Diuretics in the treatment of cardiovascular pathology
S – diameter of vessels.
The rheological properties of blood are determined by hematocrit (polycythemia), blood viscosity (hyperlipidemia, hyperfibrinogenemia, hyperglycemia), erythrocyte mobility, platelet aggregation state, etc.
Thus, there are 5 main areas of application of therapeutic interventions in the treatment of HF and hypertension:
1) sympatho-adrenal system - blockade of a- and b-adrenergic receptors;
2) kidneys – diuretics;
3) renin–angiotensin–aldosterone system – ACE inhibitors and vascular AT1 receptor blockers;
4) vascular system - peripheral vasodilators, in particular anti-calcium drugs;
5) blood rheology – antiplatelet agents, hypolipidemic, hypoglycemic, etc.
Modern cardiology cannot be imagined without β-blockers, of which more than 20 names are known, ACE inhibitors [5]. However, currently diuretics occupy a priority place in the treatment of dilated cardiopathy and hypertension
.
In the treatment of hypertension, there are three main goals: immediate, intermediate and final [1,6,7].
Immediate goal
antihypertensive therapy - reducing blood pressure to a “normal” level (< 130/85 mm Hg), and, if possible, an “optimal” level (< 120/80 mm Hg).
Interim goal
– prevention of target organ damage (central nervous system, heart, kidneys).
Final goal
– improve the quality and increase the life expectancy of patients with hypertension through the prevention or regression of cardiovascular complications.
Accumulated clinical experience indicates that thiazide diuretics have fairly high antihypertensive activity, not inferior to β-blockers, calcium antagonists, ACE inhibitors and α1-blockers. Numerous studies have shown that when treated with thiazide diuretics, systolic blood pressure decreases by an average of 10–20 mmHg, and diastolic blood pressure by 5–15 mmHg. [8–10].
Comparative studies have shown that there is no significant difference in the antihypertensive activity of low (<25 mg hydrochlorothiazide per day or equivalent doses of other drugs) and high doses (>25 mg) thiazide diuretics. Based on pooled data from 31 studies, high doses of thiazide diuretics reduced blood pressure levels by an average of 18/11 mmHg, and low doses by 13/9 mmHg. At the same time, low doses of diuretics are much better tolerated by patients and are not accompanied by significant electrolyte and metabolic disturbances [11].
Unlike beta-blockers, diuretics are equally effective in preventing cardiovascular complications in both middle-aged and elderly patients with hypertension. In 18 randomized studies in which diuretics and beta-blockers were used in the treatment of hypertension in patients over 60 years of age, it was found that diuretics effectively prevent the development of primary and recurrent cerebrovascular accidents [12]. However, unlike beta-blockers, diuretics are more effective in preventing the risk of coronary heart disease and death, which makes them first-line drugs in the initial treatment of hypertension.
Thus, thiazide diuretics are prescribed in small doses (no more than 25 mg per day), have fairly high antihypertensive activity and are well tolerated. This is the only class of antihypertensive drugs known to improve long-term prognosis in patients with hypertension.
Thiazide and thiazide-like diuretics can be divided into two generations. The first generation is derivatives of benzothiadiazone (hydrochlorothiazide, etc.) and phthelimidine (chlorthalidone, etc.); the second generation is chlorobenzamide derivatives (indapamide, etc.), which in chemical structure are a chlorobenzamide derivative containing a methylindoline group.
The hemodynamic effect of indapamide-like diuretics is due to their pharmacological action. In particular, indapamide
- a moderate saluretic diuretic associated with inhibition of the reabsorption of Na+, Cl–, H+ and, to a lesser extent, K+ and Mg2+ in the proximal and distal tubules of the short segment of the nephron. At the same time, indapamide eliminates the excess content of sodium ions in the vascular wall (due to its high lipophilicity), increases the synthesis of prostaglandin E2 and prostacyclin I2, inhibits the influx of Ca ions into vascular smooth muscle cells, which causes their dilation and reduces their sensitivity to pressor agents (catecholamines, thromboxane) . The total hemodynamic effect of indapamide is manifested as:
- vasodilating effect
- decrease in OPSS
- lowering systemic blood pressure
- changes in the viscosity properties of blood due to inhibition of platelet aggregation activity.
