Pulmonary hemorrhage: types, treatment
We are talking about a dangerous complication of various pathologies of the respiratory system, which is accompanied by the leakage of blood from the vessels located in the bronchi or lungs and its release.
Characteristic manifestations of the syndrome:
- Cough, which produces blood, liquid scarlet or in the form of clots;
- State of weakness;
- State of dizziness;
- Reduced blood pressure;
- Fainting state.
In order to identify the cause of the syndrome, various diagnostic methods are used, for example, radiography, tomography, bronchoscopy, etc.
To stop the syndrome, various treatment methods are used, including conservative hemostatic therapy and surgical treatment.
The syndrome is typical for lung oncology, as it occurs in half of patients.
The intensity of the syndrome varies: its severity is estimated from 600 ml to more than a liter of blood loss per day.
Kinds
It is important to see the difference between the two concepts “pulmonary hemorrhage” and “hemoptysis”. The latter is less dangerous, it is characterized by a lower volume and rate of blood release, but it can often precede bleeding. Therefore, the importance of its treatment is undeniable.
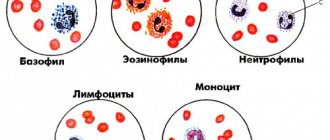
The classification, which has been used since 1990, distinguishes three degrees of bleeding:
- The first stage is daily blood loss from 50 to 100 ml;
- The second stage is daily blood loss from 100 to 500 ml;
- The third stage is daily blood loss of more than 500 ml.
The condition of heavy bleeding, which occurs simultaneously or over a short period, is extremely dangerous. So, in a severe form of the syndrome, the immediate blood loss can be more than 100 ml.
The difference between “hemoptysis” and “pulmonary hemorrhage” is also important because the first does not frighten the oncologist, he simply makes adjustments to the treatment, while the second requires urgent help, often resuscitation.
Complications
Asphyxia is considered the most dangerous complication of pulmonary hemorrhage. Sometimes atelectasis is recorded. Due to LC, the main process progresses, which happens both with pulmonary tuberculosis and with purulent diseases of this organ. Hemoaspiration pneumonia is also a common complication. It includes pneumonia and pneumonitis (a condition caused by hemoaspiration). Hemoaspiration pneumonia is understood as pneumonitis, the cause of which is aspiration of blood, and which is complicated by the addition of infectious flora.
Hemoaspiration pneumonia can be determined by symptoms and X-ray data on the 2-5th day after hemoaspiration. The localization of the lesion on the side of the source of bleeding and below it is radiologically determined as broncholobular or with the presence of small broncholobular foci. Statistics on the prevalence of this complication of pulmonary hemorrhage are contradictory. According to TCH No. 7 of the city of Moscow, the disease occurs in 9% of patients with confirmed hemoaspiration. In the intensive care unit, where patients with moderate and major bleeding are treated, hemoaspiration pneumonia is observed in 44.9% of cases, including bilateral localization in 23% of cases.
Causes
The causes of the syndrome are often associated with cancer - tumors of the bronchi and lungs. Sometimes the cause is secondary damage to the bronchi and lungs by metastases from other organs.
The cause of bleeding in oncology is a vessel corroded by atypical cells. The tumor disrupts the normal functioning of the vascular wall of the bronchi, it becomes inelastic and blood begins to flow out of it. That is, there is a connection between the size of the vessel defect and the intensity of bleeding.
Most of the bleeding occurs in the first stage of the syndrome. If lightning bleeding occurs, it is extremely difficult to save a person: two thirds of patients die within the first hour if help is not provided.
Symptoms
Medical practice shows that the syndrome is usually preceded by a severe cough. At first it is dry, then mucous sputum and blood admixtures are observed. As we have already said, the blood can be scarlet or in the form of clots.
In some cases, the precursors of the syndrome are:
- A tickling or gurgling sensation in the throat;
- Burning in the chest.
The general condition of the patient largely depends on how the blood loss is expressed. It could be:
- Fright;
- State of sudden loss of strength;
- Pallor;
- Sweating;
- Reduced blood pressure;
- Cardiopalmus;
- Feeling dizzy;
- Shortness of breath, etc.
