What are the consequences of the state of hemoconcentration?
Why is hemoconcentration (blood thickening) dangerous during pregnancy? Both the mother and her unborn baby can suffer from this pathology. The doctor immediately puts this situation under control, since the following consequences may occur:
- Varicose veins,
- The appearance of blood clots
- Stroke,
- Heart attack.
For a child, this situation is even more dangerous. He faces:
- Oxygen starvation,
- Pathological development,
- Fading pregnancy
- Risk of miscarriage,
- Premature birth.
What blood tests can indicate blood clotting?
If you suspect an increase in blood viscosity, your doctor will prescribe a blood clotting test.
Thick blood can be caused by a variety of factors and diseases. In some cases, a woman may not even be aware of them.
In most cases, a pregnant woman finds out that she has thick blood at her next doctor’s appointment after she has passed a general test. The doctor will definitely notice an increase in the level of blood cells and hematocrit and will inform the woman about this. Sometimes a pregnant woman can learn about thick blood from a laboratory technician who takes blood from a vein and notices that it is poorly absorbed into the syringe, clogging the lumen of the needle. You should definitely report this phenomenon to your doctor.
If the above-described signs of blood density are detected, the doctor will definitely refer the pregnant woman for a test such as a coagulogram. It is this research method that will help to study the state of the blood coagulation system in more detail and will predetermine further tactics of diagnosis and therapy.
Coagulogram indicators determine the following blood parameters:
- fibrinogen – the norm is 2-4 g/l, with increasing gestational age the figure increases to 6 g/l;
- thrombin time – normal 11-18 s;
- APTT is normal 24-35 s, with an increase in fibrinogen due to an increase in pregnancy, this indicator accelerates to 17-20 s;
- prothrombin – normal 78-142%;
- lupus anticoagulant – normally absent.
With increased blood density, coagulogram parameters change as follows:
- fibrinogen – increases;
- thrombin time – accelerates;
- APTT – accelerates;
- prothrombin – increases;
- lupus anticoagulant – present.
Remember that only a specialist can decipher the results of a coagulogram and assess the degree of blood density! It is he who will be able to decide on the advisability of prescribing drug treatment.
Risks for mother and baby
The main danger lies in the formation of blood clots.
Often, after childbirth, a new mother may develop varicose veins. Blockage of blood vessels can negatively affect both the fetus, which will experience oxygen deficiency, and the expectant mother herself. Because of this, the possibility of miscarriage or premature birth, heart attack or stroke may increase significantly. In the early stages, excessively thick blood can lead to a frozen pregnancy. Therefore, it is so important to visit a doctor on time and fully follow his recommendations. If you have any doubts about the prescribed treatment, immediately consult with several doctors, so you can eliminate the risk of medical error or negligence.
Pregnant woman
In the last weeks of pregnancy, the expectant mother strives to prepare her apartment or house as much as possible for the arrival of a new family member. Scientists call this sign of impending birth nesting syndrome. Many women observe signs of the syndrome from the thirtieth week of pregnancy, but at the 39-40th week nesting reaches its maximum point. Pregnant women strive to do general cleaning and repairs, re-stick wallpaper and purchase many new things that, in their opinion, are simply necessary in the house. After giving birth, many purchases cause confusion. The reason for this behavior is an increase in the level of adrenaline and norepinephrine in the body. These hormones are produced by the adrenal glands; they are necessary not only for the woman, but also for the baby to prepare for the upcoming birth.
Is thick blood during pregnancy dangerous for the woman and fetus?
Having identified a change in blood density in a pregnant woman, the doctor assesses the degree of these disorders and determines the tactics for managing the patient.
It is based on the results of a coagulogram that a specialist will be able to determine the degree of danger of blood thickening during pregnancy. In some cases, with minor changes in indicators, the doctor does not attach serious importance to blood density and gives the woman general recommendations regarding diet and fluid intake aimed at eliminating this symptom. In such situations, you should not worry, because such blood thickening does not pose a threat to either the expectant mother or the fetus, and after childbirth, the coagulogram indicators stabilize on their own.
Sometimes the cause of blood thickening during pregnancy is taking iron-containing drugs, which are prescribed when hemoglobin levels decrease. Such a symptom should also not cause concern in a woman, because after eliminating anemia and discontinuing these medications, the blood condition will stabilize.
For more serious changes in coagulogram parameters, the doctor may recommend that the pregnant woman undergo a course of blood thinning therapy. In such situations, a woman should also not worry, but simply follow all the doctor’s orders. The danger of such blood thickening lies in the increased risk of blood clots and obstructed blood flow through the vessels, but this situation can be corrected.
The slow flow of viscous blood through the vessels and a more intense load on the heart causes insufficient supply of oxygen and nutrients to all tissues and organs. This leads to the following symptoms in a pregnant woman:
- constant lethargy;
- memory impairment;
- drowsiness;
- dry mouth;
- heaviness in the legs;
- coldness of the extremities.
