What is calcitonin
Calcitonin is a thyroid hormone, it is produced by C-cells located around the follicles (vesicles with the main hormones - thyroxine, triiodothyronine).
The role of calcitonin:
- takes part in the regulation of phosphorus-calcium metabolism in the body;
- stimulates the work of bone-building cells (osteoblasts) and inhibits destructive cells (osteoclasts);
- slows down the destruction of bone tissue;
- prevents a decrease in bone mineral density (osteoporosis).
The formation of calcitonin depends on the calcium content in the blood; the more calcium, the more hormone is produced. Thyroid tumors produce a lot of calcitonin, so it is considered as a tumor marker.
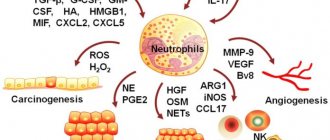
C-cells belong to the diffuse endocrine system, that is, they are not only in the thyroid gland, therefore increased formation of calcitonin also occurs in cancer of the blood, stomach, lungs, mammary, gonads, tumors of the pancreas and adrenal glands (pheochromocytoma).
Blood test for calcitonin
Blood calcitonin is now determined by various laboratories using equipment of various classes to study the level of this indicator. The most modern analyzers, which give the calcitonin analysis maximum accuracy, are 3rd generation immunochemiluminescent analyzers. Widespread and cheap to operate and handle, 2nd generation enzyme immunoassay analyzers provide a significant error in determining the level of calcitonin in the blood, which can lead to incorrect actions both at the stage of examining the patient and at the stage of his treatment. That is why, if during a blood test, calcitonin is the main indicator you are interested in, ask the laboratory what method is used to perform the analysis.
The laboratory of the North-Western Endocrinology Center performs a blood test for calcitonin using an automatic 3rd generation immunochemiluminescent analyzer Liaison XL manufactured by DiaSorin (Italy)
– one of the world's largest manufacturers of equipment for studying blood hormone levels. The accuracy of calcitonin testing using the high-tech 3rd generation method is so high that it often eliminates the errors of tests performed by other laboratories using less modern methods. Very often, patients who have elevated blood calcitonin turn to the North-Western Endocrinology Center - and often a simple double-check of the results using precision equipment makes it possible to find out that in fact the hormone is within normal limits.
| Automatic immunochemiluminescent analyzer 3rd generation DiaSorin Liaison XL (Italy) | 3rd generation chemiluminescent immunoassay analyzer for determining blood calcitonin levels with maximum accuracy |
Why is calcitonin so interesting to endocrinologists and endocrinologist surgeons? The fact is that from the C-cells that produce this hormone, a very dangerous malignant tumor of the thyroid gland grows, which is called medullary cancer or C-cell carcinoma. Medullary cancer grows slowly (this is perhaps its only positive quality), but extremely stubbornly - it is not “afraid” of chemotherapy, with the exception of some drugs from the group of kinase inhibitors, and also does not accumulate radioactive iodine at all and does not respond to external beam radiation therapy. Medullary cancer actively metastasizes to the lymph nodes of the neck, mediastinum, and also spreads its metastases through the blood to the lungs, bones, liver, and brain. Early and timely surgery is the main thing that can bring victory over medullary cancer.
Due to the fact that C-cells, which are the basis for the growth of this type of cancer, produce the hormone calcitonin, its concentration in the blood increases sharply. It is this indicator that is used for the early diagnosis of medullary thyroid cancer. Calcitonin is a method that, if used correctly, can save thousands of human lives.
Currently, about 100-150 cases of medullary thyroid cancer are detected annually in Russia. Not long ago, summary data on the diagnosis of medullary cancer in 16 large and densely populated regions of the European part of Russia were published. Overall data showed that about 40 cases of medullary cancer are detected annually in this vast region. You may be surprised, but in 2013 alone, specialists from the Northwestern Endocrinology Center identified and treated 38 patients with medullary thyroid cancer
. It turns out that one center, albeit a large one, detects as many cases of C-cell cancer per year as 16 regions of our country - and the reason for this lies not only in knowledge of the intricacies of diagnosing this tumor, but also in the competent and active use of calcitonin as a tumor marker.
