrectable arrhythmia often leads to the development of heart failure.
Treatment of arrhythmias
- if arrhythmia is a consequence of any disease (for example, thyrotoxicosis), our doctors treat the underlying disease;
- antiarrhythmic drugs are prescribed (affecting the conduction system of the heart, as well as various ion channels).
To prevent the development of complications, dynamic monitoring of the patient by a cardiologist is recommended, even during the period of remission.