If the syndrome is classified as profuse, the following may occur:
Coughing up bloody mucus
- State of fainting;
- Vomit;
- Convulsive state;
- Visual impairment;
- Asphyxia.
Symptoms of pulmonary hemorrhage
Bleeding can happen at any time and even completely for no reason against the background of complete rest or moderate exercise. Everything else depends on the rate of blood loss. If hemoptysis has already been noted before, then the patient is less afraid, but when blood comes out of the throat, everyone is scared.
As a rule, with serious bleeding, a strong and uncontrollable cough begins, which is accompanied by progressive shortness of breath, as blood flows into the alveoli and turns off gas exchange in them. Blood may foam when mixed with air. Vomiting of swallowed blood often occurs; in the rejected masses the blood is red. The heartbeat increases, the patient becomes covered in sticky cold sweat, the hands and feet become cold due to a decrease in peripheral pressure. Blood drains, strength is lost.
Book a consultation 24 hours a day
+7+7+78
Diagnostics
To determine the syndrome, an examination by an ENT specialist is necessary. That is, it is necessary to understand the nature of the bleeding, because its causes can be not only the lungs, but also the mucous membrane and the stomach.
Main types of diagnostic tests:
- X-ray;
- Computed tomography using contrast.
If it is impossible to find the source of bleeding, bronchoscopy is performed. The method can also be used as a therapeutic method, especially when there is a threat to the patient’s life.
Angiography is another diagnostic method. It is often resorted to when the syndrome is minor and its source has been identified.
Material and methods
The work is based on an analysis of the results of treatment of 134 patients with LC who were at the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky in the period from 2006 to 2015. The criterion for inclusion in the study was confirmation of the fact of LC by endoscopic examination.
All observations were retrospectively distributed depending on the nature of the underlying disease (damage) that was the cause of bleeding.
LC as a result of mechanical injuries was observed in 53 (40%) victims, in 42 - with closed chest trauma, in 11 - after penetrating stab and gunshot wounds.
In 81 (60%) cases, LC was of a non-traumatic nature. In 11 (8.2%) cases, pathological changes in blood vessels were verified as the cause of LC, including vascular malformations (8), pulmonary sequestration (2) and pulmonary hemangioma (1).
15 (11.2%) patients were diagnosed with lung malignancies, including squamous cell carcinoma (5), adenocarcinoma (4), dimorphic (2) and small cell (1) cancer, carcinoid (1) and metastatic lung lesions (1) .
The cause of LC in 12 (9%) patients was nonspecific inflammatory lung diseases, including bronchiectasis (9), pneumonia (2) and cystic fibrosis (1).
In 21 (15.7%) cases, LC was idiopathic in nature, including 12 with signs of chronic obstructive pulmonary disease.
Against the background of pulmonary tuberculosis, bleeding was noted in 7 (5.2%) patients who were under our supervision before confirming the diagnosis, and after achieving hemostasis were transferred to specialized medical institutions.
In 7 (5.2%) cases, LC occurred against the background of pulmonary hypertension due to a previous pulmonary embolism (PE).
In 5 (6%) of 8 patients, LC occurred on the operating table during surgical interventions for an aortic aneurysm (4) and pathological changes in the valvular apparatus of the heart (1), in 3 - due to rupture of a thoracic aortic aneurysm with the formation of an aortobronchial fistula (1 ), productive pulmonary vasculitis (1) and pulmonary endometriosis (1).
The male to female ratio was 2.7:1, and the average age of patients was 43 years (range 16–87 years). The average age of patients with traumatic lung cancer is 32.1 years, of patients with a lung tumor - 60 years.
Combined injuries were diagnosed in 33 (62.3%) patients with traumatic LC. Victims with closed chest trauma had more severe injuries than those with chest injuries, the average values on the ISS scale were 18.6 and 10.1 points, RTS - 7.29 and 7.68 points, respectively.
