Hydropericardium - what is it?
Hydropericardium is an abundant accumulation of fluid in the heart sac. This bag itself consists of two leaves surrounding the heart. Their task is to protect it and separate it from other organs. Fluid accumulates in the middle of the sac (called the pericardium). Its amount is insignificant, and it is designed to prevent friction of the walls of the bag against each other, as well as the heart. For normal conditions, the leaves are 3-5 millimeters apart from each other, the amount of accumulated liquid is up to 50 milligrams.
If there is too much fluid, it prevents the heart from working normally, which can lead to cardiac tamponade and cardiac arrest.
The disease we are talking about dramatically increases the amount of natural fluid in the heart sac by several times. If the natural amount of liquid mass ranges from 15 to 50 milligrams, then in a pathological condition this amount can be over a liter. In addition, when pathology develops, blood or lymph enters the bag.
Causes of hydropericardium
Normally, fluid (transudate) is produced by the cells lining the pericardium from the inside, and is reabsorbed by them. Its quantity increases in two cases - with increased production or slower absorption. Many diseases can lead to this disorder:
- chronic heart failure;
- pericarditis;
- cardiomyopathy;
- congenital malformations of the heart and pericardial sac;
- a decrease in blood protein levels, which occurs in many diseases;
- hypothyroidism;
- allergy;
- injuries;
- anemia;
- radiation therapy;
- chronic renal failure;
- tumors of the mediastinum (the place in the chest where the pericardium and heart are located).
There are special forms of hydropericardium in which fluid accumulates and:
- lymph (chylopericardium – a consequence of blocking the flow of fluid through the lymphatic vessels; occurs during metastasis of malignant tumors);
- blood (hemopericardium; causes - trauma to the heart or pericardial vessels, myocardial infarction, obesity).
Why does pericarditis occur?
The following are the main causes of pericarditis:
- Infectious agents: viruses, bacteria, fungi and even parasites. The inflammatory process in the pericardium is triggered by the influence of exo- and endotoxins released by microorganisms.
- Autoimmune connective tissue diseases such as lupus erythematosus or scleroderma. At the same time, the body synthesizes antibodies to its own cells, which damage connective tissue and cause systemic inflammation.
- Heart diseases. The result of serious damage to the heart muscle is the spread of the pathological process to the surrounding pericardium. This can occur with transmural myocardial infarction, infectious or reactive myocarditis.
- Damage to other organs, such as the kidneys, can lead to pericarditis. In cases of serious impairment of excretory function and the formation of renal failure, deposition of metabolic products in the serous cavities, including the pleura and pericardium, is observed.
- Penetrating pericardial injuries that disrupt the integrity of the pericardial layers.
- Metastatic tumors that cause pericardial carcinomatosis.
- The causes of pericarditis are varied, and, therefore, treatment approaches depend on what caused the inflammation. But in the absence of timely diagnosis and correction of this condition, the outcome is always the same. The result of chronic pericarditis is cardiac tamponade, which leads to the death of the patient.
At CELT you can consult a cardiologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
Signs of hydropericardium
With this syndrome, the onset of symptoms does not begin immediately. At first, only signs of the disease that caused the hydropericardium are noticeable. With a small accumulation of fluid, it does not manifest itself in any way, but as its amount increases, the heart is compressed and it is impossible to contract. Main manifestations:
- shortness of breath at rest or with minimal effort;
- increased heart rate;
- edema syndrome;
- decreased blood pressure due to decreased cardiac output;
- pallor of the skin, blueness of the lips and the space between the upper lip and nose (acrocyanosis of the nasolabial triangle).
With massive hemopericardium, the vagus nerve adjacent to the esophagus is irritated and then painful hiccups can occur. This is a sign of a life threat, and in this case it is necessary to immediately call an ambulance.