With a sedentary lifestyle and lack of treatment, an increased tendency to blood clots can lead to the development of the following complications in the expectant mother:
- thrombosis;
- thrombophlebitis;
- TELA;
- varicose veins;
- diseases of the cardiovascular system (heart attack, hypertension, stroke, atherosclerosis).
Significantly increased blood density also negatively affects the condition of the unborn baby. As a result of increased thrombus formation and slow blood flow, the following disorders may occur on the part of the fetus:
- miscarriage or premature birth;
- frozen pregnancy;
- hypoxia;
- developmental delay.
It is in connection with the above possible complications of thick blood that women planning a pregnancy should refuse to conceive until the course of treatment for this condition is completed. In some cases, this disorder in the blood coagulation system can be life-threatening for the expectant mother and baby, and not all medications can be taken by a woman while carrying a child. Therefore, it is better to get rid of this symptom before pregnancy.
- Finger joints hurt during pregnancy: causes of pain in the hands
When planning a conception, the doctor will definitely prescribe a coagulogram to rule out disorders in the blood coagulation system. It is especially important to conduct such a study in certain risk groups:
- the woman has a history of miscarriages or missed pregnancies;
- the woman or her relatives have varicose veins;
- close relatives of the woman had thrombosis, heart attacks or strokes;
- a woman professionally engages in sports that involve intense physical activity.
Pregnant woman
The long wait to meet your unborn child is coming to an end; the 40th week of pregnancy is the last for most women. Every day the expectant mother’s anxiety increases, and the long wait affects her mood and well-being. Women strive to give birth to a child as quickly as possible, so that pregnancy and painful contractions become a thing of the past. Every pregnant woman dreams of meeting her baby, wants to hold him to her breast and stroke his tender head.
Many women, especially first-time mothers, worry that labor will begin unnoticed, but such cases are extremely rare. A woman feels the onset of labor, feels regular contractions that repeat at certain intervals and gradually increase, the time interval between them shortens.
Contractions may be preceded by prenatal rupture of amniotic fluid, which is observed in a certain percentage of women in labor. After the water breaks, contractions may be quite weak or completely absent. Regardless of the intensity of contractions, the release of water is one of the signs of the onset of labor and requires immediate contact with specialists and the woman’s hospitalization in a maternity hospital or hospital, since when the water breaks, the integrity of the bladder is disrupted and the risk of microorganisms dangerous to the baby’s health entering the uterine cavity increases. It is important that after the water breaks, the baby is born within a maximum of 10-12 hours.
A pregnant woman must properly tune in to childbirth, concentrate on the desired result and believe in her own strength, and complete the task intended for her by nature. The right psychological attitude and theoretical knowledge will help a woman become a mother, successfully go through all stages of childbirth and hold the long-awaited child to her heart.
Causes
While carrying a baby, the expectant mother is faced with a huge number of tests. A general blood test and hemocoagulogram are mandatory tests that are included in the recommended list of laboratory tests performed during pregnancy.
“Thick” blood is a clinical concept that is defined when the amount of formed elements in the blood is significantly increased. Typically, various thrombus formation disorders lead to the development of this situation during pregnancy. These pathologies can appear both in the early and late stages of pregnancy.
It should be noted that normal blood is quite liquid. This physiological feature is necessary for its transport and nutritional functions to be fully realized.
There are quite a lot of different nutrients dissolved in the blood, as well as oxygen. All these elements are needed by the fetus for its active growth and development.
The development of pathological disorders associated with the formation of thick blood is caused by the following causes:
- Individual characteristics of the expectant mother. If a woman had any hematological disorders before pregnancy, then during pregnancy they will progress significantly. This situation usually occurs in families where several members have various diseases of the cardiovascular system. A history of heart attack or stroke in close relatives of a pregnant woman is also a predisposing factor to increased thrombus formation.
- Violation of the drinking regime. Insufficient intake of water into the expectant mother's body can lead to her blood becoming thicker. This violation occurs quite often if a woman suffers from toxicosis. Frequent vomiting contributes to dehydration, which leads to severe blood thickening.
- Insufficient supply of essential vitamins and microelements. Vitamin balance is very important during all periods of pregnancy. Carrying a baby is a very energy-intensive time. To carry out all biological reactions, enzymes are needed, which cannot be formed in the mother's body without certain vitamins and microelements.
- Frequent consumption of sweets and other “fast” carbohydrates . A large amount of sugar entering the blood leads to a significant change in its viscosity. If the expectant mother eats a lot of sweets and candies throughout her pregnancy, this can not only contribute to increased blood clot formation, but even lead to the development of signs of diabetes mellitus.
