The concept of heart disease includes various anomalies, septa, valve apparatus, large vessels of the heart that affect blood circulation.
This diagnosis appeared relatively recently, when it became possible to study the functioning of the heart in real time using ultrasound. Until this moment, doctors could not identify either the pathology or its danger in a person.
Modern ultrasound diagnostic equipment allows you to assess the condition of tissues, determine the speed of blood flow and its direction. In this regard, it became possible to track disorders and the terminology arose: congenital heart disease and acquired heart disease.
Congenital heart defect
Congenital heart disease is determined in utero. This is a change in tissue structure, disruption of connective tissue. The statistics are increasing every year. In many cases, surgery is required to save life. People with congenital heart disease receive a disability group and must be registered with a cardiologist for life. Among such patients there is a high mortality rate in the absence of qualified medical care.
Among the risk factors, the following should be noted: heredity, drug intoxication of the fetus, complications during pregnancy.
Causes of heart disease
- genetic and chromosomal abnormalities;
- infectious diseases of women during pregnancy (rubella and others);
- bad habits of the expectant mother - alcoholism, smoking, drug addiction;
- exposure to radiation;
- medicinal factor.
Malformations of newborns: causes
Unfortunately, the excellent condition of the parents’ body, good heredity and maintaining a healthy lifestyle do not always guarantee the birth of an absolutely healthy child. For almost 60% of cases of birth of children with congenital defects, specialists do not have any objective explanations. The remaining amount is associated with hereditary and external negative factors, or a combination of them.
Genetics plays a huge role in the development of some congenital defects. Every cell in the body is made up of genes, which in turn make up chromosomes. If a violation occurs in the chromosome set: one gene is missing or mutated, malformations of children occur.
Congenital malformations of a newborn are often caused by the state of health of the expectant mother: for example, if during pregnancy she suffered from rubella, the fetus may develop malformations. The development of congenital anomalies can also be caused by: consumption of alcoholic beverages, drugs, smoking, exposure to various types of radiation.
The development of multifactorial defects is caused by a combination of teratogenic and hereditary factors.
Acquired heart defect
During life, acquired heart defects also often develop. Most often in this case, the valve apparatus suffers, the petals of which lose their elasticity. In its mildest form, it is sagging. In the future, the situation is aggravated by loose closure and so-called reverse blood flow. The mortality rate among patients with acquired heart disease is lower, approximately 15-20%, but still high.
There are two main types of acquired heart disease:
- Stenosis, when the working openings for the passage of blood narrow;
- Failure is the failure of the heart chamber to close tightly, resulting in backflow of blood called regurgitation. Regurgitation, in turn, has several degrees from 0 (when there is no reverse blood flow)
Causes of acquired defects:
- Endocarditis (connective tissue diseases) of the heart of various etiologies from infectious to rheumatic;
- Heart injuries;
- Complications after infectious diseases of other systems;
- Sepsis.
Ventricular septal defect
This is a communication between the ventricles (chambers of the heart), in which, unlike the atria, the pressure is high, and in the left ventricle it is 4-5 times higher than in the right. The presence or absence of clinical manifestations depends on the size of the defect and in what area of the interventricular septum it is located. This defect is characterized by a loud heart murmur. Pulmonary hypertension can develop quickly, starting in the second half of life. It should be noted that with the formation of pulmonary hypertension and increased pressure in the right side of the heart, the heart murmur begins to decrease, since the discharge through the defect becomes less. This is often interpreted by the doctor as a reduction in the size of the defect (its healing), and the child continues to be observed at the place of residence without being referred to a specialized institution. As pulmonary hypertension progresses to its irreversible stages, the pressure in the right ventricle becomes greater than in the left, and venous blood from the right parts of the heart (carrying blood to the lungs for oxygenation) begins to flow into the left (from which oxygen-rich blood is sent to all organs and tissues). The patient develops bluish skin (cyanosis), and physical activity decreases. In this condition, the patient can only be helped by a heart and lung transplant, which is not done for children in our country.
