Tasks of eosinophils
The main task of eosinophils is the elimination of foreign harmful agents.
Their destruction occurs at the extracellular level; their capabilities also include the elimination of fairly large organisms. The effect begins when the contents of intracellular granules are released. Compared to neutrophils, the ability for phagocytosis in the agents we are considering is less, but it is still present. This is not their main task, but they can destroy and absorb germs. Let us list the main functions of eosinophilic granulocytes:
- They have a toxic effect on helminths.
- Eliminate the effect of biologically active substances that cause allergies.
- They help eliminate the consequences of the activity of bioactive substances that were produced by mast cells and basophils. The latter are the main causative agents of an allergic reaction. They also influence the development of severe forms of the disease - Quincke's edema and anaphylactic shock.
- Develop a highly sensitive reaction.
- Awaken activity to kill bacteria.
- Eliminate foreign cells by absorbing them.
Eosinophils fight allergens, leading to stabilization of the child or adult's condition
The role of basophils in the body
Basophils are a separate group of leukocytes that play an important role in human life.
They are formed in the hematopoietic organs, from where they spread throughout the circulatory system. The main task of basophilic leukocytes is to protect the body from the harmful effects of an aggressive environment and normalize metabolism. The role of basophil cells for humans:
- neutralization of allergens from the external environment;
- blocking the entry of toxins and their movement in the general bloodstream;
- maintaining immunity;
- normalization of blood flow;
- fight inflammation;
- regulation of metabolic processes in the skin;
- participation in normal blood clotting.
When an inflammatory process occurs, basophils are released from blood cells and rush to the affected areas - their number in the bloodstream decreases. With prolonged inflammation, their number, on the contrary, increases, because the bone marrow begins to actively produce the necessary cells in response to the disease.
Basophils help stop bleeding and participate in the production of heparin, which is responsible for this function. They provide significant support to children's immunity, preventing harmful substances from spreading throughout the body.
Normal indicator for children
Eosinophilic granulocytes are part of the leukocyte formula of blood. Determining their number is easiest and most reliable using a general blood test.
READ ALSO: blood formula in children: normal Normal indices of eosinophilic cationic protein can fluctuate, which is directly related to age. In children, the number of eosinophilic granulocytes is higher than in adults. So, in newborn babies - up to 8%, in older children - up to 5-6%.
The indicators that determine the norm will vary depending on the laboratory conducting the study. This is influenced by the reagents used, equipment and units of measurement adopted in a particular medical institution. Most laboratories measure the eosinophilic granulocyte count as a percentage of the total white blood cell count. Those. As a result, we see not the total number of cells, but their proportion among leukocytes.
It is important to keep in mind that the result obtained is relative. Based on this technique, eosinophilic granulocytes normally comprise:
- for newborns – from 1 to 6-8%;
- for infants from 15 days to a year – 1-5%;
- 1-2 years – 1-7%;
- 205 years – 1-6%;
- 5-15 years – 1-4%;
- over 15 years of age – up to 5%.
In infancy, eosinophil levels are the highest.
Existing tables allow you to independently determine whether the test result is normal or if there are abnormalities. To calculate the absolute number of eosinophilic granulocytes in the blood, the following unit of measurement is taken as a basis: 10^9/l.
The following indicators are considered the norm:
- from birth to one year – 0.05-0.4;
- from 1 year to 6 years – 0.02-0.3;
- for children over 6 years old and adults – 0.02-0.5.
Diagnostics and necessary tests
If you detect a deviation from the norm in basophils, you should not panic, however, there is no need to delay visiting a doctor. There is a possibility that the situation will normalize on its own, but in no case should you miss the disease at its initial stage.
A specialist will be able to determine the reason for the increase or decrease in basophils in the blood after examining the baby and additional research. If necessary, the child will be sent for consultation to a pediatric hematologist. Further examination and treatment depend on the preliminary diagnosis and the patient’s condition.
A blood test is taken from a finger or a vein. To obtain a reliable research result, you need to properly prepare for it:
- donate blood in the morning on an empty stomach (do not eat for 8 - 10 hours, for children of the first year of life - 2 hours);
- follow a diet, the evening before the test, exclude heavy and fatty foods from the diet;
- Do not drink sweet tea or coffee before the procedure; you can drink plain water;
- do not take medications, having warned your doctor in advance;
- Avoid excessive physical activity and stress before donating blood.
