Blood test for total protein
Determining the concentration of proteins in plasma provides important information about the general state of health, the functioning of vital organs and the course of pathological processes. The analysis is carried out as part of a biochemical blood test, which also includes cholesterol, liver function tests, kidney function tests and glucose (measured in mmol/l)¹.
Blood proteins are a special buffer system that maintains the acid-base balance of the plasma in an optimal state - pH 7.37-7.43.² They also affect the viscosity and coagulability of the blood.
In biochemical analysis, the indicator is designated as total protein in the blood (T-Prot) or Total Protein. The laboratory result is given in grams per liter (g/l). In a detailed study, the quantity and percentage of different protein fractions (proteinogram)² are calculated. For analysis, blood is taken from the cubital vein or the vein on the back of the hand.
Proteins account for 6.5-8.5% of the total dry residue of plasma (9-10%)¹. Concentration depends on the rate of their synthesis and destruction, as well as the volume of distribution in bodily fluids and tissues. The indicator may change during the day, after physical activity and a large meal.
Patients are referred for analysis by a therapist or doctor of any other specialty, since total protein is not a specific indicator. Protein metabolism disorders occur with any inflammation, infections, diseases of internal organs and oncology. In rare cases, patients have congenital disorders of protein production.
To test for total protein, blood is taken from the cubital vein. Photo: tridsanu1984 / freepik.com
Indications for analysis
A study of total protein in the blood may be prescribed for the following indications³:
- general clinical medical examination;
- primary search for pathology of metabolic processes (metabolism);
- unexplained weight loss;
- swelling of the limbs, face;
- fatigue and severe weakness that does not correspond to the load;
- unexplained shortness of breath;
- the appearance of complaints from the liver or kidneys: chronic fatigue, arterial hypertension, increased abdominal volume due to intra-abdominal fluid, jaundice, pale skin, changes in the daily pattern of urination;
- eating problems, including eating disorders (anorexia, bulimia);
- suspicion of pregnancy;
- presence of signs of exhaustion;
- preventive examination for athletes, workers in heavy industries;
- monitoring the treatment or progress of diseases of internal organs;
- preparation for any surgical intervention.
Testing for total protein in the blood is the first step in diagnosing many diseases of internal organs and metabolic disorders. If the values deviate, the patient is referred for clarifying tests: determination of albumin or all protein fractions (proteinogram), leukocyte formula, erythrocyte sedimentation rate (ESR), hematocrit².
Table of norms by trimester
| Dates of pregnancy | Indicator as a percentage |
| First trimester | from 78 to 121 |
| Second trimester | from 83 to 133 |
| Third trimester | from 67 to 135 |
What are the dangers of low protein C in the blood of a pregnant woman? The development of deep vein thrombosis in the legs is a fairly common occurrence for pregnant women. A decrease in protein increases the risk of developing blood clots by 10 times.
A deficiency of cells can cause a serious condition in newborns called purpura fulminans, which is the formation of clots that block small blood vessels. This disease often ends in death. This is why regular monitoring during pregnancy is so important.
Preparing for analysis
A visit to the laboratory must be planned in advance, since the informativeness of the laboratory report depends on the quality of preparation. The following rules must be observed the day before:
- the day before the study, give up alcoholic beverages, heavy physical activity and stop taking medications (after consultation with your doctor);
- 2-3 days before the test, limit the consumption of fatty foods, smoked foods, pickles, and confectionery;
- do not visit baths, saunas, or solariums for several days before the procedure, and the day before replace the hot bath with a hygienic shower;
- do not smoke for 3 hours before donating blood, avoid psycho-emotional overload;
- 15 minutes before donating blood, you need to calm down and relax;
- the last meal in 12 hours - the night before in the form of a light dinner;
- In the morning you can only drink water (even juices and chewing gum are prohibited).
Important!
Total protein in the blood is the sum of all proteins. May show false results if improperly prepared, dehydrated, or after physical activity. It also does not provide information about isolated changes in the ratio of different fractions - albumins, globulins³.
