Antibodies are complex compounds that contain carbohydrate and protein (produced by the immune system to detect and destroy pathogenic bacteria and microorganisms). It is worth noting that autoantibodies instantly react to even minimal deviations from the norm in the body: they can begin to perceive healthy cells as dangerous, therefore, actively destroying them.
It is for this reason that an analysis for antibodies to thyroid peroxidase (the enzyme through which the thyroid gland synthesizes iodine-containing hormones) allows one to determine the presence of the disease even when they, in fact, have not yet manifested themselves.
Problems with the thyroid gland and disturbances in the levels of the hormones T4, T3, and TSH can cause serious consequences, such as thyrotoxic crisis, hypothyroid coma, and even death. Endocrinologists unanimously say that problems with the thyroid gland are easy to solve if they are diagnosed in a timely manner.
What is thyroid peroxidase (TPO)
Thyroid peroxidase is an enzyme involved in the formation of thyroid hormones.
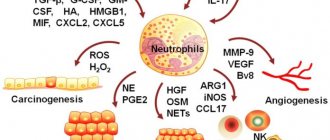
It is responsible for the most important stages of hormonal synthesis - activation of iodine (oxidizes iodide) and the combination of iodinated tyrosines in the process of synthesis of thyroxine (T4) and triiodothyronine (T3). This is a thyroid enzyme of a protein nature, it is also an antigen. With autoimmune inflammation, immune cells mistake the enzyme proteins for foreign ones, and antibodies begin to be produced to it. In this case, the work of the enzyme is disrupted, and therefore the process of formation of thyroid hormones changes. As a result, hormone levels may increase (hyperthyroidism) or decrease (hypothyroidism).
TPO is located on the surface of cells (thyrocytes) and when immunity is impaired, thyroid tissue is damaged, 2 types of autoimmune reactions are triggered at once - with the participation of B-lymphocytes (produce antibodies) and T-lymphocytes (the cellular part of the immune defense). Antibodies to TPO are not the cause of autoimmune diseases, but their indicator, a marker.
Most often (in 75-85% of patients), elevated levels are found in diffuse toxic goiter (Graves disease) and autoimmune Hashimoto's thyroiditis. Slightly less common (65%) is growth with postpartum thyroiditis.
In a quarter of the examined people (15-25.7%) without any other signs of thyroid disease, antibodies were found in significant quantities (this occurs mainly in older women). If antibodies to TPO are elevated in a pregnant woman, they can cross the placental barrier and enter the fetal bloodstream. This can affect the development of the thyroid gland and the health of the unborn child.
General information about the thyroid gland, hormones and TPO
The thyroid gland synthesizes vital hormones that regulate metabolic processes throughout the body. Its enzyme thyroid peroxidase plays a dominant role in this process. The negative impact of antigens leads to impaired productivity, negatively affects the condition of the gland and leads to chronic pathologies. Deviations from normal functioning can lead to excess production of hormones - hyperthyroidism, or deficiency - hypothyroidism.
The presence of antibodies in the blood of pregnant women is especially dangerous. Anti-TPO negatively affects not only the mother's health. They are able to pass through the placenta and enter the fetus. Long-term exposure to antibodies can affect the formation of the thyroid gland of the unborn baby.
Indications for the analysis of antibodies to thyroid peroxidase
A test for antibodies to the thyroid gland is prescribed as part of a comprehensive examination of patients with:
- signs of hyperthyroidism: increased nervousness, weight loss with good appetite, rapid heart rate, arrhythmia, protruding eyeballs, trembling hands, heat intolerance, shortness of breath with light exertion;
- symptoms of hypothyroidism: swelling of the face, eyelids, lethargy, drowsiness, apathy, hair loss, chilliness, weight gain with decreased appetite;
- spontaneous abortion, preeclampsia, unsuccessful IVF attempts;
- an established diagnosis of autoimmune thyroid disease to monitor the effectiveness and duration of treatment;
- an established diagnosis of other autoimmune diseases (for example, systemic lupus erythematosus, pernicious anemia, systemic autoimmune vasculitis, type 1 diabetes mellitus or rheumatoid arthritis) when signs of thyroid dysfunction appear;
- symptoms of disruption of the normal functioning of the thyroid gland and/or detected changes in test results for T3, T4, thyroid-stimulating hormone of the pituitary gland;
- the need to prescribe drugs that affect the functioning of the thyroid gland (for example, lithium, amiodarone, interferon alpha);
- family predisposition to autoimmune thyroid diseases;
- as a preventive measure in the first trimester of pregnancy to identify the risk of thyroid dysfunction during pregnancy and the development of postpartum thyroiditis.
