materials » Microscopes » Articles about microscopes, microspecimens and studies of the microworld » Human blood under a microscope
Have you ever wanted to see with your own eyes what human blood looks like under a microscope? After all, this is one of the most interesting tissues of the body! It consists of many cells of different types and performs vital functions: transport (carries oxygen throughout the body), protective (special cells eliminate harmful microorganisms) and homeostatic (maintains the constancy of the internal environment of the body).
In order for you to be able to see how human blood works, the microscope must provide at least 1000x magnification. Take this into account when choosing it.
What does blood look like under a microscope?
At high magnification, all three types of blood cells can be seen.
Red blood cells are disc-shaped red cells that transport oxygen throughout the human body. Diameter – 7–10 microns. The color of these cells is due to the content of hemoglobin, a special substance that allows them to carry oxygen molecules. These cells are the most numerous, therefore, when examining human blood under a microscope , you will see them first.
Leukocytes are round-shaped cells ranging in size from 7 to 20 microns. They form the immune system, which protects the body from pathogenic viruses, bacteria and fungi. There are several types of white blood cells: lymphocytes, monocytes, basophils, neutrophils and eosinophils.
Platelets are flat, colorless cells responsible for blood clotting. They have the smallest dimensions - from 2 to 4 microns - so they can only be examined in detail using a professional microscope.
Objectively about pseudoscientific. Dark Blood Fields: Diagnosis
4902 April 24
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Dark fields of blood: Diagnostics / Author: Alexey Vodovozov Source: / January 2010
Blood is an amazing creation of nature. It can be said without exaggeration that it is the source of life. After all, it is through the blood that we receive oxygen and nutrients, and it is through the blood that “production waste” is removed from the cells. Any illness is necessarily reflected in the blood. A number of diagnostic techniques are based on this. And charlatan ones too.
Blood was one of the first liquids that inquisitive doctors placed under the newly invented microscope. More than 300 years have passed since then, microscopes have become much more advanced, but doctors’ eyes still look at blood through eyepieces, looking for signs of pathology.
On glass
Antonie van Leeuwenhoek would definitely have received several Nobel Prizes had he lived today. But at the end of the 17th century this award did not exist, so Leeuwenhoek is content with the worldwide fame of the designer of microscopes and the fame of the founder of scientific microscopy. Having achieved 300-fold magnification in his instruments, he made many discoveries, including the first to describe red blood cells.
Leeuwenhoek's followers brought his brainchild to perfection. Modern optical microscopes are capable of magnification up to 2000 times and allow us to examine transparent biological objects, including the cells of our body.
Another Dutchman, physicist Fritz Zernike, noticed in the 1930s that the acceleration of light in a straight line makes the image of the model being studied more detailed, highlighting individual elements against a light background. To create interference in the sample, Zernike came up with a system of rings that were located both in the objective and in the condenser of the microscope. If you correctly configure (adjust) the microscope, then the waves that come from the light source will enter the eye with a certain phase shift. And this allows you to significantly improve the image of the object being studied.
The method was called phase-contrast microscopy and turned out to be so progressive and promising for science that in 1953 Zernike was awarded the Nobel Prize in Physics with the wording “For the justification of the phase-contrast method, especially for the invention of the phase-contrast microscope.” Why was this discovery so highly regarded? Previously, in order to examine tissues and microorganisms under a microscope, they had to be treated with various reagents—fixatives and dyes. It was impossible to see living cells in this situation; the chemicals simply killed them. Zernike's invention opened a new direction in science - intravital microscopy.
In the 21st century, biological and medical microscopes have become digital, capable of operating in different modes - both in phase contrast and in dark field (the image is formed by light diffracted by the object, and as a result the object appears very light against a dark background), as well as in polarized light, which often makes it possible to reveal the structure of objects that lies beyond the usual optical resolution.
It would seem that doctors should rejoice: a powerful tool for studying the secrets and mysteries of the human body has fallen into their hands. But this high-tech method was of great interest not only to serious scientists, but also to charlatans and scammers from medicine, who considered phase-contrast and dark-field microscopy a very successful way to extract certain amounts of money from gullible citizens.