Indicators indicating an increase in level
For different ages, the norm of eosinophils in the blood of children will also be different. Compared to adults, their number is slightly higher in children, since the child’s immunity is just developing. Normal laboratory values are as follows:
- In newborns – 1-6
- In children under two weeks of age – 1-6
- From two weeks to one year – 1-5
- From one to two years – 1-7
- From two to five years – 1-6
- From six to sixteen years old – 1-5
If the indicators are higher, then this condition is called eosinophilia. It’s not very good when the analysis showed low eosinophils in the child’s blood. This may signal the initial stage of inflammation, a stressful condition, a purulent infection, or poisoning with any heavy metals or chemicals.
- Why are eosinophils in the blood low, what does this mean?
Blood test for ARVI
When a child has a fever, cough and runny nose, parents want to be sure that this is a common ARVI and not a bacterial infection. Sometimes it seems to them that a general blood test will dot the i's - as soon as they take it, it will immediately become clear what the child is sick with and whether they need to give him antibiotics. However, this is not quite true. In some cases, a blood test will actually help the doctor make a diagnosis, but most often it is not necessary. In addition, the result obtained, where half of the indicators go beyond the norm, only needlessly scares parents. Pediatrician Alexandra Zhukovskaya talks about why you shouldn’t rush to get a blood test at the first symptoms of the disease.
What indicators can change during infection?
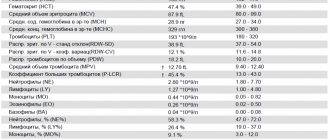
First of all, the total number of leukocytes changes - these are the cells that protect the body from viruses and bacteria. There are several types of white blood cells that perform different tasks: neutrophils, lymphocytes, monocytes, eosinophils and basophils. Their number and relationship to each other are displayed in the leukocyte formula - usually as a percentage. As soon as one indicator increases slightly, the rest will automatically decrease. This is why, with minor changes in the leukocyte formula, the forms look frighteningly red. In addition, in many laboratories, the forms indicate standards for adults, which differ from children. Thus, in children under 5 years of age, lymphocytes predominate, in older children - neutrophils, and the total number of leukocytes changes with age.
What do deviations mean?
With a bacterial infection, you usually experience:
- increase in the number of leukocytes (leukocytosis) - more than 15 × 10⁹/l;
- increase in the absolute* number of neutrophils - more than 10 × 10⁹/l;
- a shift in the leukocyte formula to the left - that is, the appearance of immature (band) forms of neutrophils - more than 1.5 × 10⁹/l.
*To estimate the absolute neutrophil count, you need to know the total white blood cell count and the percentage of neutrophils. For example: leukocytes are 9 × 10⁹/l, and neutrophils make up 72%, which is usually already highlighted in red. We count: 9 × 72/100%, we get 6.5 - that is, the normal absolute number of neutrophils.
With a viral infection, you usually experience:
- Decrease in the total number of leukocytes (leukopenia) - especially with influenza, measles, etc.
- Increased absolute number of lymphocytes (lymphocytosis).
- The appearance of “atypical” cells occurs in infectious mononucleosis.
Another nonspecific sign of inflammation is an increase in erythrocyte sedimentation rate (ESR). High ESR is typical for both viral and bacterial infections.
What then causes difficulties?
The fact is that in the first days of the disease there may not yet be any characteristic changes in the general blood test, or vice versa - the leukocytes may “jump” significantly even for a banal viral infection, casting doubt on the diagnosis. Many viruses (adenovirus, Epstein-Barr virus) lead to a persistent increase in the number of white blood cells - leukocytosis - which is usually associated with a bacterial infection.
Conversely, some bacterial diseases occur without abnormalities in blood tests - for example, otitis media or atypical pneumonia, or even with changes characteristic of a viral infection - for example, lymphocytosis is observed in whooping cough.
There are quite a few such exceptions, which is why at the beginning of the disease a general blood test cannot be a universal diagnostic method - the doctor will receive much more information during a thorough examination of the child.
How else can you clarify the diagnosis?
If the doctor suspects streptococcal sore throat or influenza, a streptate test or rapid test for influenza is performed. Methods are available to detect many viruses in saliva, nasal secretions, etc. A chest x-ray is indicated to rule out pneumonia. If a urinary tract infection is suspected, urine test strips and urine tests are performed. In case of severe intestinal infections, feces are examined for the presence of bacteria belonging to the intestinal group (salmonellosis, dysentery, etc.). If the child has been feverish for a long time and there is no obvious source of infection, the levels of C-reactive protein and procalcitonin are looked at in a biochemical blood test. Some time after the onset of the disease, specific antibodies against various infectious agents can be detected in the blood.
Isn't it easier to give an antibiotic right away?