The effect of indapamides on blood pressure without a significant effect on diuresis is manifested in a daily dose of 2.5 mg, with an increase in which the diuretic effect becomes dominant.
In its hypotensive activity, indapamide is 30 times superior to the effect of spironolactones, 100 times superior to furosemide, and 300 times superior to chlorthalidone when used in comparable doses [13]. One of the identified antihypertensive effects of indapamide is its effect on renal production and release of prostaglandins, inhibition of the formation of the vascular vasoconstrictor thromboxane. Under the influence of indapamide in patients with essential arterial hypertension, the release of prostaglandin E2, which has vasodilating activity, increased. The effect of indapamide inhibiting the synthesis of thromboxane A2 in human platelets and stimulating the release of vasodilating prostacyclin I2 was verified in vitro [14].
The therapeutic efficacy of indapamide diuretics has been demonstrated in a number of large randomized studies. Their ability to prevent the development of coronary artery disease by reducing myocardial mass in hypertension
.
This property, atypical for other classes of diuretics, makes indapamide a unique drug with a cardioprotective effect
, the severity of which is not inferior to beta-blockers and ACE inhibitors.
Particular attention is drawn to the fact that indapamide-like diuretics do not have a withdrawal syndrome and do not cause adverse metabolic disorders: they do not have a negative effect on glucose metabolism and blood lipid levels. Recent studies have shown that indapamide helps normalize glucose metabolism in type 2 diabetics
, preventing diabetic nephropathy. A similar pattern was noted in the study of cholesterol and triglyceride metabolism in patients with dyslipoproteinemia. Indapamide reduces the level of atherogenic low-density cholesterol and triglycerides, while simultaneously increasing the concentration of high-density lipoproteins [15].
Thus, indapamide, combining all the positive pharmacodynamic, pharmacokinetic and economic advantages, in the absence of side effects of other diuretics, is a drug that is promising in terms of therapeutic tactics in patients with hypertension and chronic heart failure.
CHF is quite often a consequence of arterial hypertension syndrome and remains one of the main causes in the structure of causes of disability and mortality from cardiovascular pathology. Currently, the drugs of choice in the treatment of CHF with LV systolic dysfunction are ACE inhibitors, and for diastolic dysfunction - diuretics. The basis of CHF in most patients with hypertension is a violation of the diastolic and systolic function of the left ventricle, therefore the most promising is combined treatment with ACE inhibitors and diuretics. Taking into account the above, for the treatment of CHF, preference should be given to thiazide-like diuretics - indapamides
with moderate strength and long-lasting action [16]. Indapamide, reducing the level of intracellular calcium while maintaining the magnesium content, reduces the rigidity of the vascular wall and promotes more effective relaxation of the cardiomyocyte in diastole. At the same time, the synthesis of prostacyclins increases, platelet aggregation and the release of thromboxane A2 decrease, which overall has a positive hemodynamic effect by reducing afterload for the LV.
Indapamide, improving microcirculation in the kidney, eliminates microalbuminuria, which is a marker of generalized vascular damage and a predictor of cardiovascular and renal complications.
Thus, the use of diuretics, in particular indapamide-like ones, is relevant and promising in the prevention and treatment of hypertension and CHF.
Literature:
1. Preobrazhensky D.V., Sidorenko B.A. Differential drug therapy for arterial hypertension. Consilium Medicum. 2001. T 3, 10, p. 83
2. Preobrazhensky D.V., Sidorenko B.A., Shatunova I.M., Maryenich A.V. The place of diuretics in the treatment of hypertension. Indap. Moscow, 2000.
3. Smith TW, Brannwald E. The management of heart failure // Heart Disease. 1984.587.
4. Grantham JJ, Chonko AM The physiological basis and clinical use of diuretics. Sodium and Water Homeostasis. New York, 1978, 179.
5. Shilov A.M., Knyazeva S.A., Ushakova M.V. Beta blockers in the treatment of hypertension. Russian medical news. 2001, VI, 4, p. 31.
6. Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. //Arch. Intern. Med. 1997, V 157, 213.
7. Evsikov E.M. Indapamide is a modern antihypertensive drug with a combination of mechanisms of action. Indap. Moscow. 2000. 26.
8. Stimpel M. Arterial hypertension. Berlin – New York, 1996, 8.
9. Kaplan NM Clinical hypertension. 7 edition. Baltimore, 1998.
10. Opie LH Drugs for the heart. 4th edition. Philadelphia, 1995.
11. Ames RP A comparison of blood lipid and blood pressure responses during the treatment of systemic hypertension with indapamide and with thriazides. // Amer. J. Cardiol. 1996, 77, 128 – 168.
12. Psaty B., Smith NL, Siscovick DS and all. Health outcomes associated with antihypertensive therapies used as first–line agents. A systematic review and meta-analysis. JAMA, 1997, 277, 739.
13. Ogilvie RI Diuretic treatment in essential hypertension. // Current Medical Research and Opinion. 1983, N8, 53.
14. Gbeassor FM, Grose JH, Le Bel M. Influence of diuretics on prostaglandin and thromboxane synthesis. // Clin. and Invest. Med., 1982, N5. 26.
15. Passeron J., Panly N., Despart J. International multicentre study of indapamide in the treatment of essential arterial hypertension. Postgrad. //Med. J., 1981, V 57, 53.
16. Kuimov A.D., Lozhkina N.E., Kazina N.P. Treatment of patients with CHF with hypertension syndrome with indapamide in capsule form and enalapril. Indap. Moscow. 2000. 77.
ABOUT HEART FAILURE AND THE USE OF DIURETICS
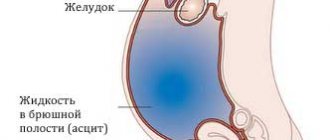
Some patients with CHF have very moderate manifestations of cardiac decompensation. It is important for the doctor to overcome the stereotype that dictates the prescription of diuretics to any patient diagnosed with CHF. Diuretics are indicated only for patients with CHF who have clinical signs and symptoms of excessive fluid retention in the body.
The features of diuretic therapy, its components and errors in prescribing certain diuretics will be discussed1.
In the practice of modern cardiologists and therapists in the treatment of heart failure, sufficient attention is paid to diuretic therapy. For the effective action of diuretics, it is important: entry into the body, adsorption and entry into the bloodstream, filtration and penetration into the renal tubules, active influence on specific transporters (electrolyte carriers in the apical membrane of renal tubule cells).
Table Classification of diuretics, their quality indicators
| Diuretics | Serum NH3- | Serum K+ | Serum pH | Complications |
| Thiazide: hypothiazide, indapamide | increases | is decreasing | > 7 | agranulocytosis, thrombocytopenia, anemia, pancreatitis, hepatic coma |
| Loops: furosemide, lasix, britomar, torasemide, ethacrynic acid | increases | is decreasing | > 7 | gastrointestinal bleeding, hyperglycemia, skin rash, hepatic coma |
| Potassium-sparing: spironolactone, veroshpiron, amiloride, triampur | increases | increases | < 7 | acidosis, gynecomastia, azotemia, hyperkalemia, hepatic coma |
| Osmotic: mannitol, urea | — | is decreasing | > 7 | hyperosmolar coma, hypoosmolarity |
| Carbonic anhydrase inhibitors | — | is decreasing | < 7 | urolithiasis, acidosis, hepatic coma |
Today, thiazide and loop diuretics . What is the difference?
Thiazide diuretics act on the cortical segment of the loop of Hengle in the area of the distal tubules, blocking the activity of the sodium-chloride transporter. Their effect on Na+ reabsorption and, therefore, on diuresis is moderate and is observed with normal renal function (creatinine clearance greater than 30 ml/min.). Thiazide diuretics suppress the reabsorption of sodium, increasing the excretion of it and other ions in the urine, they practically do not disturb the acid-base balance, compared with loop diuretics, they begin to act later (2 hours after administration, but have a longer effect (12–36 h), reduce glomerular filtration, reduce Ca+ excretion in the urine, do not have a “rebound” effect. They are indicated for edema of any level, hypertension, and diabetes insipidus.