She's alive and moving
From a patient who decides to undergo examination using the “Living Drop of Blood Diagnostics” method (variants of the name are “Testing on a dark-field microscope” or “Hemoscanning”), a drop of blood is taken, not stained, not fixed, applied to a glass slide and studied by viewing the sample on the monitor screen. Based on the results of the study, diagnoses are made and treatment is prescribed.
Hemoscanning can be considered the crowning achievement of fraudulent thought, a masterpiece and the highest aerobatics of near-medical quackery. Firstly, a real existing physical phenomenon is used (remember about the Nobel Prize?) and real complex medical equipment. And really expensive. The cost of a diagnostic complex costs at least 3–4 thousand dollars, and it is sold by reputable suppliers of serious medical equipment. The equipment has all the necessary - genuine and completely deserved - certificates and certificates. Secondly, no problems with licensing. Laboratory diagnostics is a completely legitimate type of medical activity, and a microscope that allows phase-contrast or dark-field microscopy is a completely legitimate medical diagnostic equipment. Moreover, it is widely used in medicine, that is, there are certified and certified specialists. Thirdly, under a microscope you can indeed detect a lot of signs of certain diseases. For example, changes in the shape of red blood cells in sickle cell anemia. You can also see intracellular parasites, all in the same red blood cells, called Bartonella. And even helminth eggs can theoretically be detected in the blood.
I see arba - I sing arba
So what's the catch? In interpretation. In how the “Dark Polish people” explain certain changes in the blood, what the discovered artifacts are called, what diagnoses are made and how they are treated. It is difficult even for a doctor to figure out that this is a hoax. You need special training, experience working with blood samples, and hundreds of examined “slides” – both stained and “live.” As in a regular field, so in a dark one. Fortunately, the author of the article has such experience, as does the experts with whom the results of the investigation were verified.
It’s rightly said – it’s better to see once. And a person will believe his own eyes much faster than all verbal exhortations. This is what the “laboratory assistants” are counting on. A monitor is connected to the microscope, which displays everything that is visible in the smear. When was the last time you saw your own red blood cells? That's it. It's interesting. And while the fascinated visitor admires the cells of his own beloved blood, the “laboratory assistant” begins to interpret what he sees. Moreover, he does this according to the principle of akyn: “I see an arba, I sing an arba.” Read in detail in the sidebar about what kind of “arba” charlatans can sing about.
After the patient is frightened and confused by incomprehensible, and sometimes downright scary pictures, he is given “diagnoses”. Most often there are many, and one is more terrible than the other. For example, they will tell you that the blood plasma is infected with fungi or bacteria. It doesn’t matter that seeing them even at such magnification is quite problematic, much less distinguishing them from each other. Microbiologists have to sow pathogens of various diseases on special nutrient media, so that later they can say exactly who has grown, what antibiotics they are sensitive to, etc. Microscopy is used in laboratory research, but either with specific dyes or even with fluorescent antibodies that attach to bacteria and thus make them visible.
But even if, purely theoretically, such a giant of the bacterial world as Escherichia coli (1–3 microns long and 0.5–0.8 microns wide) is found in the blood under a microscope, this will mean only one thing: the patient has sepsis, infection blood. And he should lie horizontally with a temperature of under 40 and other signs of a serious condition. Because normally blood is sterile. This is one of the main biological constants, which is checked quite simply by inoculating blood on various nutrient media.
They may also tell you that the blood is “acidified.” A shift in the pH (acidity) of the blood, called acidosis, does occur in many diseases. But no one has yet learned how to measure acidity by eye; you need contact between the sensor and the liquid being tested. They can detect “toxins” and tell you about the degree of slagging in the body according to WHO (World Health Organization). But if you look through the documents on the official website of this organization, there is not a word about either slags or the degree of slagging. Diagnoses may include dehydration syndrome, intoxication syndrome, signs of fermentopathy, signs of dysbacteriosis and a host of others that are not related either to medicine or to this particular patient.
