Heart rhythm disorders (arrhythmias) are conditions in which the heart beats irregularly, too fast, or too slow. With frequent heart contractions - above 100 beats per minute in adults, this condition is called tachycardia, with rare - less than 60 beats per minute, it is called bradycardia. Some types of arrhythmia have no symptoms. If the arrhythmia is symptomatic, then the main complaints are palpitations or a feeling of a pause between heartbeats. Sometimes patients may complain of dizziness, fainting, shortness of breath or chest pain. Most types of arrhythmia are not a serious threat to the patient, but complications such as stroke or heart failure can often occur, and sometimes the arrhythmia can lead to cardiac arrest.
The Innovative Vascular Center employs experienced cardiologists who will help determine exactly why cardiac arrhythmia occurs and prescribe the correct treatment. In addition to drug therapy, our clinic implants artificial pacemakers (pacemakers) of any configuration. Timely and correct treatment allows our patients to avoid many complications, which means prolonging life and improving its quality.
Slow heartbeat - bradycardia
Bradycardia is a condition where the heart beats so slowly that it cannot pump enough blood to meet the body's needs. If bradycardia is left untreated, it can lead to extreme fatigue, dizziness, or fainting because not enough blood is supplied to the brain. This condition can be corrected by using an electronic pacemaker, which makes the heart beat normally.
Bradycardia occurs for various reasons:
- Sick sinus syndrome
The appearance of sinus bradycardia as a result of a “malfunction” in the sinus node (the natural pacemaker of the heart) occurs when discharges for contractions occur too infrequently. A weak sinus node can develop with age or be a consequence of illness. Some medications may also cause or worsen bradycardia. This arrhythmia may be temporary or permanent. It can be treated with medications or an electronic pacemaker.
- Blockage of the heart pathways
Heart block is a slowing or interruption of the electrical signal to the lower chambers of the heart (ventricles) that cause the heart muscle to contract. The heart's electrical conduction system typically sends signals from the upper chambers of the heart (atria) to the lower chambers (ventricles), which causes coordinated contractions of the heart muscle. Complete blockade of the atrioventricular node can manifest as a sudden loss of consciousness, since the ventricles contract very rarely without stimulus from the sinus node. An artificial pacemaker can eliminate this problem and normalize heart function.
What's the forecast?
The prognosis for life with atrial fibrillation is determined primarily by the causes of the disease. For example, for survivors of acute myocardial infarction and significant cardiosclerosis, the short-term prognosis for life can be favorable, but for health in the medium term unfavorable, since in a short period of time the patient develops chronic heart failure, which worsens the quality of life and shortens it duration.
However, with regular use of medications prescribed by a doctor, the prognosis for life and health undoubtedly improves. And patients with a permanent form of MA registered at a young age, with proper compensation, live with it for up to 20-40 years.
Rapid heartbeat - tachycardia
- Supraventricular tachycardia
This is a rapid heartbeat in the atria (upper chambers of the heart) or in the atrioventricular (atrioventricular) node, the electrical connection between the atria and ventricles. The first signs of atrial fibrillation are usually detected on an ECG. Atrial fibrillation can be permanent or paroxysmal (periodic) in form, which determines the approach to treatment. Sinus tachycardia is a rapid heartbeat with the formation of regular complexes on the ECG. Sinus arrhythmia is usually associated with an emotional background, elevated temperature, endocrine diseases of the thyroid gland, as well as a predominance of the sympathetic autonomic nervous system.
- Atrial flutter
For atrial flutter to occur, an additional or early electrical impulse must move around the atrium in a circular path rather than along its normal path. This electrical signal causes the atria to contract very quickly, which is usually not life-threatening, but can cause chest pain, dizziness, or other more serious problems. Many chronic heart diseases lead to the development of flutter and atrial fibrillation - its variety.
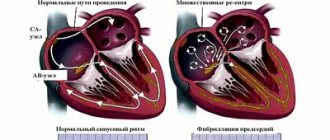
- Atrial fibrillation
Coronary heart disease often leads to arrhythmia. This common form of tachycardia is more common in women and occurs when there is excess electrical activity in the atria that is extremely disorganized. The manifestation of this electrical activity is very frequent and chaotic contractions of the atria. The atria lose their contractile function, which leads to stagnation of blood in them and can contribute to the formation of clots. Blood clots are the main cause of complications and danger of atrial fibrillation, since they can break away from the atria and enter the general bloodstream. Such a blood clot can cause a blockage of any artery in the body (embolism), leading to a stroke or gangrene of the limbs.
- Paroxysmal supraventricular tachycardia (PSVT)
With PSVT, heart rate increases from 140 to 250 beats per minute (the norm is 60-90 beats per minute). Why does this condition happen, cause trouble, but rarely life-threatening? The causes of this type of cardiac arrhythmia are associated with congenital additional electrical pathways between the atria and ventricles. Idiopathic supraventricular tachycardia is treated by destroying additional electrical pathways using radiofrequency ablation. Tachycardia is felt as an increased heartbeat and is very worrying for patients.