In case of hemopericardium due to injury, a critical condition may occur - cardiac tamponade. In this case, the heart contractions are not enough to push blood through the vessels, and the person may die within a few minutes. Dobrobut.com clinic specialists recommend studying cardiopulmonary resuscitation measures and using them in such cases - this is the only chance to save a person before specialists arrive. If symptoms of tamponade appear, you should immediately call a doctor. Symptoms:
- a sharp decrease in pressure, especially with loss of consciousness;
- feeling of lack of air with frequent shallow breathing;
- weakness, darkening of the eyes;
- feeling of heartbeat;
- fear of death, overexcitement
Possible complications
The development of complications of hydropericardium is associated with the severity of heart failure.
An increase in the volume of pathological effusion to 1-1.5 liters provokes an increase in symptoms: pressure numbers decrease, shortness of breath worsens, and swelling becomes more noticeable. Advanced hydrocele of the heart leads to the development of tamponade, in which accumulated fluid compresses the heart muscle so much that physiological contractions become impossible. The clinical picture of the condition is accompanied by a pronounced loss of strength, weakness, attacks of suffocation with frequent shallow breathing, a feeling of rapid heartbeat, and episodes of loss of consciousness. In such a case, emergency medical attention is required.
Diagnosis of hydropericardium
The main method for diagnosing this condition is ultrasound. Echocardiography in the area in the area of the posterior wall of the left ventricle of the heart can reveal a discrepancy between the parietal and visceral layers of the pericardium, which is normally 5 mm. An increase in this distance clearly indicates the presence of liquid between the sheets. Criteria for echodiagnosis of hydropericardium:
- 6-10 mm divergence of the leaves is the early stage of hydropericardium;
- 10-20 mm – moderate stage;
- over 20 mm – pronounced stage.
In the latter case, an additional puncture of the pericardium is performed with suction of part of the fluid and study of its nature (inflammatory exudate, lymph, blood, etc.)
Echocardiography can also identify hydropericardium in the fetus during pregnancy. In this case, the diagnostician should suspect a congenital heart defect in the unborn newborn or a hemolytic disease. In this case, the woman should be thoroughly examined and, if necessary, undergo a course of appropriate treatment under the supervision of specialists.
In addition to ultrasound, to diagnose diseases that have led to a worsening of the condition, you will have to undergo other studies:
- chest x-ray;
- general urinalysis and complete blood count;
- thyroid hormone levels;
- blood protein level;
- ECG, etc.
Clinical picture
If the fluid content in the pericardial cavity is low, the person does not notice anything. The condition worsens when there is 80–100 ml in the “bag”. Patients experience pressure in the front behind the sternum, which increases when the torso is tilted forward.
Further symptoms of impaired cardiac activity appear:
- general weakness;
- shortness of breath independent of physical activity;
- pain behind the sternum of a pressing nature, very long-lasting due to compression of the coronary vessels and increasing myocardial ischemia;
- paroxysmal suffocation;
- the face and hands are swollen and look puffy;
- swelling on the feet and legs increases.
The neck veins become visible without palpation
When examining a patient, the doctor pays attention to:
- pulsating veins in the neck (due to compression of the mouth of the vena cava);
- constant tachycardia;
- tendency to lower blood pressure;
- dull heart sounds on auscultation.
In the advanced stage, due to compression of the esophagus, there are difficulties in swallowing, hiccups are disturbing.
If the pericardial cavity is full, then symptoms of incipient cardiac tamponade appear:
- weakness increases;
- the feeling of heaviness in the chest is constant and intensifying;
- shortness of breath at rest;
- the skin is covered with profuse cold sweat;
- the patient is excited, there is a fear of death;
- tachycardia intensifies, heart sounds are barely audible;
- a drop in blood pressure causes dizziness and fainting;
- breathing is shallow, frequency reaches 30 per minute.
Lack of treatment is accompanied by acute heart failure, cardiogenic shock, cardiac arrest and death.
Treatment of hydropericardium
The underlying disease is what the doctor should first pay attention to. Treatment of heart failure, taking medications containing thyroid hormones, restoring protein levels are all methods of treating the disease that caused the hydropericardium. Often this approach is enough to relieve the patient of this symptom.