Thyroid peroxidase antibodies (ATPO)
Other names: Thyroid peroxidase antibodies, microsomal antibodies, microsomal antigen antibodies, Anti-thyroid Peroxidase Autoantibodies, Antimicrosomal Antibodies, Antithyroid Microsomal Antibodies, TPO Antibodies, Thyroid Peroxidase Test, Thyroid microsomal antibody, Thyroperoxidase antibody, TPOAb, Anti-TPO.
general information
Thyroid peroxidase (thyroid peroxidase) is an enzyme in the thyroid gland that produces active forms of iodine necessary for the synthesis of thyroid hormones - thyroxine (T4) and triiodothyronine (T3).
Antibodies are protective proteins that are produced by the immune system, recognize and destroy foreign agents (bacteria, viruses, toxins, etc.). However, some antibodies, called autoantibodies, can react this way to your own body tissues.
Antibodies to thyroid peroxidase (ATPO) are specific proteins (immunoglobulins) directed against peroxidase. They are formed when the human immune system mistakenly recognizes thyroid tissue as a foreign object, which can lead to tissue damage and various problems with its function. Thus, the ATPO indicator is a specific marker of autoimmune diseases.
Reasons for the appearance of autoantibodies to thyroid peroxidase:
- genetic predisposition;
- nervous overstrain;
- age-related changes;
- infectious and inflammatory diseases;
- mental and physical injuries, etc.
Important! Quantitative serum analysis for antibodies to thyroid peroxidase is the most sensitive method for diagnosing autoimmune thyroid diseases. Deviation from the norm of its results is an early sign of Hashimoto’s thyroiditis and diffuse toxic goiter (Graves’ disease).
Antibodies to peroxidase in pregnant women are able to penetrate the placental barrier from the mother’s blood into the fetus’s body, which can affect the development of the thyroid gland and the health of the unborn child.
Indications for the purpose of analysis
- examination of newborns if the mother has ATPO and/or established autoimmune thyroiditis;
- screening in the first trimester of pregnancy to identify the risk of thyroid dysfunction during pregnancy and the development of postpartum thyroiditis;
- the presence of symptoms of hypothyroidism (lethargy, apathy, edema, periorbital edema, prolapse, etc.);
- the presence of symptoms of hyperthyroidism (anxiety, irritability, weight loss, tachycardia, etc.);
- presence of changes in other laboratory indicators of thyroid function (T3, T4 and/or TSH);
- monitoring patients with thyroid disease;
- established autoimmune diseases of the thyroid gland (Hashimoto's thyroiditis, diffuse toxic goiter, postpartum thyroiditis, autoimmune thyroiditis, hyperthyroidism or hypothyroidism in newborns) to clarify the effectiveness and duration of treatment;
- prescribing therapy associated with the risk of developing hypothyroidism as a result of the appearance of ATPO (lithium preparations, amiodarone, interferon alpha, interleukin-2);
- miscarriages, premature births, unsuccessful attempts at artificial insemination in women;
- the presence of other autoimmune diseases (rheumatoid arthritis, systemic lupus erythematosus, pernicious anemia, systemic autoimmune vasculitis, insulin-dependent diabetes mellitus);
- patients at high risk for autoimmune thyroiditis (for example, pregnant women with a history of this disease in their family).
Method: electrochemiluminescence immunotest
Analyzer : Cobas 6000
Materials for research: venous blood serum
Units: IU/ml
Interpretation of results
The result of laboratory tests is not a sufficient basis for making a diagnosis. Interpretation of results and diagnosis is carried out only by the attending physician .
