Heart murmurs in children
One of the common signs of heart damage is heart murmurs. In children, they are divided into systolic and diastolic organic and functional in origin . Heart murmurs in children vary in volume, duration, timbre, zone of maximum localization and area of preferential conduction, connection with systole or diastole. Consultation and examination by a pediatric cardiologist - Markushka polyclinic.
Organic heart murmurs in a child
Organic noises can occur in systole and diastole and are characterized by a fairly definite and constant connection of the sound phenomenon with the anatomical substrate in the form of changes in the walls, openings or valves of the heart or pericardium. These include noises caused by acquired and congenital defects of the heart and great vessels, inflammation of the endocardium and pericardium, and the sound phenomenon of clicks and noises of mitral valve prolapse. The organic nature of the noise can be evidenced by diastolic, pansystolic noises, noises at the end of systole and those combined with tremors, very loud noises, noises that are accompanied by some disorders of the cardiovascular system - pulse asymmetry, clicks, pathological splitting of tones, etc.
Systolic heart murmurs in a child
Systolic murmurs are divided into pansystolic, early, middle, late. Systolic murmur occurs with congenital and acquired defects of the heart and blood vessels.
Diastolic murmurs in children
Diastolic murmurs in children in the vast majority of cases have an organic origin and occur with insufficiency of the semilunar valves of the aorta and pulmonary artery, stenosis of the left and right atrioventricular orifices, pathological discharge of blood in diastole (aortopulmonary septal defect, patent aortic duct, common truncus arteriosus with truncus valve insufficiency and etc.). Unlike systolic murmurs, the intensity of diastolic murmurs correlates with the severity of the defect. Protodiastolic murmur is characteristic of semilunar valve insufficiency, mesodiastolic and presystolic murmurs occur with stenosis of the atrioventricular orifices.
Functional noise
Functional noises can occur in practically healthy children at various ages.
Along the path of blood flow originating from the systemic veins through the heart to the aorta, five normal murmurs may occur, which can be defined as follows.
Spinning top noise (connection of the jugular, subclavian and innominate veins with the superior vena cava). Continuous, often with diastolic accentuation, is best heard under the right clavicle, can be carried into the upper part of the chest on the left, completely disappears in the supine position, which allows it to be differentiated from the murmur of a patent aortic duct or arteriovenous fistula. Murmur on the pulmonary artery (connection of the right ventricle with the pulmonary trunk). It is best heard in the 2nd intercostal space at the left edge of the sternum, can be heard slightly up and down, a wide, fixed splitting of the 2nd sound suggests that the murmur is pathological and may be caused by an atrial septal defect. Murmur of physiological peripheral pulmonary stenosis of newborns (branching of the pulmonary trunk). It is best heard in the upper third at the left edge of the sternum, extends well into both subclavian regions, the back, and also slightly down along the left edge of the sternum, disappears during the first year of life. Atrial vibrating murmur , or Still's murmur (connection of the left ventricle with the aorta). Best heard medially from or above the apex, conducted medially to the lower and middle third of the left sternal border, usually has a much stronger musical component than any of the other normal sounds, and is often described using various terms - vibrating, moaning ", "sounding string". Supraclavicular murmur , or murmur over the carotid artery (the connection of the brachiocephalic vessels with the aortic arch). Best heard in the neck above the collarbones, usually bilateral, can be carried down into the infraclavicular areas.
Other groups of functional noises in children
Noises due to autonomic dysfunction due to changes in muscle tone, especially papillary muscles (shortening or lengthening of muscles), which creates conditions for incomplete closure of the valve leaflets. More often, such noises occur in adolescents who, along with autonomic dysfunction, have increased activity of the thyroid gland.
Heart formation murmurs arise due to the fact that different parts of the heart grow unevenly, which causes a relative discrepancy in the sizes of the chambers and openings of the heart and blood vessels, which leads to turbulence in the blood flow and the appearance of the murmur. There may be unevenness of individual valve leaflets and chords, which leads not only to a temporary failure of the valves' closing function, but also to a change in their resonant properties. These murmurs are most often heard on the pulmonary artery in children of preschool and preschool age, and at the apex in school-age children.
Murmurs of muscle origin are caused by a decrease in the tone of the papillary muscles or the entire myocardium. They are often the result of incomplete closure of the valve leaflets and blood regurgitation. The causes of these noises are acute or chronic dystrophic changes in the myocardium, metabolic disorders in the heart muscle (mucopolysaccharidosis, glycogenosis, etc.).
Murmurs of “small” anomalies of the heart and blood vessels are considered borderline murmurs. This is usually a violation of the architectonics of the trabecular surface of the myocardium or the original location of the chords, the structure of the papillary muscles, small holes in the septa, mildly expressed stenoses of large vessels, etc., creating turbulence in the blood flow, resulting in noise.
Unlike organic noises, functional noises occupy a limited area, are not carried out beyond the cardiac region, are gentle in timbre or have a vibrating, “string” character. Such noises are not constant, their intensity varies depending on the phase of breathing and the position of the child’s body. They are better heard when lying on your back; in an upright position and after physical activity, their intensity weakens significantly or they disappear altogether; they are characterized by lability over time - disappearing or intensifying when listening at short intervals.
Children with functional (atypical) murmurs
Conventionally, children with functional (atypical) noises can be divided into three groups.
Healthy children with clearly functional murmurs such as a formation murmur or a pulmonary artery murmur. Children with murmurs of muscle origin requiring immediate or routine examination. Children with murmurs requiring dynamic monitoring and hemodynamic monitoring.