Advertising
On the other hand, ventricular septal defects are prone to spontaneous closure, which is associated with the growth characteristics of intracardiac structures in the baby, so they are usually not in a hurry to be eliminated surgically immediately after birth. In the presence of heart failure, the signs of which are determined by the doctor, drug therapy is prescribed to support the functioning of the heart and the dynamics of the development of the process are monitored, examining the baby every 2-3 months and conducting echocardiography. If the size of the defect decreases to 4-5 mm or less, then such defects, as a rule, are not operated on, since they do not affect health and do not cause pulmonary hypertension. If it comes to surgery, then ventricular septal defects are closed in the vast majority of cases using artificial circulation, cardiac arrest using a patch. However, over the age of 4-5 years, with a small size of the defect and its specific localization, endovascular closure is possible using an occluder passed through the vessels. It should be noted that it is better to be observed in a cardiovascular surgery center (the doctors there, including echocardiographers, which is very important, have more experience). If the size of the defect decreases to 4-5 mm or less, then such defects, as a rule, are not operated on, since they do not affect health and do not cause pulmonary hypertension.
Signs of heart disease
If a person has a heart defect, the symptoms are similar to those of heart failure.
- Increased fatigue, even with the slightest exertion, dizziness and fainting, drowsiness;
- Difficulty breathing, especially when lying horizontally, as at this time the pressure in the vessels of the lungs increases. Against this background, coughing attacks and frequent infectious diseases of the lower respiratory tract may occur.
- Pain with heart disease can also occur due to an enlarged liver in the right hypochondrium, or in the area of the heart.
- Cardiopalmus;
- Blue discoloration in the nasolabial area during exercise or walking.
2. Symptoms of the disease
Sometimes it happens that the symptoms of heart disease do not appear at all and the disease does not cause any concern. Or, for example, symptoms of the disease appear only in adulthood. As a rule, symptoms of heart disease in adults are expressed in the following forms:
- Dyspnea;
- Labored breathing;
- Rapid fatigue, fatigue;
- Inability to perform activities associated with heavy physical exertion;
- Headache;
- Dizziness;
- Pain in the heart, abdominal area.
Visit our Cardiology page
Treatment
When a heart defect is diagnosed, treatment consists of either maintaining a stable condition without worsening, or radical surgical intervention. It will not be possible to cure heart disease with medication, so the only thing you can do is monitor your health, carefully, by visiting a cardiologist.
The Heratsi Medical Center employs experienced cardiologists and ultrasound specialists with an academic degree who will help to clearly and correctly carry out diagnostic measures and develop a program for supporting a patient with heart disease.
The cost of services can be viewed in the “Price” section or by calling the 24-hour hotline.
Risk group
Conducting a medical-genetic consultation, which allows for the timely identification of malformations of a newborn, is recommended for future parents in the following cases:
- if there are cases of birth of children with congenital pathologies in the families of one or both parents, even if the parents themselves do not have health problems;
- if the family already has a case of the birth of a child with developmental defects;
- if a woman has a history of spontaneous abortion or stillbirth;
- if the spouses are related;
- if the age of the future mother exceeds 35 years, and the future father – 50 years;
- if the activities of one or both parents are associated with the influence of negative external factors, as well as their abuse of alcohol or drugs.
If a specialist identifies a threat of giving birth to a child with a congenital pathology, the doctor may advise termination of pregnancy (if pregnancy has already occurred), or the use of donor biomaterial for artificial insemination for a couple who is just planning a pregnancy.
Types of ultrasound examinations
Ultrasound diagnostics represents a wide range of studies. There are several types of ultrasound that accurately determine intrauterine malformations of the baby.