There may be situations when there is not enough time to wait for the effect, and then it is necessary to supplement the treatment of the underlying disease by combating the hydropericardium directly. Initially, diuretics are used - potassium-sparing (spironolactone, triamterene, hydrochlorothiazide) or thiazide diuretics (furosemide, torsemide) in combination with potassium supplements. If there is no result and if the volume of fluid is critical, it is possible to perform a pericardial puncture with pumping out excess exudate.
Hydropericardium is a symptom or complication. The underlying disease that led to the appearance of this symptom needs to be treated. And it is best to prevent the development of such complications, for which you should consult a doctor if there are any signs of trouble in the body.
Related services: Cardiac examination
Acute pericarditis: key issues in diagnosis and emergency care
Evgeny Evgenievich Gogin
Professor, corresponding member of the Russian Academy of Medical Sciences.
Making a diagnosis of “pericarditis” has always caused certain difficulties for clinicians. Doctors received fundamentally new opportunities for diagnosing this disease with the advent of echocardiography (EchoCG). In the past, there was no doubt that pericarditis was rarely detected at the initial presentation of the patient. The doctors were not sure that the condition was assessed correctly. Sometimes pericarditis was detected only at autopsy. When using echocardiography, this diagnosis is obvious already in the early stages of the disease.
Pericarditis is not among such common diseases as hypertension or ischemic heart disease and other clinical forms of atherosclerosis, but they are more common than myocarditis and cardiomyopathies combined. This is because pericarditis not only accompanies most infectious myocarditis, but is also characteristic of patients with endocarditis and severe myocardial infarction (with a heart attack, local pericarditis occurs - Kernig's epistenocardial pericarditis and Dressler's widespread autoimmune pericarditis).
Pericarditis complicates the course of the postoperative period during cardiac surgery in a third of patients (postpericardotomy, posttraumatic, postcommissurotomy pericarditis). Along with other serositis, pericarditis occurs with systemic connective tissue diseases (systemic lupus erythematosus, rheumatoid disease), as well as with rheumatism. They may be the only or one of multiple manifestations of active tuberculosis. Pericarditis manifests itself most clearly in the case of a drug-induced disease; in a number of other cases it allows the detection of a metastasized tumor.
Many pericarditis is relatively mild and ends in recovery even in the absence of targeted treatment. At one time, this became the reason for the unreasonable inclusion in clinical classifications of so-called acute benign pericarditis, presumably of viral etiology. However, the nature of most of these pericarditis turned out to be allergic: viral pericarditis occurs only in combination with viral myocarditis (this is indirectly confirmed by the fact that viral pleurisy and peritonitis are extremely rare). However, determining the etiology of pericarditis after its detection most often remains a very difficult task.
Acute dry pericarditis
As a rule, it is possible to suspect acute dry (fibrinous) pericarditis already at the first examination based on the characteristics of pain and the characteristic friction noise of the pericardium. However, the routine methodology of a medical examination of a patient with complaints of pain in the heart, as well as decreased interest in auscultation and deterioration of auscultation skills make the establishment of initial forms of pericarditis a rare success. Many patients complain of pain in the heart area, and the doctor first of all excludes true angina or myocardial infarction. Doctors are sometimes inclined to consider other pains uninformative and lose interest in them if the patient can tolerate these pains. When listening to the heart, the doctor, as a rule, does not ask you to hold your breath during inhalation and exhalation, and does not note the direction of propagation of the noise, and this is necessary to detect a pericardial friction noise.
Pain during pericarditis can be moderate, and in some cases very severe, as with myocardial infarction. They are monotonous, increase gradually, last for hours, are not relieved by nitroglycerin, and only temporarily weaken with the use of analgesics. Complaints of palpitations, shortness of breath, dry cough, general malaise, and chills are possible. The characteristic dependence of pain on breathing, movements, and changes in body position brings the picture of the disease closer to the symptoms of dry pleurisy - the patient cannot take a deep breath.