- Wolff-Parkinson-White syndrome (WPW)
In people with Wolff-Parkinson-White syndrome (WWS), extra, abnormal electrical pathways in the heart lead to periods of very fast heartbeat (tachycardia). Most people with WPW syndrome can lead normal lives. Many have no symptoms and no episodes of tachycardia. In some people, WPW syndrome can cause a rapid heartbeat (paroxysmal supraventricular tachycardia), when the heart rate rises to 240 beats per minute (normal is 60 to 80 beats per minute). Other symptoms include palpitations, shortness of breath, fainting, and angina (chest pain) with exercise. The first symptoms of this form of cardiac arrhythmia do not always require treatment, but a thorough examination by a cardiologist is necessary.
- Ventricular tachycardia
Ventricular tachycardia occurs when the ventricles (lower chambers of the heart) contract too quickly, making this arrhythmia life-threatening. This condition can be very serious as the ventricles are responsible for pumping blood to the rest of the body. If the tachycardia becomes so severe that the ventricles cannot pump blood effectively, it can be life-threatening. Tachycardia can be treated with medications. Other procedures include implantation of a defibrillator, catheter radiofrequency ablation, or surgical removal of the heart's accessory pathways. Ventricular extrasystole is a cardiac arrhythmia, which manifests itself as a sudden strong interruption in the functioning of the heart. It is clearly visible on the ECG and interrupts the normal heart rhythm. Bigemeny is one extrasystole every normal cardiac cycle. Trigemeny - extrasystole after two normal cycles. This poor prognostic sign is of great importance and requires immediate attention to a cardiologist.
- Ventricular fibrillation
Erratic and inefficient contractions of the ventricles occur when the electrical signal that normally causes the heart to beat breaks up and travels along random paths around the ventricles instead of following its normal route. The result is a series of rapid but ineffective contractions of the ventricles, leading to loss of consciousness as a result of a sharp drop in blood pressure. This means that without emergency treatment, fibrillation becomes fatal, as it turns off the pumping function of the heart and stops blood circulation. Fibrillation can be stopped with an electric shock or a blow to the heart using a defibrillator. The discharge allows you to “reset” the electrical activity of the heart and return to normal rhythm. Ventricular fibrillation occurs with myocardial infarction, severe chronic heart disease, hemorrhagic shock, and intracardiac procedures.
Methods for diagnosing arrhythmia
To diagnose arrhythmia, the following are used:
ECG
An ECG is a simple and informative study that allows the doctor to obtain the necessary information about the rhythm of the heart muscle. The electrocardiogram shows whether there is an arrhythmia or not, and if there is, an ECG will determine the type of arrhythmia.
More information about the diagnostic method
Holter monitoring
Holter monitoring is used to diagnose arrhythmia and monitor the progress of its treatment. A device is attached to the patient’s body that records heart activity throughout the day. At the same time, the person leads his usual lifestyle (the only thing is that the device cannot be wet). The monitoring results are then processed on a computer. This method makes it possible to identify episodes of arrhythmia caused by habitual daily exercise - this does not require being seen by a doctor at that very moment.
Echocardiography
Echocardiography for arrhythmia is carried out to identify functional and morphological changes in the heart.
More information about the diagnostic method
Treadmill test
A treadmill test is an electrocardiographic study that is performed during physical activity on a special treadmill (treadmill). Such a functional test allows you to identify heart rhythm disturbances, which usually appear only during increased stress and are absent at rest.
More information about the diagnostic method
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Forecast
Cardiac arrhythmias are dangerous because they can lead to sudden cardiac arrest due to complete blockade of conduction. In severe arrhythmia, there is a high risk of ventricular fibrillation, which can be fatal. Atrial fibrillation leads to the formation of blood clots in the atria and their transfer to other organs with the development of stroke and gangrene of the extremities. The probability of an unfavorable outcome in patients with arrhythmias depends on the form of rhythm disturbance and is more than 20% per year. You should not rely on folk remedies - arrhythmia is very dangerous and requires correction by a professional cardiologist.
Bibliography
- Guzovskaya, E.V. Pathophysiology of the heart: textbook/ / E.V. Guzovskaya, S.F. Nepomnyashchy; GBOU VPO IGMU of the Ministry of Health of Russia - Irkutsk, IGMU - 48 p.
- Zatonskaya, E.V. Epidemiology of arrhythmias (review of literature data)/ E.V. Zatonskaya, G.V. Matyushin, N.G. Gogolashvili, N.N. Novgorodtseva - Text: direct // Siberian Medical Review, 2021.- No. 3.- P.5-16.