It should be noted that at present, almost all deaths of patients suffering from various forms of thyroid cancer are caused by medullary or anaplastic cancer. And if we still do not have an effective treatment for anaplastic cancer, medullary cancer is completely curable - and a blood test for calcitonin is designed to help with this.
After lengthy debate, in 2012 the European Thyroid Association in its recommendations indicated the need for a single calcitonin test for all patients with thyroid nodules. The test does not need to be done annually - if the first test shows that the hormone level is not elevated, the next test should be performed only if new nodes appear that were not previously recorded.
Large international studies have shown that when calcitonin levels are determined in all patients with thyroid nodules, previously unsuspected medullary cancer is detected in 1 case out of 300
. In this regard, the European endocrine community is inclined to believe that spending 299 times the money on analysis (and insurance companies pay for the examination there, not the patients themselves) is quite reasonable if, as a result, one patient is diagnosed with cancer at an early stage, when it is still can be cured. By the way, the American Thyroid Association has not yet supported this opinion - in the USA it is believed that such spending of money is unwise (we are talking about the economic efficiency of the method, not about its clinical significance and usefulness - no one has any doubts about this).
Indications for calcitonin testing
Calcitonin determination is carried out for symptoms:
- medullary thyroid carcinoma - nodes in the thyroid tissue, enlargement of the gland and lymph nodes;
- multiple tumors of the endocrine glands - detection of pheochromocytoma, medullary cancer and other neoplasms of the glands;
- osteoporosis: back pain, poor posture, fractures due to minor trauma;
- dysfunction of the parathyroid glands (hyperparathyroidism with bone destruction, increased blood calcium and the deposition of kidney stones, stomach ulcers or hypoparathyroidism with low calcium and convulsive syndrome).
general characteristics
Peptide hormone. Produced by parafollicular C cells of the thyroid gland. Its physiological function as a parathyroid hormone antagonist is to inhibit bone osteoclast activity and reduce serum calcium levels. It may increase with benign lung diseases and during pregnancy. Gradually decreases with age. Typically, an increase in serum levels of both basal and stimulated levels of calcitonin during a provocative test with intravenous calcium administration serves as the main diagnostic criterion for medullary thyroid carcinoma, even in the absence of radioisotope diagnostic data, and correlates with the stage of the disease and the size of the tumor. An unfavorable prognostic criterion for medullary carcinoma after surgery is considered to be an increase in calcitonin levels > 150 pg/ml and a reduction in the time for a twofold increase in calcitonin levels from 2 years to 6 months. To the doctor: if you have a malignant disease, indicate the diagnosis in the referral.
The dangers of high and low calcitonin
Elevated calcitonin indicates diseases:
- medullary thyroid cancer and other tumor diseases;
- renal failure;
- megaloblastic anemia due to vitamin B-12 deficiency;
- increased function of the parathyroid glands;
- alcoholic cirrhosis of the liver;
- inflammation of the thyroid gland.
Low calcitonin is normal; its decrease while taking prescribed medications or after surgery indicates the effectiveness of therapy.
Norm of calcitonin
You need to know that there is no lower norm for this hormone. Even if its level is at zero, this is the norm. The main thing is that the concentration does not exceed the upper limit.
It makes no sense to give standards for the hormone calcitonin, since different laboratories use different models of analyzers. The form that is issued with the analysis results must indicate the actual calcitonin level and its number in accordance with the analyzer model used.
For example, the analysis can be carried out using two methods - ELISA and CLIA. In the first case, a calcitonin concentration of 0.07–12.97 pg/ml will be considered normal, in the second - no more than 1.46 pmol/ml.
With age, the indicators decrease, during pregnancy they increase, but after the birth of the baby they very quickly return to normal.
Important! The material for analysis is blood from the lateral or medial vein of the arm.