The pericardial friction noise at the height of pain is gentle and limited in extent. It is difficult to distinguish from a short systolic murmur. With an increase in fibrinous deposits on the pericardial layers, the noise becomes rough and is heard over the entire zone of absolute dullness of the heart. It can be biphasic or triphasic, since it occurs not only in ventricular systole, but even during atrial contraction and in the phase of rapid diastole of the heart. All components of such noise are similar in character and strength; it is compared to the rhythm of a steam locomotive. It is possible to verify the pericardial origin of a murmur heard only during systole by listening to the heart in different phases of breathing. The noise occurs either on exhalation or only on inhalation. The friction murmur is always limited to the zone of absolute dullness of the heart or localized in some part of it. A distinctive feature of pericardial murmur is its poor conductivity, it “dies where it was born”, and is not conducted even into the zone of relative cardiac dullness.
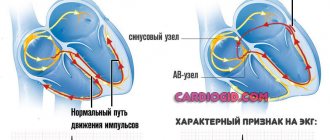
When, during acute pericarditis, the subepicardial layers of the myocardium are involved in the inflammatory process, ECG changes occur. An early sign of acute pericarditis is a concordant rise of the T wave, covering all standard leads within 1–2 days (the greatest rise is noted in lead II). A tall positive T wave is formed.
After 1–2 days, the ST interval drops below the isoelectric line, then within a few days it returns to the isoelectric line, despite the ongoing inflammatory process in the pericardium. With slowly progressing pericarditis, no ECG changes occur. Depending on the etiology of dry pericarditis, in some cases, rapid positive dynamics of the process are noted, the friction noise remains narrowly localized (epistenocardiac murmur), and is heard for only a few hours. In other cases, the course of pericarditis becomes protracted or recurrent, in third cases it transforms into effusion (exudative) pericarditis.
Exudative pericarditis
Exudative pericarditis means total involvement of the heart lining in the inflammatory process. Liquid effusion can accumulate after the stage of dry pericarditis or bypassing it, with rapidly beginning (allergic) and with primary chronic “cold” (tuberculous, tumor) pericarditis. With the slow accumulation of fluid, intrapericardial pressure does not increase even with large effusions (up to 2–3 l). Inside the stretched pericardial cavity, the anterior surface of the heart and its apex usually maintain contact with the outer layer of the pericardium, since during systole, due to the stretching of the aorta and pulmonary artery by the blood, the heart is thrown towards the anterior chest wall. The apex beat of the heart is displaced upward and medially from the lower left border of dullness. This is due to the accumulation of fluid in the pericardium. The boundaries of dullness change depending on the position of the patient's body. When he stands up, the area of dullness in the second and third intercostal spaces is reduced by 2–4 cm on each side (displaced medially), and the dullness in the area of the lower intercostal spaces expands by the same distance. Absolute dullness in the lower parts comes close to the boundaries of relative dullness, and there is a sharp transition to tympanitis over the compressed lung.
Heart sounds, even with the accumulation of large effusion in the pericardial sac, often remain clearly audible medially from the apical impulse. In the lower left sections of dullness, they are weakened, since the heart in the cavity stretched by effusion is displaced upward and medially (a uniform decrease in the sonority of tones is a sign of myogenic dilatation of the heart).
X-ray picture. Behind the shadow of the fluid-filled pericardial sac, the shadow of the heart itself is indistinguishable. An early sign of exudate accumulation is not so much an increase in size as a change in the contour of the “heart” shadow: its outlines are rounded, the waist is smoothed. The triangular shape of the shadow is characteristic of long-standing chronic pericardial effusions. It appears due to the fact that the outer layer of the pericardium loses its elasticity. A spherical shadow indicates a more active process with a rapid increase in the volume of effusion. The exudate actively stretches the outer layer of the pericardium, which has not lost its elasticity, thereby creating high intrapericardial pressure. The patient's venous pressure increases and the liver swells. A sip of a contrast suspension allows you to establish a posterior displacement of the esophagus. The pulsation of the shadow contour weakens.