Concomitant diseases were present in 65 (48.5%) patients with LC; every third patient with non-traumatic LC had arterial hypertension (34.5%).
The duration of LC at the time of admission to the hospital varied from 1 hour to 7 days. In 128 patients, BL was observed for the first time, in the remaining 6 there had been previous episodes of bleeding.
According to the classification of V.I. Struchkova et al. [10], in 91 (68%) patients the amount of bleeding corresponded to grade I, in 27 (20.1%) - grade II, and in 16 (12%) - grade III. Table data 1 indicate relatively more severe bleeding if its cause was coagulopathy during cardiac surgery and closed lung injuries. In these groups, grade II and III bleeding was observed in 75 and 45% of patients, respectively.
Table 1. Distribution of patients by etiology and degree of LC Note. * - according to the classification of V.I. Struchkova et al. (1985).
The majority of patients with LC—120 (89.6%)—were hospitalized in intensive care units, 49 (36.6%) of them required artificial ventilation lasting from 4 hours to 10 days or more.
All patients, regardless of duration and etiology of LC, underwent clinical, laboratory, radiological and endoscopic examinations, and in 123 cases, spiral computed tomography (SCT). A comparative retrospective analysis of the results of using the X-ray method and SCT in identifying the localization of the suspected source of L.K. was carried out. Data from radiological research methods were verified using fiber-optic bronchoscopy (FBS).
A total of 43 endovascular studies were performed in 40 cases, which accounted for 30% of the total number of cases of LC. In 39 cases, angiography was performed for non-traumatic LC and only in 1 case for a false aneurysm of the bronchial artery with an arteriobronchial fistula 6 months after a gunshot wound to the chest. In the remaining patients with traumatic pulmonary artery angiography was not used due to the fact that embolization of damaged vessels of the pulmonary circulation is inappropriate due to the risk of developing pulmonary infarction and pulmonary hypertension.
Some clinical and laboratory parameters are given in table. 2. On admission, patients with closed chest trauma had relatively low systolic blood pressure (on average 106 mm Hg), which indicated the severity of the injuries. At the same time, in a number of other patients, in particular with idiopathic LC, the average systolic blood pressure reached 150 mm Hg. The average hemoglobin content in the blood of patients with LC was 114 g/l. However, with a certain etiology of bleeding, in particular with closed chest trauma and when it occurred during cardiac surgery, a significant decrease in hemoglobin levels was observed - on average to 99 and 86 g/l, respectively.
Table 2. Clinical and laboratory characteristics of LC observations Note. The median values are indicated; BP - blood pressure; HR—heart rate; RR - respiratory rate; Hb - hemoglobin; INR—international normalized ratio; PTI—prothrombin index; APTT—activated partial thromboplastin time.
Comparatively significant changes in the blood coagulation system were observed in patients with LC secondary to a previous history of pulmonary embolism. The INR level reached an average of 2.8, PTI - 43.2%, APTT - 52 s. These changes in this group were due to the use of anticoagulants in half of the observations before the development of LC.
For mathematical processing of the obtained data, statistical packages MS Excel and Statistica 10.0 were used. The research results were tested for reliability using the Pearson χ2 test. In cases of deviation from the normal distribution, the nonparametric Mann-Whitney test for unrelated samples was used to compare data. Differences at p
<0,05.
Treatment
In the treatment of the syndrome, therapeutic methods, hemostasis, and surgical operations are applicable.
Therapy is prescribed for the syndrome classified as the first two stages.
Aspiration is necessary to remove blood from the tracheal lumen. If we are talking about asphyxia, then urgent intubation, blood suction and artificial ventilation of the lungs are necessary.
Among the medications, hemostatic drugs and antihypertensive drugs are prescribed.
If therapeutic methods do not give a positive result, the syndrome is stopped through local endoscopic hemostasis.
As a rule, these methods help to stop the development of the syndrome for some time.
Palliative surgery is used in cases where it is impossible to perform radical surgery.
As for radical operations, they are aimed at partial resection of the lung, for example, marginal resection or removal of the entire organ.