The apotheosis of diagnosis, of course, is the prescription of treatment. By a strange coincidence, it will be carried out with biologically active food additives. Which, in essence and by law, are not medicines and cannot be treated in principle. Especially such terrible diseases as fungal sepsis. But this does not bother hemoscanners. After all, they will not treat the person, but the very diagnoses that were given to him out of thin air. And with repeated diagnostics, rest assured, the indicators will improve.
What you can't see with a microscope
No matter what the “experts” tell you, using a microscope you cannot see the pH of the blood in a drop of blood taken from your finger; deficiency of enzymes for protein breakdown; level of water-salt metabolism; food mutagenic/teratogenic toxins; damage to red blood cells by kidney toxins/free radicals; parasites, fungi, bacteria, worm eggs, cysts; activity, quantity and quality of immune cells.
Live blood testing originated in the United States in the 1970s. Gradually, the true essence and value of the technique became clear to the medical community and regulatory authorities. Since 2005, a campaign has begun to ban this diagnosis as fraudulent and unrelated to medicine. “The patient is deceived three times. The first time is when a disease that does not exist is diagnosed. The second time is when a long and expensive treatment is prescribed. And the third time is when a repeat study is falsified, which will necessarily indicate either an improvement or a return to normal” (Dr. Stephen Barrett, vice president of the American National Council Against Medical Fraud, scientific consultant to the American Council on Science and Health).
Are bribes smooth?
Proving that you were deceived is almost impossible. Firstly, as already mentioned, not every doctor will be able to suspect forgery in the technique. Secondly, even if the patient goes to a regular diagnostic center and they don’t find anything there, you can, as a last resort, blame everything on the operator who performed the diagnostics. Indeed, the visual assessment of complex images depends entirely on the qualifications and even the physical condition of the person doing the assessment. That is, the method is not reliable, since it directly depends on the human factor. Thirdly, you can always refer to some subtle matters that the patient cannot understand. This is the last frontier where all medical scammers usually face their death.
What do we have in the bottom line? Unprofessional laboratory technicians who pass off random artifacts (maybe even orchestrated) in a drop of blood as terrible diseases. Then they suggest treating them with nutritional supplements. Naturally, all this for money, and quite a lot.
Does this technique have diagnostic value? It has. Undoubtedly. The same as traditional smear microscopy. You can see, for example, sickle cell anemia. Or pernicytosis anemia. Or other really serious illnesses. But, to the great regret of scammers, they are rare. And you can’t sell crushed chalk with ascorbic acid to such patients. They need real treatment.
And so - everything is very simple. We discover a non-existent disease and then successfully cure it. Everyone is happy, especially the citizen over there, who had a fragment of the bell-mosquito’s space communications antenna expelled from his blood... And no one feels sorry for the money that was wasted, or rather, to enrich the swindlers.
However, not everyone. Some defend their rights in all possible instances. The author has at his disposal a copy of a letter from the Office of Roszdravnadzor in the Krasnodar Territory, where victims of hemoscanning “doctors” turned. The patient was diagnosed with a bunch of diseases that were proposed to be treated with no less than a bunch of biologically active food supplements. Based on the results of the inspection, it turned out that the medical institution that carried out the diagnostics violated licensing requirements, did not enter into an agreement for the provision of paid services (the doctor takes money in cash), and the rules for maintaining medical records were violated. Other violations were also identified.
I would like to end the article with a quote from a letter from the Central Office of Roszdravnadzor: “The 'Hemoscanning' technique was not submitted to Roszdravnadzor for consideration and permission to use as a new medical technology and is not permitted for use in medical practice.” Couldn't say it any clearer.
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor.
Blood smear: execution and research algorithm
N. Puletti
The production of blood smears is technically simple and fast. To obtain maximum information, the assessment of blood cells must be systematized.
In practice, it is not always possible to obtain sufficient objective data when using hematological rapid diagnostics. Examination of blood smears allows one to relatively quickly clarify and supplement the information received. This method allows you to identify some elements that are not apparent during automated clinical blood tests (for example, changes in the shape of red blood cells, a shift in the leukocyte formula to the left [towards immature neutrophils], or the presence of parasites in the blood). In some cases, this method allows a definitive diagnosis to be made.