With echocardiography, the layer of fluid anterior and posterior to the contour of the heart is reliably visualized as an anechoic space. Often, compaction of the pericardial layers is also noted, and heterogeneous shadows of fibrinous deposits are determined, and with large effusions, characteristic vibrations of the heart inside the stretched pericardial sac.
Cardiac tamponade
With the rapid accumulation of effusion in the pericardial cavity, cardiac tamponade develops, tachycardia occurs, and pulse filling decreases. There is no congestion in the lungs due to an obstruction to the blood supply to the right heart. The presence of congestive wheezing in the lungs contradicts the diagnosis of cardiac tamponade. When you inhale, especially little blood flows to the left heart, since the capacity of the vascular bed of the lungs increases. The left heart becomes empty as you inhale, and the pulse volume drops.
A paradoxical pulse appears. When the weakening of the pulse during inspiration is not pronounced enough, you should put a cuff on the shoulder, increase the pressure in it above the minimum blood pressure and ask the patient to breathe deeper - during inspiration the pulse wave disappears completely. The paradoxical nature of the pulse is often of decisive diagnostic importance.
Echocardiographic signs of cardiac tamponade are not as informative as clinical symptoms. The greater the intrapericardial pressure, the higher the venous pressure, which is manifested by swelling of the neck and peripheral veins. The liver enlarges and becomes painful, especially its left lobe. Since in certain positions the basin of the superior vena cava is partially unloaded, a patient with increasing cardiac tamponade usually sits, the torso is tilted forward, the forehead rests on a pillow (Breitman's pose) or freezes in a deep bowing position. Painful attacks of weakness occur with a small, barely perceptible pulse, and the patient experiences fear of death. The skin is covered with cold sticky sweat, cyanosis increases, the extremities are cold, and consciousness is periodically disturbed. There are vital indications for pericardial puncture. The faster tamponade develops, the more dangerous the delay; sometimes the count is not days, but hours or minutes.
Interpretation of effusion detected by echocardiography
EchoCG makes it possible to establish initial forms of pericarditis that were previously inaccessible for diagnosis. These small, usually spontaneously resolving effusions cannot always be differentiated from exudative pericarditis (as is sometimes written in the echocardiographic report): often it is not an inflammatory effusion, but a hydropericardium.
The presence of intrapericardial fluid up to 100 ml during examination of patients with acute infarction can be detected by echocardiography much more often than signs of dry epistenocardial pericarditis. In these cases, it is difficult to exclude hydropericardium due to acute hemodynamic disturbances. In severe forms of myxedema, an effusion almost always forms in the pericardium, but it is usually small. Hydropericardium without general edema is also described in cases of severe cardiac atrophy, mainly in people of the older age group, as well as in patients with alcoholic cardiopathy. There is usually no pain in the area of the heart and no friction noise with hydropericardium, but sometimes a touch noise similar to a short light friction is heard.
The final diagnostic and highly effective treatment measure in the clinic of effusion pericarditis remains puncture. It allows you to conduct a cytological examination, perform bacteriological, immunological and biochemical tests. When puncture is performed using the lower approach using Larrey or Marfan, there is no risk of injury to the heart and pleura. The needle enters the lower anterior corner of the pericardial sac, where a large amount of fluid accumulates during exudative pericarditis. Punctures through the intercostal spaces are strictly contraindicated, no matter what needle or catheter they are performed, even under ultrasound control. All tragic cases of heart injury with a needle or mandrel occurred (and continue to occur if the surgeon is inexperienced) during punctures through the intercostal spaces. In systole, the heart, even with a large effusion, is thrown forward, and the contracting atrium damages itself against the needle section protruding into the pericardial cavity. The length of such a scarifying wound sometimes reaches 2 cm, and catastrophic cardiac tamponade occurs. The patient can only be saved by immediate surgery to suturing the heart wound.