Important! Thiazide diuretics are not prescribed for significant renal failure, severe diabetes mellitus, or gout with kidney damage.
The most powerful are loop diuretics , which block the activity of a special Na+/2Cl-/K+ transporter in tubular cells throughout the entire ascending segment of the loop of Hengle. The diuretic effect of loop diuretics is stronger and persists even with reduced renal function (with creatinine clearance not lower than 5 ml/min.). When using these diuretics, the effect occurs quickly and does not last long, so they require repeated doses throughout the day. It has been established that loop diuretics interfere with Na+ reabsorption and increase glomerular filtration. Loop diuretics are prescribed for edema caused by CHF, dysfunction of the liver, kidneys, and endocrine glands. They are indicated for edema of the brain, lungs, and to relieve hypertensive crises. The action of loop diuretics can provoke a pronounced deficiency of Na+ K+ Mg+ Cl- ions, dehydration, decreased tolerance to carbohydrates, and increased concentrations of uric acid and lipids in the blood serum. Ethacrynic acid may cause ototoxic effects.
Important! Loop diuretics are contraindicated in severe diabetes mellitus, uric acid diathesis, severe liver and kidney damage. These diuretics should not be used during lactation if you are intolerant to sulfonamide drugs.
RECOMMENDATIONS OF AN EXPERT
When using loop and thiazide diuretics in the blood, the concentration of cholesterol, beta-lipoproteins, and triglycerides increases, therefore, when prescribing diuretics, lipids in the diet should be limited, and, if necessary, combine them with angiotensin-converting enzyme inhibitors (ACE inhibitors). Another complication of treatment with loop and thiazide diuretics is hyperuricemia (increased levels of uric acid in the blood serum), in order to avoid it requires a corrective diet with limited purines, as well as the use of diuretics with ACE inhibitors. This combination - capozide + ACE inhibitors - is effective, both components enhance each other’s effect and is safe, because allows you to avoid many adverse reactions characteristic of diuretic therapy.
Diuretic treatment tactics include two phases: active and maintenance .
The task of the active phase is to eliminate excess accumulation of fluid in the body, manifested in the form of edema. In this phase, it is necessary to create forced diuresis, with urine excreted exceeding the fluid consumed by 800–1000 ml per day. In parallel, body weight should decrease daily by no more than 750–1000 g.
After achieving optimal dehydration, the patient is transferred to the maintenance stage of treatment. During this period, the amount of fluid drunk should not exceed the volume of urine excreted, and body weight should remain stable. The main thing in the maintenance phase of treatment is the daily use of selected doses of diuretics.
It is important to remember that the practice of prescribing “shock” doses of diuretics (once every few days) is flawed and is difficult for patients to tolerate. It is better to recommend the patient the drug “ Hypothiazide ” - 12.5-25 mg per day than 40-80 mg of the drug “ Lasix” once every 5 days.
In the latter case, the patient lives in a vicious cycle. He spends the day of taking the diuretic near the toilet due to excessive diuresis. On the 2nd day, the patient is completely overwhelmed, thirsty, and suffers from electrolyte imbalance (even to the point of seizures). On the 3rd day the patient begins to recover. On the 4th day he could feel cheerful, but over the days that have passed since the start of taking the drug, the accumulating fluid again causes overhydration and shortness of breath, which will require repeating the “shock” diuresis on the morning of the 5th day.
ALGORITHM FOR PRESCRIPTION OF DIURETICS DEPENDING ON THE SEVERITY OF CHF
- Functional class I (no edema) - you can do without diuretics;
- Functional class II (stagnation) - thiazide or loop diuretics are indicated in small doses, with a glomerular filtration rate of 30 ml/min. the use of thiazide diuretics is not recommended;
- III functional class (maintenance treatment) - loop diuretics + spironolactone are recommended;
- IV functional class - loop + thiazide diuretics + aldosterone antagonists are indicated.