The following factors also influence protein content³:
- pharmaceuticals containing sex hormones (testosterone, estrogens, oral contraceptives), phenothiazines;
- high physical activity can temporarily increase concentration by up to 10%;
- dietary patterns (for example, vegetarians who do not take special nutritional supplements have fewer circulating proteins in the serum);
- pregnancy;
- environment - people who live in warm countries have more immunoglobulins than residents of cold climates;
- damage to internal organs leads to massive loss of the protein part;
- change in circulating blood volume;
- any inflammation;
- improper storage of reagents and biological material;
- error of a specific research method;
- method of collecting material - long-term application of a tourniquet before taking blood from a vein increases the amount of protein in the serum.
Plasma protein concentrations are variable and change rapidly during the day under the influence of external factors. It increases by 10-20% if you stand up suddenly after lying down for a long time and then take the test 30 minutes later.
The study is carried out on an empty stomach, in the morning. You should not visit the laboratory after massage or physiotherapeutic procedures. Any effects on the body, including radiological ones, must be excluded before analysis³.
Figure 1. Norm of total protein and its fractions. Source: MedPortal
Causes of protein deficiency
- Impaired liver synthetic function
- the central metabolic factory. It is here that blood plasma proteins are formed: albumins and most globulins, which largely mediate the maintenance of homeostasis in the body.
This is accomplished by forming oncotic pressure: protein molecules, due to their chemical nature, attract water, thus exercising control over water-salt metabolism. An important consequence can be drawn from this: when the concentration of proteins in the blood serum is low or when they increase in the intercellular fluid and tissues, which is especially characteristic of inflammatory processes accompanied by increased vascular permeability, edema develops - water goes beyond the arteries and veins.
In diseases manifested by damage to hepatocytes (toxic or infectious agents), edema also occurs - and mainly on the lower half of the body and limbs. We wrote about this in more detail in this article:
- Nutritional factors
- fasting, generally leading to protein-energy deficiency, or an unbalanced and uncompensated plant diet with nutraceuticals, accompanied by a lack of essential amino acids in the diet - that substrate for the construction of cells and tissues that the body cannot reproduce on its own, from available elements and with the help of those present enzymes.
Below we have provided a small table with essential amino acids and the foods in which they are concentrated. We hope that this will help you competently organize and choose the type of nutrition that suits you.
| Valin | Isoleucine | Leucine | Lysine |
| eggs | soybeans | peas | chum salmon |
| milk products | peanut | perch | lentils |
| beef | egg yolk | turkey | chicken and turkey |
| lentils | pink salmon | milk | mutton |
| Methionine | Threonine | Tryptophan | Phenylalanine |
| eggs | sunflower seeds | turkey | beans |
| meat | pollock | squid | almond |
| milk and dairy products | zander | milk | cashew |
| mackerel | sesame | pistachios | cod |
- One of the most common pathologies that leads to difficulty absorbing protein from food is reduced acidity of gastric juice.
Hydrochloric acid produced by the parietal cells of the mucosa activates proteolytic enzymes and, in addition, promotes the swelling of protein molecules, facilitating enzymatic processing of food. It is also a powerful nonspecific protection factor that has a strong bactericidal effect - in particular, against protozoa, parasitic worms, bacteria and viruses.
The widespread popularity of self-administration and frequent prescription of proton pump inhibitors (“Omez”) has become a cause of serious concern among scientists about the likely consequences of their long-term use not only on the organs of the gastrointestinal tract, but on the body as such.
In addition to the effects of medications, disruptions in the folate cycle
(or rather, in the three main genes that regulate it: MTHFR, MTR, MTRR), since it is this that ensures the formation of the main mediator of the parasympathetic system - acetylcholine, which also stimulates the parietal cells of the stomach. When a mutation is detected, additional support for the body is necessary, aimed at reducing the concentration of homocysteine that accumulates in such conditions - an amino acid known for its damaging effect on the endothelium (the inner lining of the vessel) and plays an important role in the pathogenesis of atherosclerotic damage.