Etiological diagnosis of acute pericarditis
Such diagnosis remains difficult, and in many cases is speculative. Meanwhile, both the prognosis and treatment tactics largely depend on the nature of pericarditis. The diagnostic problem is solved in detail when examining a patient in a hospital.
The diagnosis of tuberculous pericarditis is especially difficult. More often it occurs in people with a hyperergic tuberculosis process of a different localization or in people who have had tuberculosis in the past. Pain in the heart area is rare. Low-grade fever, night sweats, and dry cough are observed. The course of the disease is long and sluggish; intrapericardial effusion can be large without the development of tamponade. Sometimes the effusion persists stably for years, almost without being accompanied by fever and inflammatory changes in the blood (“cold” flow). The myocardium is not involved in the process, and no ECG changes occur. The greatest difficulty is in diagnosing those forms in which pericarditis becomes the “calling card” of active tuberculosis; however, there is no damage to the lungs or other organs. Lymphocytes predominate in the pericardial effusion, antibodies to Koch bacilli are detected, but Mycobacterium tuberculosis can only be detected biologically; Clinicians attach importance to high tuberculin tests. In later stages, X-ray examination can detect areas of calcification.
Pericardial tuberculosis, one of the forms of organ tuberculosis, is severe and unfavorable: high temperature, leukocytosis, night sweats, rapid accumulation of exudate in the pericardial cavity, loss of body weight. The process, even with active treatment, often leads to constriction after 1.5–2 months and then requires urgent pericardiectomy. An equally difficult task is to establish the nature of non-infectious pericarditis.
Allergic pericarditis is characterized by an acute onset with sharp pain in the heart area and a tendency to relapse; it occurs some time after exposure to a resolving factor (administration of serum or allergenic medication). They usually occur in the form of myopericarditis with the formation of serofibrinous effusion, skin rashes and other manifestations of a drug-induced disease or allergic condition.
Autoaggressive (alterogenic) pericarditis is associated with various heart injuries: post-infarction pericarditis, post-commissurotomy, post-pericardotomy. Most often, post-infarction syndrome (Dressler's syndrome) with clear, sometimes violent manifestations occurs in the 3rd week of acute myocardial infarction, when the highest titer of circulating antibodies to myocardial antigens is detected. Post-infarction syndrome can first form in a wide time range - from 10 days to several months after a heart attack, depending on the nature of the course of coronary artery disease and a number of associated factors, and with a re-infarction it often occurs from the first days of acute coronary syndrome.
The interest of surgeons in the timely diagnosis of pericarditis after cardiac surgery has increased. Expansion of the technical capabilities of surgery and an increase in the number of cardiac surgical interventions require increasingly reliable and accurate characterization of pericardial diseases, determination of their phase and the degree of functional impairment of the patient’s condition.
Pericarditis due to tumors is usually hemorrhagic, but in 50% of cases, an uncolored effusion is detected at the first puncture. It becomes hemorrhagic later. A large amount of liquid accumulates in the cavity. With cancerous pericarditis, often up to 90% of leukocytes in the exudate are lymphocytes, and conglomerates of tumor cells are found. Cytological examination is highly informative. Tumor pericarditis develops more often in the second half of life, but sometimes at a young and even childhood age (sarcoma). Differential diagnosis is most often carried out with tuberculous pericarditis. The tumor process is characterized by a steady course with constant accumulation of effusion (“inexhaustible exudate”), and the ineffectiveness of anti-tuberculosis and anti-inflammatory treatment. The introduction of thiophosphamide into the pericardial cavity for cancerous pericarditis ensures not only the cessation of exudation, but often also obliteration of the cavity. For pericarditis complicating the course of pneumonia or sepsis, the introduction of an antibiotic into the pericardial cavity is effective.
Features of manifestations of hydropericardium in newborns
Specialists in neonatal resuscitation note a connection between the development of hydropericardium in newborns and:
- prematurity;
- complication of central venous catheterization when the catheter is in place for 3–4 days.