Bradyarrhythmia
A decrease in the frequency of contractions of the ventricles of the heart less than 60 per 1 minute is qualified as bradyarrhythmia. This class of pathology includes: 1) sinus bradycardia (sick sinus syndrome), sinoauricular blockade, sinus node arrest; 2) atrioventricular block (AVB); 3) atrial fibrillation (Frederick's syndrome - atrial fibrillation in combination with complete atrioventricular block; atrial fibrillation); 4) carotid sinus syndrome (carotidogenic sinus bradycardia and atrioventricular block). Bradyarrhythmia can be functional and organic. The cause of the first form is an overdose of cardiac glycosides, antiarrhythmic drugs, and autonomic influences. The second form is caused by cardiosclerosis due to ischemic heart disease or previous myocarditis. Congenital bradyarrhythmias, as a rule, are a consequence of an abnormality of the conduction system of the heart. In all forms of bradyarrhythmia, a slowdown in the rate of ventricular contractions occurs.” This causes their diastolic overload. At first, circulatory compensation is supported by an increase in stroke volume, due to myocardial hypertrophy. In most patients, blood pressure increases compensatoryly (systolic hypertension). Over time (increasing slowdown of the rhythm), the stroke rate reaches a limit, which leads to a drop in the minute volume of blood circulation. Stagnation occurs in the pulmonary and systemic circulation. Circulatory hypoxia occurs. When the ventricular contraction rate decreases to less than 30 per minute, critical cerebral ischemia occurs. It manifests itself as Morgagni-Adams-Stokes attacks. Usually one of these attacks of asystole is irreversible and leads to death. In other situations, death may occur as a result of complications of arterial hypertension (cerebral infarction, hemorrhagic stroke).. Clinic of bradyarrhythmias. Moderate bradycardia of more than 40 per minute may be the only symptom of pathology. In other situations, patients most often complain of attacks of dizziness up to loss of consciousness, a feeling of slow heart function or stopping, headache, and a feeling of heaviness in the chest. The physical picture is scanty. There is an expansion of the borders of the heart in both directions. Occasionally, a soft systolic murmur may be heard at the base of the heart - the result of volume overload of the ventricles and relative stenosis of their output tracts. With a permanent form of bradyarrhythmia, stable bradycardia and, in most cases, arterial hypertension are detected. In patients with incoming bradyarrhythmias, signs of pathology may not be detected at the time of examination. A critical decrease in heart rate seriously threatens the lives of patients, as it causes episodes of asystole and Morgagni-Adams-Stokes attacks. In such a situation, sudden cessation of blood circulation, loss of consciousness occurs (resulting in injury to the head, limbs, etc.), clonic-tonic convulsions, spontaneous urination, defecation. Most often, the automaticity of the heart is spontaneously restored, and the patient regains consciousness. Resuscitation measures are rarely required. Otherwise, death becomes inevitable. Thus, the clinical picture of bradyarrhythmia is manifested by vivid neurological symptoms. Therefore, patients often end up in a neurological hospital, where they are treated for acute cerebrovascular accidents or epilepsy. Diagnosis of bradyarrhythmias. In all cases, an ECG is informative, which detects certain forms of bradyarrhythmia. Meanwhile, patients with transient bradyarrhythmias require ECG recording for a day or more (Holter ECG monitoring). Diagnostically valuable information is provided by non-invasive electrophysiological studies based on programmed transesophageal electrical stimulation of the heart. The method makes it possible to identify hidden forms of conduction disorders and automatism of the heart, differentiate functional and organic bradyarrhythmias, predict their further course, establish indications for implantation of artificial pacemakers, and select optimal modes of therapeutic cardiac pacing.
Heart murmurs - what to do?
If a child has a heart murmur, the specialists at the Happy children's clinic strongly recommend that mothers do not panic ahead of time, but bring the baby to an appointment with a pediatric cardiologist. Only a qualified examination will make it possible to determine whether the anomalous phenomenon is “innocent” in nature or is a reason to take certain measures.
In addition, do not forget that if murmurs are detected, regardless of their nature, children should definitely visit a cardiologist periodically, because age-related changes in cardiac structures can also occur as the child grows older.
What are “pathological” noises, their causes and dangers
Pathological are those types of heart murmurs that are a consequence of pathology and indicate the presence of a congenital defect. During auscultation, you can pay attention to their distinct character, rough sound, very audible, long-lasting, most often spreading over the surface of the chest. There are cases when congenital defects do not manifest themselves as heart murmurs in a newborn, but appear a month or two later. A dangerous indicator in this case is their increase in dynamics.
As a rule, the pathological type of murmur is accompanied by changes in the ECG, but there are also “invisible” exceptions. The pathology they indicate can be detected by x-ray examination of the organ.
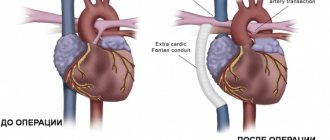
Pathological noises can indicate the presence of problems such as:
- stenosis (mitral, aortic or pulmonary artery);
- development of hypertrophic cardiomyopathy;
- tricuspid valve insufficiency;
- Ebstein's anomaly;
- endocarditis;
- heart failure;
- defect of the interchamber septum;
- the appearance of cardiac myxoma (a rare type of benign tumor) and many other very serious diseases.
Unfortunately, the absence of murmurs is also not a guarantee that there is no pathology developing in the heart in the child’s body, so it is very important to carefully monitor any abnormalities, and if even small problems appear, be sure to discuss them with the pediatrician. Fatigue, weakness, pallor (especially if it is accompanied by blueness of the fingers, lips, tip of the nose), shortness of breath - all this may indicate cardiac pathology.
We all know that the heart is the most important organ that ensures the vital functions of the entire body, therefore its health should be given increased attention from the very birth of the baby.