- Oversaturation of the body with iron-containing drugs . These drugs are usually prescribed to pregnant women who have had a decrease in hemoglobin during pregnancy. Excessive intake of iron-containing drugs can lead to an increase in platelets in peripheral blood.
- Impaired functioning of the spleen . This organ is necessary for the body to maintain optimal concentrations of blood cells. Hypersplenism is a pathological condition that is characterized by significant disturbances in the functioning of the spleen.
This pathology, which occurs during pregnancy, also contributes to the progression of thrombosis.
It is important to note that there are a number of specific pathologies that occur mainly only during pregnancy. antiphospholipid syndrome can lead to an increase in blood viscosity and disruption of its fluidity Doctors note that the incidence of this pathology is only growing every year.
Severe blood loss or traumatic shock resulting from some type of injury may also cause baseline blood counts to change. These pathologies can also appear if a pregnant woman shows signs of internal bleeding. This condition is already extremely unfavorable and requires urgent medical attention.
- Why do my legs hurt during early and late pregnancy, what should I do?
Calculate gestational age
39th week of pregnancy: what happens to the fetus?
At the 39th week, the child’s weight reaches 3,100-3,500 g, and his height is 50-52 cm. Height and weight indicators are very relative and can differ significantly. The baby is rapidly preparing for the most important test in his life - birth, which requires endurance and significant effort. During this period of pregnancy, the size and weight of the child’s adrenal glands, that is, the glands of the endocrine system, which are responsible for the human body’s response to stress factors, increase. It is the hormones adrenaline and norepinephrine produced by the adrenal glands that help the child adapt as quickly as possible to new temperature conditions, tactile, sound and light impulses.
All the baby's senses are developed at 39 weeks. Within a few moments after birth, the baby can focus his gaze, he reacts to bright light and moving objects, many scientists claim that newborns distinguish colors and see the faces of parents and doctors. In the last weeks of intrauterine life, the baby's hearing is also fully developed; after birth, he reacts to loud sounds and noise. A newborn baby can identify the basic shades of taste, recognize sour, bitter, sweet and salty.
In the womb, the baby is in an aquatic environment that minimizes contact. Immediately after birth, the baby experiences many tactile sensations; unlike intrauterine life, he feels the touch of his mother’s hands and diapers, towels, dressings and other materials. Babies especially like the touch of skin to skin, so in a modern maternity hospital, newborns are always placed on their mother’s stomach even before the umbilical cord is cut. The child adapts more easily to the new environment and feels protected. Placing the baby out has not only a psychological aspect, since it promotes the colonization of microorganisms from the mother’s skin onto the skin and mucous membranes of the baby, and increases his immunity.
Diagnostic tests to determine blood viscosity
Often, too thick blood during pregnancy is detected during routine testing. When blood is taken from a finger, it clots too quickly, clogs the tubes, flows poorly, etc.
However, visual analysis alone is not enough to correctly diagnose and identify the causes of pathology. A coagulogram is intended for these purposes. This diagnostic method helps determine whether there are problems with blood clotting and helps develop the correct treatment tactics. The examination is carried out only on an empty stomach.
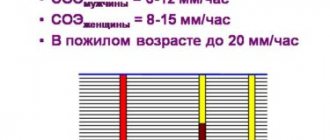
The following indicators are important for making a diagnosis:
- Prothrombin index. It shows the rate of blood clotting as a percentage. The optimal indicators are 110% with deviations of 32%. If the patient's readings are higher, the blood is too thick.
- Fibrinogen content. In the first trimester, its amount should be from 2 to 4 g/l, in the third – about 6.
- Thrombin time is the rate at which a blood clot forms. Normally, it is formed in 15 s. For pregnant women, the indicator is slightly increased - up to 25 s.
- Lupus coagulant - a woman's tendency to develop lupus.
- Activated partial thromboplastin time. Normally it ranges from 25 to 35 s, for pregnant women - from 17 to 20 s.
Diagnosis at home
It will be difficult for a pregnant woman to independently identify such a problem, because physiological discomfort may not necessarily be associated with an increase in blood viscosity. Therefore, at the first signs of thick blood, it is important to contact your doctor as soon as possible and undergo the necessary tests.
At home, a coagulogram can be done using a portable coagulometer
On the other hand, the modern medical equipment market offers convenient and simple devices for performing coagulograms at home - coagulometers. These devices allow you to determine the prothrombin time (blood clotting time) and the level of prothrombin in the blood.
The device comes with sterile needles, which are used to make a painless puncture on the finger. Next, the biomaterial is applied to the test strip supplied with the coagulometer (3–5 pieces in a package), which is placed in a special guide hole.
The analysis is carried out in one and a half to two minutes, the result is displayed on the display. Test strips have a certain expiration date, so they can be shown to your doctor if necessary.