The umbilical vein is most accessible for the necessary intravenous administration of drugs
This is proven by the same composition of the fluid in the pericardial cavity and that introduced through the system (in 97% of cases). The incidence of cardiac tamponade associated with hydropericardium reaches 3%. And the mortality rate of newborns with catheters in the umbilical vein is 0.7 per 1000.
Other causes of fluid accumulation are extremely rare and are more associated with inflammatory diseases.
There remains controversy among resuscitators regarding the role of the catheter tip and its level:
- Some suggest that when catheterizing the central vein in a newborn, it should not be brought closer than 1 cm from the shadow of the heart during X-ray examination in premature infants, and 2 cm in full-term infants. With this localization, the end of the catheter does not reach the site of attachment of the pericardial layers.
- Others believe that inserting a catheter directly into the right atrium is quite safe.
Another equally controversial issue is the effect of injected solutions of increased concentration on the atrium wall. It has been proven that they lead to “delayed” damage to the heart wall (on days 3–4), which coincides with the timing of the onset of hydropericardium.
Clinical manifestations in newborns are different: an asymptomatic course is possible until death is declared. But more often it develops in the same way as in adult patients, acute heart failure, a state of shock. For children, bradycardia is more typical than tachyarrhythmia.
Stages and forms
The degree of development of hydrocephalus varies depending on the amount of effusion accumulated in the pericardial sac.
- Minor hydrocephalus - the volume of fluid does not exceed 100 ml;
- moderate - volume from 100 ml to 500 ml;
- large - the volume of transudate exceeds 500 ml.
At the third stage, up to 1 liter of transudate can accumulate in the pericardial sac.
Depending on the characteristics of the permeate composition, the following forms are distinguished:
- Hemopericardium - blood accumulates in the pericardium. This phenomenon occurs when the blood vessels supplying the pericardial tissue rupture, a heart attack, trauma, or obesity of the heart;
- Chylopericardium - when the lymphatic ducts are compressed, the outflow of lymph is disrupted, and lymphatic fluid accumulates in the pericardium.
Classification
This is done on two grounds. The first concerns the type of change that occurs.
Accordingly they talk about:
- Hydropericardium. Classic shape. There is a release of fluid into the sac surrounding the heart. Essentially, this is a serous transudate that comes out of the vessels and intercellular space for one reason or another. Which one you need to look at.
- Chylopericardium. Impaired lymph drainage. The main development factors are trauma, tumors, and inflammatory processes.
- Hemopericardium. It is not part of the structure of a typical hydropericardium, since it is not serous fluid that accumulates in the cavity, but blood. Some scientists combine all three pathological varieties in one classification.
The second criterion is the degree of severity. The basis for the distinction is the volume of output.
- First. No more than 100 ml in total. The pathological process is accompanied by minor symptoms. The clinical picture includes chest pain of moderate intensity, shortness of breath, and nausea. There may be pressing discomfort, a feeling as if a heavy stone had been placed.
- Second degree. 100-300 milliliters. Accompanied by severe clinical manifestations, breathing disorders, heart sounds, pallor, cyanosis. The patient takes a forced position, usually half-sitting due to increasing asphyxia and arrhythmia.
- Third degree. Over 300-400 ml. The risk of death is maximum, recovery in a hospital setting is urgent. Without help and surgical intervention, the patient will die.
Despite the indicated volumes, the pericardium can take up to several liters of fluid. All this time the patient is walking on the edge; at what point he breaks down is a matter of the body’s endurance. It's not worth testing.
Forecast
{banner_banstat10}
Determined by the degree of impairment, timeliness of treatment and underlying disease. Hydropericardium of the 1st degree is easily treated, survival rate is maximum.
The third degree, especially if the transudate volume is over 500 ml, is associated with high mortality. Approximately 60-70% without quality timely intervention.
If it is possible to completely cure the etiological factor, they speak of good prospects. Otherwise, constant monitoring by a cardiologist will be required, as relapses are likely. Even the best specialist won’t say when exactly.