We recommend
“Vitamin D: top 30 foods with its high content” Read more
On the other hand, along with insufficient formation of acetylcholine, there is an increase in the inflammatory mediator - histamine. This occurs due to a disruption in the processes of its neutralization, normally carried out by methylation reactions. Considering that histamine is also an activator of gastric juice secretion, we can draw a logical conclusion: the effect of the folate cycle on the digestive system is somewhat ambiguous. It is logical to assume that under conditions of excessive intake of this biogenic amine, not only erosive lesions of the gastric mucosa develop, but also, due to increased permeability of the intestinal wall, structural elements of bacteria enter the systemic bloodstream - an inflammatory process is observed, and not limited to the gastrointestinal tract.
Another possible cause of hypochlorhydria is atrophic gastritis
- an autoimmune disease, accompanied by a decrease in the number of functioning cells due to their death during the “attacks” of antibodies from an immune system gone crazy, which ceases to clearly distinguish between what is “ours” and what is “foreign”.
- Damage to the gastric mucosa
: ulcers, gastritis, erosion. Despite the widespread belief in people’s minds that inflammation of the epithelial lining is purely caused by H. pylori, this cannot be compared with one hundred percent truth.
Firstly, infection occurs in early childhood, so the very concept of infection in adolescence or adulthood is more likely an ephemeral rarity than a truth as such.
Secondly, everything depends on the strain of the bacterium: not all of them are aggressive (or at least so strongly pathogenic that clinical manifestation and inflammation of the gastric mucosa itself appear) - and this entails mandatory diagnosis (at least before prescribing 2 weeks of antibiotic therapy). Considering the widespread distribution of the latter, which has already led to total resistance of the microflora (inhabiting both the distal parts of the small and large intestines of humans) to chemicals, as well as the bacterial past of mitochondria, our small power plants, selflessly producing energy, the decision to eradicate Helicobacter It should be well thought out by the doctor or nutritionist that resorting to more gentle therapy with nutraceuticals.
Helicobacter actually adapts (unlike most microorganisms) to the unfavorable conditions of the gastric environment: having a specific enzyme that breaks down urea, it alkalizes its habitat by releasing ammonia. However, pathology develops only when it disseminates - spreads from the pyloric region bordering the duodenum along the entire perimeter of the stomach.
Stress often leads to damage to the gastric mucosa
: it is accompanied by activation of the sympathetic nervous system with the subsequent release of adrenal medulla hormones into the blood, which, in turn, affecting the secretory apparatus of the kidneys, stimulate their release of a vasoconstrictor. It is the narrowing of the lumen of blood vessels, including those that supply blood to the stomach, that leads to subsequent ulceration of the mucous membrane.
- Impaired breakdown and absorption of proteins in the intestine.
The first is characteristic of exocrine pancreatic insufficiency, in which its secretory cells cease to form and release a sufficient amount of enzymes into the blood (and not only proteolytic ones). The second accompanies malabsorption syndrome and celiac disease - another autoimmune disease that, unfortunately, has ceased to be such a rarity today.
- Violation of bile formation and bile outflow,
which leads to the impossibility of not only the emulsification of fats, but also the activation of pancreatic enzymes. Helminthic infestation, blockage of the biliary tract by stones, decreased fluidity of this secretion due to the predominance of cholesterol over other components (bile acids and phospholipids) - a large number of possible causes necessitate careful laboratory and instrumental diagnostics, which build the missing puzzles in the clinical picture of the disease.
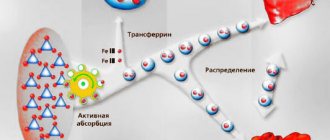
- Kidney diseases:
Normally, protein molecules are not filtered into primary urine due to their bulky size. However, if the renal filter is damaged (the formation of “holes” in it), massive proteinuria is observed, as evidenced by the detection of proteins in a general urine test.
Blood protein levels
Normal indicators for children and adults differ.