Reference values:
0-34,0
Recommendations for preparing for analysis:
- take on an empty stomach, after sleep;
- stop eating 8-12 hours before the test;
- You can only drink clean, still water;
- do not smoke for 2 hours before the test;
- do not consume spicy, fatty, fried foods and alcohol for 2 days;
- exclude physical and emotional stress 1 day before the analysis;
- do not take the test after radiography, physiotherapeutic procedures and instrumental studies.
Possible reasons for increased ATPO levels:
- autoimmune thyroiditis (Hashimoto's thyroiditis);
- diffuse toxic goiter (Graves disease);
- nodular toxic goiter;
- subacute thyroiditis (de Quervain);
- postpartum thyroiditis;
- other autoimmune diseases (rheumatoid arthritis, systemic lupus erythematosus, insulin-dependent diabetes mellitus, thyroid cancer, systemic autoimmune vasculitis, etc.);
- idiopathic hypothyroidism;
- insufficient effectiveness of the therapy or exacerbation of an established thyroid disease.
Possible reasons for a decrease in ATPO levels:
- successful results in the treatment of diseases associated with elevated ATPO levels.
Where to get tested for thyroid peroxidase antibodies (ATPO)
You can get tested for antibodies to thyroid peroxidase (ATPO) at any Synevo point in Minsk, Gomel, Brest, Grodno, Vitebsk, Mogilev, Bobruisk, Baranovichi, Soligorsk, Slutsk, Polotsk, Novopolotsk, Orsha, Zhlobin, Svetlogorsk, Molodechno, Mozyr, Pinsk, Borisov, Rechitsa, Smorgon.
How to properly prepare for research
The test for antibodies to TPO is carried out from venous blood. We recommend:
- donate blood during the period from 8 to 11 am, on an empty stomach, after an 8-12 hour overnight fasting period;
- on the eve of the study - a light dinner with limited intake of fatty foods;
- on the day of the test, drink still water and it is better to avoid coffee and tea;
- 24 hours before the test, exclude alcoholic beverages;
- 1 hour before the test it is better to refrain from smoking;
- 24 hours before the study, exclude the use of medications (in consultation with the attending physician);
- 24 hours before the test, eliminate emotional and physical stress;
- do not donate blood immediately after radiography, ultrasound, massage, endoscopic and physiotherapeutic procedures;
- Rest for 10-20 minutes before donating blood.
What do the results mean?
The normal level of antibodies to TPO is up to 34 IU/ml. If a significant increase is detected, then this is a sign of autoimmune inflammation of the thyroid gland:
- thyroiditis: postpartum, Hashimoto's, newborns;
- diffuse toxic goiter.
A moderate increase in the level of antibodies to TPO can also occur in other autoimmune diseases of the thyroid gland: subacute thyroiditis, single and multiple thyroid nodules, thyroid cancer. An increase in antibodies during treatment indicates its insufficient effectiveness, while a decrease indicates the success of therapy.
Bibliography
- Lapin S.V. Totolyan A.A. Immunological laboratory diagnosis of autoimmune diseases. Publishing house "Man", St. Petersburg - 2010.
- Tietz Clinical guide to laboratory tests. 4th ed. Ed. Wu ANB- USA, WB Sounders Company, 2006, 1798 p.
- Conrad K, Schlosler W., Hiepe F., Fitzler MJ Autoantibodies in Organ Specific Autoimmune Diseases: A Diagnostic Reference/PABST, Dresden – 2011.
- Conrad K, Schlosler W., Hiepe F., Fitzler MJ Autoantibodies in Systemic Autoimmune Diseases: A Diagnostic Reference/PABST, Dresden – 2007.
- Gershvin ME, Meroni PL, Shoenfeld Y. Autoantibodies 2nd ed./ Elsevier Science – 2006.
- Shoenfeld Y., Cervera R, Gershvin ME Diagnostic Criteria in Autoimmune Diseases / Humana Press – 2008.
- Czarnocka, B., Eschler, D. C., Godlewska, M., & Tomer, Y. Thyroid Autoantibodies. / Autoantibodies, 365–373 - 2014
- Weetman, A. P. (2014). Thyroid disease. / The Autoimmune Diseases, 557–574 - 2014.
- Test system manufacturer's instructions