No.
- Antibiotics are ineffective against viruses and cannot prevent bacterial complications, but vaccination against pneumococcus and other bacterial infections can cope with this.
- Antibacterial therapy disrupts the vital activity of normal microflora involved in protection against foreign and dangerous microorganisms.
- Taking antibiotics without indications leads to antibiotic resistance—bacterial resistance. This means that the next time an antibiotic is actually needed, it will no longer be harmful to the bacteria, and the disease will be more difficult to cure.
- For some viral infections (for example, infectious mononucleosis), the administration of widely used penicillin antibiotics leads to the appearance of a rash. This is often interpreted as an allergic reaction, although there are no contraindications for further use of this group of antibiotics in a child.
- All medications, including antibacterial drugs, have side effects. The benefit of any intervention should be greater than the potential harm - you should not break this rule by giving antibiotics “just in case”.
Norms of eosinophils in children
To find out whether a child’s eosinophils are elevated or not, you need to know what the norm is. Its indicators vary depending on the age of the child. Since eosinophils are often recorded as a percentage, the figures for different age groups are as follows:
- from birth to two weeks – 1–6%;
- from two weeks of age to one year – 1–5%;
- 1–2 years – 1–7%;
- 2–4 years – 1–6%;
- 5–18 years – 1–5%.
As can be seen, eosinophils may be present in the blood in small quantities. This is normal and does not require correction.
What are basophils and how do they work?
There are constantly a large number of different particles in the bloodstream, including different groups of leukocytes, each of which has its own purpose. The main purpose of basophils is to recognize foreign agents and particles in the body that may be potentially harmful to health. After recognition, these bodies attract a large number of other blood particles, including lymphocytes, which are capable of destroying a suspicious object.
If basophils are elevated in a child, it is necessary to conduct an examination
- What are the norms of basophils in the blood?
The formation of these blood cells occurs in the bone marrow tissue, but basophils make up no more than 1% of the total number of leukocytes. These particles penetrate into the bloodstream within two hours after formation, and then spread to the organs and tissues of the body. The lifespan of each such cell is only 11–12 days, which is quite a bit. But at the same time, they are necessary for maintaining health and are involved in many important processes, in particular:
- help improve blood flow, normalizing the movement of blood through the vessels and speeding it up if necessary;
- help form new capillaries, which promotes better saturation of tissues with various nutrients and oxygen;
- protect the intestinal walls;
- help other types of leukocytes move along the bloodstream;
- necessarily participate in all manifestations of allergies and in any inflammatory processes.
Etiology
An increase in eosinophils in a child has the following pathological causes:
- allergic reactions;
- helminthic infestations;
- lack of magnesium;
- immunodeficiency states;
- systemic diseases;
- infectious and viral diseases;
- chronic skin diseases;
- dysfunction of the thyroid gland;
- diseases of the upper respiratory tract, most often pneumonia;
- extensive thermal burns;
- poisoning with toxic substances;
- congenital diseases of the cardiovascular system;
- increased tone of the vagus nerve;
- polycythemia;
- tuberculosis;
- vasculitis;
- Infectious mononucleosis;
- benign tumors;
- oncological processes.
In addition, eosinophils in the baby’s blood can be increased with long-term use of drugs of this type, such as sulfonamides, nitrofurans, hormones and antibiotics.
The reasons that eosinophils are higher than the permissible number can only be established through diagnostic measures, since this process does not have a specific clinical picture.
Reasons for the increase
If, during a study, an increase in the concentration of basophils is detected in the baby’s blood, it is necessary to accurately determine the factor that led to such a situation and take adequate measures. Most often, an increased content of these particles can be caused by the presence of helminths in the baby’s body, a developing infection, the accumulation of toxic compounds, and the penetration of allergens. However, some diseases can also provoke an increase in concentration, for example:
- various pathologies and blood diseases, including myeloid leukemia;
- active inflammatory process, both obvious and hidden;
- infectious diseases;
- negative effects of different types of radiation - in particular, the concentration of particles may increase slightly after a routine x-ray examination;
- the development of an allergic reaction when a particular irritant enters the body;
- disturbances in the functioning of different types of glands related to the endocrine system;
- anemia of any kind.
An increased content of basophils is determined by a general blood test
If basophils are elevated in a child, it is necessary to consult a doctor, undergo a comprehensive examination and accurately determine the factors that provoked the occurrence of such a situation. It is necessary to correctly diagnose and establish exactly what this means in order to take the necessary measures and help the baby in a timely manner. The examination cannot be postponed.