How to prepare for analysis
To test for calcitonin, venous blood is needed.
Rules for preparing for the study:
- We recommend donating blood between 8 and 11 am;
- blood must be donated on an empty stomach, after an 8-12 hour overnight fast;
- on the eve of the study - a light dinner with limited intake of fatty foods;
- on the day of the test, you can drink still water and it is better to avoid coffee and tea;
- 24 hours before the test, exclude alcoholic beverages;
- 1 hour before the test it is better to refrain from smoking;
- 24 hours before the study, exclude the use of medications (in consultation with the attending physician);
- 24 hours before the test, eliminate emotional and physical stress;
- You should not donate blood after radiography, ultrasound, massage, endoscopic and physiotherapeutic procedures;
- It is recommended to rest for 10-20 minutes before donating blood.
Calcitonin (quantitative)
Calcitonin is a thyroid hormone synthesized in parafollicular cells, one of the main regulators of calcium-phosphorus metabolism. Calcitonin is a thyroid hormone produced in parafollicular cells (C-cells), one of the most important regulators of calcium-phosphorus metabolism. The formation of calcitonin directly depends on the level of calcium in the blood: when it rises, the concentration of calcitonin increases, and when it falls, it decreases. Once in the blood, calcitonin quickly disappears from it; its half-life, according to various sources, ranges from 2 to 15 minutes. Osteocytes (bone cells) have special receptors, acting on which calcitonin increases the flow of calcium from the blood into the bones, which inhibits bone resorption (destruction, decrease in mineral density). Thus, the action of calcitonin is aimed at reducing blood calcium levels and inhibiting bone demineralization. Calcitonin is a direct antagonist of parathyroid hormone (PTH), a hormone of the parathyroid glands. The effect of PTH is directly opposite to the effect of thyrocalcitonin, although it is also regulated by the concentration of calcium in the blood. It removes calcium from the bones to maintain its desired concentration in the blood. Calcitonin and PTH in a healthy person, interacting with each other, are in balanced quantities for the normal regulation of calcium-phosphorus metabolism, which is mainly responsible for bone density. Vitamin D3 plays an important role in regulating the PTH-calcitonin relationship. Thus, measuring calcitonin levels is primarily advisable in cases of disturbances in calcium-phosphorus metabolism caused by primary osteoporosis. It should be remembered that calcitonin levels must be assessed in conjunction with other markers of bone remodeling. With secondary osteoporosis (which resulted from hypercortisolism, hypogonadism, thyrotoxicosis, hyperparathyroidism), the level of calcitonin does not decrease. The calcitonin test is extremely important for the diagnosis of medullary thyroid cancer, including the detection of multiple endocrine neoplasia syndrome (MEN-IIa, Sipple's disease), which can manifest as medullary cancer, adrenal medulla tumor (pheochromocytoma), or parathyroid hyperplasia and hyperparathyroidism . An increase in the concentration of calcitonin in the blood serum during a test with pentagastrin is the main diagnostic criterion for the presence of medullary thyroid carcinoma; the results of the study determine the stage of the disease and the size of the tumor. After administration of pentagastrin, calcitonin levels increase in almost all patients with medullary thyroid cancer. If it was already elevated, then during a test with pentagastrin it will increase 10-20 times. When the level of calcitonin is at the lower limits of normal or is not detected at all, and after stimulation with pentagastrin it increases significantly, but does not go beyond normal limits, an early stage of medullary cancer or hyperplasia of C-cells of the thyroid gland is suspected. In some patients, intravenous calcium supplements should be used as stimulation, since tumors may not respond to pentagastrin. Calcitonin testing is prescribed after surgical treatment of medullary thyroid carcinoma to evaluate the results of the operation. In particular, it is recommended to take it in the late postoperative period to monitor whether the medullary carcinoma has metastasized and whether there is a recurrence of the tumor. Since the secretion of calcitonin can be influenced by enzymes of the gastrointestinal tract (pepsin), glucagon produced by the pancreas, diseases of these organs (pancreatitis, acute cholecystitis, cirrhosis of the liver) can indirectly affect the synthesis of calcitonin. Analysis used:
- For the diagnosis of medullary thyroid cancer.