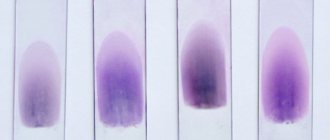
| Drawing. Different layers of a blood smear. Cells are assessed under a microscope in a thin layer of smear on the pigtails using the shuttle method |
Preparation and staining of blood smears
When collecting material from an ideally calm animal with an average diameter of the vein widening, the blood should quickly flow into a tube containing an anticoagulant. EDTA (ethylenediaminetetraacetate) is most often used because this anticoagulant allows for better preservation of the blood cells being studied. However, to prevent various types of morphological degradation of cells, the time interval between the collection of fresh and well-homogenized blood and the preparation of the drug should be as short as possible (JW Harvey, 2001; D. Walker, 2008).
| Photo 1a. Preparing a blood smear. A small drop of blood is placed on the end of a glass slide using a microcapillary | Photo 1b. Preparing a blood smear. The drop is smeared by placing a second slide at an angle of approximately 45° relative to the first |
Preparation of smears begins by taking a drop of blood (usually one from a capillary tube) onto the edge of a slide. Then the drop is smeared using a second glass, which slides over the first (photos 1a and 1b). A well-prepared blood smear has a so-called “cat tongue” at the end. It indicates that the sample was performed correctly and allows for a high-quality blood examination (figure). Painting is carried out using the standard method (Diff-Quick®, RAL®, Wright-Giemsa®). Before staining, the prepared smear is dried in air by shaking the slide, which avoids the formation of a light unstained zone in the center of the red blood cells and, accordingly, eliminates the erroneous interpretation of hypochromia (photo 2) (D. Walker, 2008). Other coloring artifacts may exist. For example, Wright staining produces a precipitate if the stain is not renewed after a period of time, if the slide was left in the staining solution for a long time, or if it was poorly washed after staining (photo 3) (D. Walker, 2008). As a result, the accumulation of dye can be interpreted as the presence of bacteria or parasites in the blood. In addition, smear staining and cell morphology may be altered when the slide is exposed to formaldehyde fumes. Typically, blood smears are stained using the Romanowsky method (Wright® or Wright-Giemsa®), based on eosin and methylene blue.
| Photo 2. Microscopy of a dog’s blood smear (×1000). In some red blood cells, white light refractions appear in the center (arrows). These are artifacts caused by poor drying of the slide before staining. | Photo 3. Microscopy of a dog’s blood smear (×500). The coloring artifact can be confusing, resembling parasites or bacteria |
Classic coloring differs from fast coloring. Recently, quick dyeing methods such as Diff-Quick® have been advantageous because they are resistant to variations in pH of solutions and the formation of dye deposits. However, they are less effective at detecting polychromatophils and do not stain basophil and mast cell granules well (JW Harvey, 2001; D. Walker, 2008). To obtain a specific visual pattern of reticulocytes, it is necessary to stain with new methylene blue (NBM). In a plastic test tube, a drop of blood is mixed with two drops of NBM. The test tube is left at room temperature for 10 minutes. After mixing, a small drop is placed on a glass slide and smeared in the same way as when performing a blood smear. The slide is then quickly air dried and examined under a high magnification microscope (×50–×100).
Systematic examination of blood smears
When assessing a blood smear, it is very important to be guided by a single research scheme.
A blood smear, made in one thin (monocellular) layer with a roundness at the end, thickens towards the base. Blood cells are assessed on a thin layer, because a thick layer carries little information. At low magnification (×10 or ×20), the edge of the smear, mainly the rounded end, is usually examined for platelet aggregates or broad atypical cells (lymphoblasts or dendritic cells) (Figure 4). Platelet aggregates after their activation are formed in vitro. This phenomenon sometimes occurs as a result of difficult blood sampling, which, for example, is most often noted in cats (E. Duan Lassen, G. Weiser, 2006; SL Stockhman, MA Skkott, 2008; D. Walker, 2008).
| Photo 4. Microscopy of a blood smear of a healthy dog (× 1000). Platelet clots |
The thin layer can have the shape of zigzags or braids, which allows you to very clearly observe different blood cells during a targeted study using the APEL algorithm (A - other [for example, atypical cells, blood parasites]; P - platelets; E - erythrocytes; L - leukocytes).