Each laboratory sets its own standards (reference values), which depend on the hardware and test methodology. Therefore, to monitor the effectiveness of prescribed therapy, it is recommended to use the services of one medical or diagnostic institution. Table 1. Norms of total protein in a biochemical blood test³
| Age | Norms for men and women, g/l |
| Premature | 36-60 |
| Newborns | 48-73 |
| In children 1-2 years old | 56-75 |
| For children 2-14 years old | 60-80 |
| Over 14 years old and adults | 65-85 |
Women and men do not have a significant clinical difference in blood protein levels⁵. By about the age of three, the amount of proteins in the serum of children and adults becomes almost the same.
Proteins in the human body are produced and broken down continuously: they are constantly renewed. In addition to hormonal and physical factors, this process is influenced by the nature of nutrition, heredity, and the presence of concomitant diseases.
Important!
The norms may deviate slightly in healthy women during menstrual bleeding, pregnancy and breastfeeding. A decrease in total protein to 55-65 g/l during pregnancy is not considered a pathology³.
Albumen
The total protein consists of 50-70% albumin, which determines the oncotic pressure of plasma². With their isolated decrease (hypoalbuminemia), fluid leaves the vascular bed into the tissues and body cavities without returning back. The same mechanism underlies the development of hungry edema.
Albumin performs a transport function, provides cells with necessary amino acids and takes part in maintaining a constant internal environment. The normal content of albumin in the plasma of an adult is 30-50 g/l.² Liver cells produce approximately 12 g of this protein² per day.
Globulins
Globulin molecules have a larger molecular weight than albumins and are less soluble in water. These include specific serum proteins, enzymes, hormones, antibodies (immunoglobulins). Synthesized in the liver and immunocompetent organs.
Almost 35-50% of total protein consists of globulins. Below are the normal values for the main fractions²:
- alpha1-globulins - 1-3 g/l (3-6%);
- alpha2-globulins - 6-10 g/l (9-15%);
- beta globulins - 7-11 g/l (8-18%);
- gamma globulins (immunoglobulins IgA, IgM, IgG) – 8-16 g/l (15-25%);
When the ratio of serum proteins changes, dysproteinemia develops. Each of the fractions has its own functions and properties, therefore, by the deviation of their quantity, one can suspect the cause of the disorders or even a specific disease.
The severity of dysproteinemia is assessed using the albumin-globulin coefficient (ratio of fractions). In healthy people, this value does not exceed 2.5-3.5. With liver cirrhosis or chronic hepatitis, the indicator decreases to 1-1.5 due to impaired albumin production in liver cells¹.
What is hypoalbuminemia?
Albumin structure
Hypoalbuminemia (HA) is a condition in which the main blood plasma protein albumin is reduced. HA develops unnoticed and can lead to serious consequences, so it is important to identify the pathology as early as possible.
- Protein tests: from the variety of studies to the specifics of analyzing total protein in blood serum
Albumin is a simple protein consisting of 585 amino acid residues. The oncotic pressure of the plasma depends on its concentration, that is, the protein is involved in regulating the passage of fluid through the capillary wall. With HA, due to a lack of albumin, fluid accumulates in the intercellular space, which is manifested by edema.
The albumin molecule contains many reactive sites, thanks to which the protein easily binds and transports substances necessary for the body: fatty acids, calcium, magnesium, chlorine, bile acids, bilirubin, vitamins, hormones, and medications. In case of GA, the usual intake of medications can lead to intoxication, since albumin does not effectively perform its function of delivering them to the detoxification organs. Albumin is a central participant in the body's detoxification system. It is able to bind to heavy metal ions and toxic waste products, promoting their elimination. With GA there is a sharp increase in the toxicity index.
Albumin synthesis occurs in the liver, producing about 12 g of protein daily. With increasing needs of the body, for example, with a decrease in osmotic pressure, the process of albumin formation accelerates. But as a result of various diseases, liver hepatocytes are not able to produce enough protein molecules or the rate of albumin breakdown exceeds the rate of its synthesis.
Causes of high protein
An increase in the amount of serum proteins is called hyperproteinemia. It can be absolute (impaired protein production due to organ damage) and relative (associated with changes in plasma volume).