- To detect multiple endocrine neoplasia syndrome (MEN-IIa, Sipple's disease), which may manifest as medullary carcinoma, adrenal medulla tumor (pheochromocytoma) or parathyroid hyperplasia and hyperparathyroidism.
- To find out whether there are metastases of medullary thyroid cancer.
- For indirect assessment of the size of medullary carcinoma.
- To evaluate the outcome of surgery to remove medullary thyroid cancer.
- For the diagnosis of primary osteoporosis.
- For the diagnosis of hyper- and hypoparathyroidism.
Analysis is prescribed:
- If medullary carcinoma is suspected (with nodular formations of the thyroid gland, an increase in its size, enlargement of regional lymph nodes).
- When diagnosed with pheochromocytoma, hyperparathyroidism to exclude multiple endocrine neoplasia syndrome (MEN IIa).
- Before and after surgery to remove medullary carcinoma.
- If one of the patient's relatives had medullary cancer.
- For symptoms of osteoporosis (bone pain, deformation and multiple fractures) for a comprehensive assessment of calcium metabolism disorders.
- For calcium-phosphorus metabolism disorders (hyper-, hypoparathyroidism).
Calcitonin (CT)
Material for research: blood serum.
Research method: IECHL.
Calcitonin is a peptide hormone consisting of 32 amino acids and produced by parafollicular epithelial cells (C cells) of the thyroid gland.
The half-life of the hormone in the blood is 12 minutes. Normally, calcitonin is involved in the regulation of calcium metabolism, being a physiological antagonist of parathyroid hormone. In osteocytes, it inhibits enzymes that destroy bone tissue; in renal tubular cells, calcitonin causes increased clearance and release of Ca++, phosphates, Mg++, K+, Na+ and thereby helps reduce the concentration of Ca++ in the blood. The regulation of the synthesis and release of calcitonin is determined by the concentration of Ca++ in the blood: an increased concentration stimulates the synthesis and secretion of the hormone, and a decreased concentration inhibits these processes. In addition, the secretion of CT is stimulated by gastrin and glucagon.
In clinical practice, CT determination is necessary for the diagnosis of medullary thyroid cancer, since in this disease the content of CT in the blood increases significantly, as well as for a comprehensive assessment of calcium metabolism disorders together with parathyroid hormone and vitamin D.
The definition of CT is of exceptional importance for the diagnosis of medullary thyroid cancer. Typically, an increase in serum levels of both basal and stimulated CT levels during a provocative test with intravenous calcium administration serves as the main diagnostic criterion for medullary thyroid carcinoma, even in the absence of radioisotope diagnostic data, and correlates with the stage of the disease and tumor size.
A persistent increase in CT content after tumor removal in patients with medullary thyroid cancer may indicate a non-radical operation or the presence of distant metastases. A rapid rise in CT levels after surgery indicates relapse of the disease. The clinical condition of patients correlates with the CT level in the blood in 67% of patients with medullary thyroid cancer; as the disease progresses, the CT level rapidly increases.
An increase in the level of CT in the blood can be observed in non-malignant lung diseases, acute pancreatitis, hyperparathyroidism, pernicious anemia, Paget's disease. An increase in CT concentration is also possible in case of malignant neoplasms of the breast, stomach, kidneys, and liver.
Attention to the Patient
- the concept of norm is not absolute and has no clear boundaries
- Normal reference values often vary significantly among people of different sexes and age groups.
Remember that only your attending physician, who knows your medical history well, can provide a clear interpretation of the test results.
To the attention of the DoctorReference limits for healthy and sick people are often largely the same. You can contact your BRIGHT-Bio consultant for more information. |
Serum calcitonin levels are normal:
women – up to 12.97 pg/ml; men – up to 30.26 pg/ml.