Blood smear testing is a fairly common method that can quickly diagnose many common disorders in dogs and cats. The main conditions for the effective use of this diagnostic method are strict adherence to the smear preparation technique and systematic research in compliance with the research algorithm.
Basic provisions
— After collecting the material, the blood should be quickly placed in a tube with an anticoagulant in order to preserve the quality of the cells.
— New methylene blue stain allows identification of reticulocytes.
— The assessment is carried out on a thin layer of blood smear with reading under a microscope at the level of its pigtails.
— Systematic blood smear examination refers to the APEL algorithm.
SVM No. 5/2010
Rate material
Like Like Congratulations Sympathy Outrageous Funny Thoughtful No words
2
Gynecological smear “for flora”: what to look for and how to understand
Most women are familiar with the “flora” smear as the “simplest” gynecological test. However, the research is much more “useful” than it might seem. And just a few (or even one) deviations can highlight significant problems, even before any symptoms appear. So how can we understand the results? Let's talk point by point.
Epithelium
As you know, any living object in nature has a limited lifespan, after which it dies “of old age.”
The epithelium in a gynecological smear is the desquamated “old” cells of the mucous membrane of the vagina, cervical or urethra (depending on the locus being assessed). Which may be present in the material in moderate quantities.
Exceeding regulatory limits (“a lot” or “copiously”) may indicate:
- inflammation, due to which cells are destroyed at an “increased volume”,
- or excess estradiol, which stimulates proliferation (division and growth) of epithelial cells, thereby increasing their total number.
A decrease or absence of epithelium in a smear indicates atrophic changes, a lack of estradiol or an excess of androgens.
In addition, due to the dependence of the epithelium on the level of sex hormones, its amount in the material can vary greatly depending on the day of the cycle, from a single “in sight” at the very beginning to a moderate and even large amount closer to and during ovulation.
And the appearance in the smear of so-called “key cells” (epithelium “covered” with small coccal bacteria) is a marker of bacterial vaginosis.
Leukocytes
The “norm” of leukocytes in a smear also greatly depends on the stage of the cycle and the level of sex hormones, as well as the locus being studied.
So, for the “maximum” for:
- vagina taken 10,
- cervical canal – up to 25,
- and in the urethra - no more than 5 leukocytes in the field of view.
An increase in the indicator obviously indicates inflammation, and a complete absence can normally occur at the very beginning of the cycle.
Slime
The result “absent”, “little” or “moderate” for this indicator is the norm, which is also associated with individual hormonal characteristics and the cycle.
But “a lot” of mucus in the smear may indicate that the smear was taken in the middle of the cycle, dysbiotic changes or excess estrogen. Therefore, it requires the attention of a specialist or, at a minimum, monitoring over time.
Flora
The predominant flora of the female genital tract normally in women of reproductive age is known to be lactobacilli (or Dederlein bacilli). The amount of which can be from moderate to abundant, depending, among other things, on the phase of the menstrual cycle.
The detection of “mixed, predominantly rod-like” flora in a smear is also a normal option. True, if these same rods are “small, polymorphic,” that is, they morphologically correspond to lactobacilli.
The predominance of coccal flora in the smear, and especially if its amount is “abundant”, is a sign of pronounced dysbiotic disorders. Which requires a more detailed assessment of the quality of the microflora and, importantly, the relationship between its representatives (for example, the Femoflor-16 analysis). Since it is associated with many reproductive pathologies (including hidden ones).
Pathological elements
The presence of fungal mycelium, trichomonas, diplococci (including the causative agent of gonorrhea), leptothrix, mobiluncus and other pathogenic microorganisms in a normal smear is not allowed, even in minimal quantities. And their identification is a serious reason to immediately seek treatment.