Possible causes of hyperproteinemia²:
- severe dehydration (profuse diarrhea and/or vomiting, ketoacidosis in diabetes mellitus, insufficient water intake, massive sweating);
- extensive burns;
- autoimmune diseases, in which the body begins to produce a large amount of protein immunoglobulins that attack its own organs (rheumatism, systemic lupus erythematosus, sarcoidosis);
- Hodgkin's lymphoma (lymphogranulomatosis) - malignant lesion of lymphoid tissues;
- tumors of the blood and lymphatic system;
- chronic hepatitis in the active phase;
- liver cirrhosis in the initial stages;
- Waldenström's macroglobulinemia is a tumor that primarily affects the bone marrow and produces large amounts of monoclonal immunoglobulin M (IgM);
- peritonitis - active inflammation of the peritoneum;
- intestinal obstruction;
- kidney pathology in the phase of polyuria (excessive urination);
- cholera is an acute infectious disease (especially dangerous), accompanied by damage to the small intestine, massive diarrhea, vomiting and severe dehydration;
- acute and chronic infections.
Important!
Severe hyperproteinemia leads to impaired blood viscosity and improper circulation through the vessels. The most dangerous outcome is disseminated intravascular coagulation syndrome (DIC), in which thrombosis alternates with bleeding.
Symptoms
If the protein deficiency is mild, then it does not manifest itself symptomatically, except in cases of hereditary deficiencies of certain amino acids, which are structural components of protein molecules.
External symptoms include:
- Continuous weight loss;
- Brittle nails;
- Brittle, dull and falling hair;
- Edema;
- Dryness, flaking of the skin;
- Weakness.
Nervous system symptoms:
- Migraine;
- Mood swings;
- Lethargy, fatigue;
- Sleep problems;
- Low mental activity.
Symptoms of the musculoskeletal system:
- Muscle weakness;
- Slow growth in children;
- Decreased muscle mass;
- Pain syndrome in muscles and joints.
Digestive organ symptoms:
- Nausea;
- Bloating, pain;
- Increased consumption of sweets;
- Problems with stool;
- Enlarged liver.
Causes of low protein
Hypoproteinemia is a decrease in the concentration of proteins in the blood. Most often associated with the direct loss of proteins, starvation or inhibition of their synthesis, that is, production in organs.
After surgery, the amount of protein in the blood is reduced. Photo: photography33/Depositphotos
There are the following causes of hypoproteinemia¹:
- burn disease;
- prolonged overheating of the body (hyperthermia), including febrile states;
- diabetes;
- bleeding;
- thyrotoxicosis - hyperfunction of the thyroid gland;
- prolonged physical activity;
- recovery after surgery;
- oncological diseases;
- kidney damage with the development of nephrotic syndrome;
- loss of protein due to inflammation of the intestinal mucosa (enteritis);
- liver damage with signs of cellular failure due to hepatitis, cirrhosis, poisoning (toxic substances, alcohol, medications);
- insufficient intake of protein from food, fasting, exhausting diets, strict vegetarianism);
- impaired absorption of protein foods during pancreatitis (inflammation of the pancreas), intestinal resection (malabsorption syndrome);
- increased breakdown of proteins due to injuries, infectious diseases, Cushing's syndrome;
- inflammatory bowel diseases;
- movement of proteins from the vascular bed into the abdominal (ascites) or pleural cavity (pleurisy);
- severe heart failure;
- inadequate volume of infusion therapy through droppers, resulting in a sharp increase in circulating blood;
- Parhon's syndrome (antidiabetes insipidus) - a violation of vasopressin production due to hyperfunction of the hypothalamic-pituitary system in the brain;
- congenital deficiency of gamma globulins or other protein fractions.
A decrease in the protein portion of plasma can lower oncotic pressure, resulting in the development of edema. The fluid passes from the vessels into the tissues and cavities of the body. This disrupts the nutrition of the vascular wall and blood clotting.
Important!
Total protein levels below 40 g/l are life-threatening³!
Treatment begins after determining the cause of the deviation from the norm. Drug therapy is selected by the attending physician in accordance with the diagnosis, the severity of the patient’s condition, and concomitant diseases.