INTERACTION OF DIURETICS WITH OTHER medicinal products, MECHANISM OF ACTION OF DIURETICS
In order to avoid unwanted effects, you must follow several recommendations:
- the combined use of thiazide diuretics and cardiac glycosides increases the toxicity of the latter due to hypokalemia;
- the combination of thiazide drugs with antihypertensives has an increased hypotensive effect;
- when diuretics are prescribed simultaneously with glucocorticoids, the likelihood of hyperglycemia is high;
- Furosemide increases the ototoxic effect of aminoglycosides, increasing the risk of developing glycoside intoxication;
- When loop diuretics are combined with nonsteroidal anti-inflammatory drugs (NSAIDs), the diuretic effect is weakened.
I am glad that the percentage of choice of Torasemide for initial therapy has become quite high - 68%, for Indapamide - only 13%. It is necessary to use new generation loop diuretics, such as Torasemide , Britomar, . It is noticed that:
- Torsemide is able to block aldosterone receptors.
In American studies, it was emphasized that there was a 56% reduction in re-hospitalization compared with the use of furosemide;
- the combination of thiazide and loop diuretics with ACE inhibitors leads to an increased diuretic effect.
ACE inhibitors can be prescribed to patients with CHF with a systolic pressure level above 85 mmHg. Art. At initially low blood pressure, the activity of ACE inhibitors remains. The prescription of ACE inhibitors is necessary with a gradual reduction in the starting dose. To exclude hypertension, the first dose of ACE inhibitors should be administered 24 hours after heavy diuresis;
- Spironolactone increases the concentration of cardiac glycosides in the blood and enhances the hypotensive effect of antihypertensive drugs.
With the simultaneous administration of spironolactone and non-steroidal anti-inflammatory drugs, the diuretic effect is reduced;
- ACE inhibitors, as an addition to the treatment of edema, not only improve the general condition of the patient, but also reduce the risk of hospitalization;
- normalization of the protein profile is necessary, namely the use of Albumin (200–400 ml/day), possibly together with diuretics, which increases the rate of their filtration;
- if the blood pressure level is sufficient, it is possible to additionally prescribe drugs that increase the glomerular filtration rate.
Only a third of surveyed doctors (30%) prescribe the maximum tolerated dose;
- if the absorption of the drug is impaired, the dose of the diuretic prescribed orally can be increased as desired, but success will not be achieved, and only transferring the patient to parenteral treatment will provide an adequate diuretic response;
- in case of systemic hypotension, the dose of diuretics and vasodilators should be increased no more than once a week;
- in case of intolerance to ACE inhibitors, sartan preparations that do not have indications for heart failure ( Eprosartan, Candesartan , etc.) should not be prescribed to patients with heart failure;
Only sartans in a number of studies have proven their effectiveness in patients with heart failure from functional classes I to IV. But you need to know that not all sartans have indications for heart failure ; only 59% of medical specialists know this;
- in practice, underestimation of heart rate control in patients with heart failure has been observed.
The good news is that 9 out of 10 doctors know that heart rate control is needed, but low doses of beta blockers, when the heart rate (according to outpatient records) is more than 70, the doses of beta blockers are not optimized in 76% of cases. The use of the drug Ivab Radin (Coraxan), the first representative of a new class of drugs - if-channel inhibitors, has increased the survival rate of patients with CHF;
- irresponsible ignorance of the role of mineralocorticoid receptors in the treatment of patients with heart failure. According to studies, it was found that 47% of surveyed doctors use drugs of this group ( Spironolactone ) in the treatment of heart failure from functional classes II to IV.
Summary. To achieve positive results in the treatment of CHF, the doctor should inform the patient about how and when to take medications, familiarize him with a list of recommendations, including the dose and frequency of taking each drug, and also give the patient an idea of the most common side effects of diuretics and the need for See a doctor if they occur.
—— 1 Prepared based on the introduction by Anna Ivanovna Chesnikova , Chairman of the Rostov Regional Research Society of Therapists, Doctor of Medical Sciences, Professor, at a symposium within the framework of the XI National Congress of Therapists