- Sozonov, A.V. The role of a single-channel electrocardiogram at home in the diagnosis of heart rhythm disorders in children / A.V. Sozonov, Yu.A. Trunova, O.S. Pokusaeva-text: direct // Russian Journal of Cardiology, 2021.-No. 24 (add.) – P. 18-19.
- Hingorani P., Natekar M., Deshmukh S., Karnad DR, Kothari S., Narula D., Lokhandwala Y. Morphological abnormalities in baseline ECGs in healthy normal volunteers participating in phase I studies // Indian. J. Med. Res. - 2012. - Vol. 135. - P. 322-330.
Author:
Pugonina Tatyana Alekseevna, Therapist
Causes of pathology
- Alcohol abuse, smoking, drug use
- Including plenty of caffeine-containing foods and drinks in your diet
- Side effects of certain medications
- Psycho-emotional stress and hard physical labor
- Somatic diseases (coronary heart disease, consequences of myocardial infarction, arterial hypertension, diseases of the adrenal glands and thyroid gland)
- Traumatic brain injuries
- Menopause
Anticoagulants thin the blood - is it dangerous?
Like any blood thinners, anticoagulants can cause bleeding. However, the risk of bleeding is 10 times lower than the risk of stroke. If a person has spontaneous bruises, nosebleeds, heavy menstruation, or blood in the urine, this is not an indication that the dosage needs to be reduced. Minor bleeding does not cause death, unlike a stroke. If you have the above symptoms of bleeding, you need to come for an examination to your attending physician - a gynecologist, urologist and, of course, a cardiologist.
| If a person takes anticoagulants, he must take a general blood test, creatinine, glomerular filtration rate (creatinine clearance), potassium, sodium, ALT, AST every 6 months. |
How do I know if I have atrial fibrillation?
The most common symptoms of AF are palpitations, shortness of breath and general weakness. You should not trust subjective sensations - you need to do a cardiogram or conduct daily Holter ECG monitoring.
Holter will help more accurately determine the presence of paroxysms. If the paroxysm lasts 30 seconds or more, you can consult a doctor for anticoagulants. There are 40 thousand heartbeats per day, of which there may be 400 extrasystoles (heartbeats out of rhythm) - this is the norm.
It happens that a person does not feel paroxysms - for example, when they happen at night. This is bad because small blood clots can form that will block small vessels in the brain. Loss of blood supply to some areas will lead to their death, which significantly increases the risk of developing dementia.
In young people, extrasystoles may have extra-cardiac causes - it is necessary to check the levels of ferritin, hemoglobin, thyroid hormones, examine the gastrointestinal tract in order to exclude reflux-esophagitis, which also causes rhythm disturbances, including atrial fibrillation. People with AF need to undergo liver, kidney and general blood tests every 6 months.
| There are three forms of atrial fibrillation: — Permanent form — Persistent form (AF goes away with medical help) — Paroxysmal form (AF appears and goes away on its own) |
Emergency care for patients with an acute attack of atrial fibrillation
If a person knows that he may have an attack of atrial fibrillation, then he should be able to provide first aid to himself. These activities are carried out until the medical team arrives.
They are called vagal tests:
- Sinus massage. The patient lies on his back, finds the carotid artery in the neck and gently massages it clockwise.
- Pressure on the eyeballs.
- Stimulation of the cough reflex.
- Valsalva maneuver: you need to take a deep breath and tense your abdominal muscles.
- Pressure on the root of the tongue to induce vomiting.
Prevention of rhythm disturbances
- Treatment of somatic diseases and regular medical examination for these conditions (coronary heart disease, hypertension)
- Proper balanced nutrition (products rich in vitamins and microelements);
- Light physical activity (morning exercises, walking in the fresh air, swimming), exercise therapy according to a specially designed scheme
- Correct work and rest schedule
- Categorical refusal to smoke, drink alcohol, coffee, strong tea
- Weight control (obesity prevention)
- Psycho-emotional peace
Anticoagulants can only be taken as prescribed by a doctor.
Standard dosage: Xarelto 20 mg / once a day Eliquis 5 mg / 2 times a day Pradaxa 150 mg / 2 times a day
Studies show that patients are more comfortable taking Xarelto - taking it once a day is easier to remember, especially for older people.
"Wafarin": take one tablet in the evening, take the INR test after 3-4 days. If the INR does not reach 2.0, then the doctor should increase the dosage. The INR should be taken every 3-4 days until the desired level is reached. Then you need to take an INR test every 3 weeks.
Important: all medications and their dosage are prescribed strictly during an in-person consultation with a doctor! This information is for informational purposes only and cannot be a guide to action. Self-medication for arrhythmia is unacceptable and can have serious health consequences.
| Reducing the dosage of anticoagulants mainly depends on only three parameters: — Creatinine clearance is less than 50. — The patient’s weight is less than 65 kg. — The patient’s age is over 85 years. In other cases, reducing the dosage risks a stroke. |