What is C-reactive protein
h22,0,0,0,0—>
In the results of blood biochemistry, among the protein indicators, you can find a separate type of protein - C-reactive protein (abbreviated as CRP or CRP). This substance belongs to the acute phase proteins or dominant proteins, which are produced at an accelerated rate during damage to body tissues and the development of inflammatory reactions. The protein mobilizes the immune system to fight foreign antigens and activates defense mechanisms. Today it is considered to be a marker of inflammation in the body, much more sensitive than ESR. When a pathological process develops in tissues, the concentration of C-reactive protein quickly increases tenfold.
p, blockquote8,0,0,0,0—>
How to reduce or increase protein in the blood
Therapeutic diets with high or low protein content are selected by a nutritionist in accordance with the patient’s diagnosis. In case of minor deviations from the norm, the problem can be solved by self-correction of the diet.
What foods increase protein in the blood?
A high-protein diet involves consuming 110-120 g of protein per day⁶. Prescribed for patients with diabetes, kidney disease, severe anemia and sepsis.
Important!
Animal products (dairy products, meat and fish) are a natural source of proteins and essential amino acids, which are absorbed by more than 90%. They should make up 50% of the total amount of protein in the daily diet of an adult, 60% for children⁷.
The diet includes the following easily digestible protein sources:
- lean beef, veal;
- rabbit;
- skinless chicken;
- turkey;
- boiled tongue;
- trimmed pork without fat;
- moderately fatty fish varieties, preferably sea or red;
- milk;
- fermented milk drinks;
- cottage cheese;
- sour cream;
- hard cheese;
- eggs (chicken, quail);
- legumes in the form of cereals, in salads;
- mushrooms (with normal tolerance);
- quinoa;
- seeds, sesame;
- tofu;
- nuts;
- soy milk;
- green vegetables.
You can increase protein in the blood with the help of high-protein foods. Photo: antoninavlasova / freepik.com
What foods reduce protein in the blood?
When serum total protein levels are elevated, a low protein diet is followed. Protein consumption is temporarily limited to 20-60 g/day until its level is normalized according to the results of a control blood test. You cannot completely eliminate proteins from your diet without consulting a doctor.
Low-protein nutrition is indicated for severe liver cirrhosis and chronic renal failure. As compensation, the diet is enriched with vitamins and minerals. Drinking plenty of water can naturally reduce protein (berry fruit drinks, compotes, teas). If there is an urgent need, red meat is replaced with white (poultry fillet) along with a large amount of vegetables and fruits.
Sources
- Laboratory tests for the study of specific proteins / Ed. Yu.I. Yarets. Gomel. 2015. 64 p.
- Proteins in blood and urine. Analysis of proteinograms and clinical diagnostic significance. Candidate of Biological Sciences, Associate Professor Gorelaya M.V. Dnepropetrovsk 2015.
- Clinical laboratory diagnostics: textbook / Ed. V.V. Dolgova, Federal State Budgetary Educational Institution of Further Professional Education "Russian Medical Academy of Continuing Professional Education". – M.: FGBOU DPO RMANPO. 2021. – 668 p. ISBN 978-5-7249-2608-9
- Clinical laboratory diagnostics: teaching method. manual for students of medical, pediatric and medical-psychological faculties / S.V. Lelevich, V.V. Vorobiev, T.N. Grinevich – Grodno: GrSMU, 2011. – 166 p.
- Abumuslimov S.S., Magomedova Z.A. Total protein and protein fractions in blood donors in Grozny according to automated analysis // Bulletin of KrasGAU. 2021. No. 6.
- National Association for Clinical Nutrition. Clinical recommendations for the diagnosis and correction of nutritional disorders. Moscow 2013.
- MP 2.3.1.2432-08 Norms of physiological needs for energy and nutrients for various groups of the population of the Russian Federation.
- Druzhinina, N. A. Malnutrition in childhood / Druzhinina N. A. - Moscow: GEOTAR-Media, 2021. - 160 p. — ISBN 978-5-9704-5164-9.