Standard ultrasound
. It is usually combined with a biochemical blood test. It is carried out no earlier than 10 weeks of pregnancy. First of all, the thickness of the fetal collar zone is detected, which should not exceed 3 mm, as well as visualization of the nasal bone. In a baby with Down syndrome, the nuchal region is thicker than normal, and the nasal bones are not developed. The following factors also influence the increase in thickness:
- heart disease
- stagnation of blood in the neck veins
- lymphatic drainage disorder
- anemia
- intrauterine infections
Doppler - uh
This is an unusual ultrasound test that evaluates fetal blood flow. The difference between the sent and reflected signal indicates the norm or pathology of the fetus-placenta-mother chain.
- 3D ultrasound allows you to see a color image of the baby, see the limbs, the absence of fused fingers, underdeveloped feet, etc. The accuracy of diagnosing the nuchal translucency increases by 30%. The doctor can tell for sure whether there are pathologies in the development of the neural tube.
- 4D ultrasound does not differ in operating principle from simpler options, but has many advantages. The doctor sees a three-dimensional image of the heart and a view of the fetus from different angles. It is 4D diagnostics that finally dots all the i’s, whether there are chromosomal abnormalities or not. It can be stated with 100% accuracy whether there are malformations of the nervous system, skeletal dysplasia, cleft lip or cleft palate.
Lower limb defects
Developmental anomalies of the lower extremities are similar to the upper ones. Congenital anomaly of the lower extremities in ICD-10 occupies codes Q74.1-Q74.9.
Main diseases:
- abnormalities of the foot - its partial or complete absence;
- underdevelopment of the hip;
- hip dysplasia;
- valgus and varus curvature;
- absence of the patella;
- dislocations;
- false joint.
Autosomal recessive mode of inheritance
The carrier of the pathological trait is a recessive gene contained in the autosome. With an autosomal recessive inheritance mechanism, the situation looks paradoxical - healthy parents suddenly give birth to a child with developmental defects, sometimes severe and even incompatible with life. The reason is the latent carriage of mutant recessive genes by both spouses. However, the birth of a sick child does not necessarily mean that all subsequent children will suffer from the same disease. Just as in the autosomal dominant type, boys and girls are equally susceptible to the disease.
When and why genetic pathologies of the fetus occur: risks by age
Anomalies in fetal development occur already at the moment of fertilization of an egg by a sperm. For example, a pathology such as triploidy (the presence of three chromosomes in a row of a chain, and not two, as expected), occurs when two sperm penetrate the egg, each of which leaves one chromosome. Naturally, with such a set, a living organism cannot survive, so at a certain stage a miscarriage or frozen pregnancy occurs.
Spontaneous miscarriages occur in 50% of abnormal fertilizations. This is how nature protects humanity from complete degeneration.
In general, chromosomal pathologies are divided into 4 groups:
- Gametopathy.
The pathology is present even before conception in the sperm or egg itself, i.e. This is a genetic disease - a congenital pathology. - Blastopathy
. Anomalies occur in the first week of zygote development. - Embryopathy
. The embryo receives damage from 14 to 75 days after conception. - Fetopathy
. It consists in the formation of pathology of fetal development starting from the 75th day after fertilization.
No one is immune from the birth of a baby with genetic disorders. If previously the risk group included mothers over 35 years of age, diabetics, women with chronic diseases (kidney failure, thyroid problems), today sick children are born to young mothers aged 20 to 30 years.
These statistics lead to gloomy thoughts. Thus, the risk of having a baby with chromosomal abnormalities in 20-year-old women is 1:1667, and in 35-year-old women it is already 1:192. But in reality, this means that in 99.5% of cases, a child of a thirty-five-year-old mother will be born healthy.
Clinical picture of congenital malformations of children
Symptoms of fetal malformations are varied and depend on which organ and system is involved in this pathological process. Most often, pathologies appear immediately after the baby is born. For example, if the child’s respiratory system is defective, respiratory failure is diagnosed; abnormalities in the development of the heart muscle are manifested by heart rhythm disturbances.
The presence of a number of chromosomal diseases can be suspected by characteristic external signs: with Down syndrome, children are born with flat faces, slanted eyes and a characteristic skin fold on the neck. Cretinism is manifested by dwarfism, hydrocephalus - by an increased head size and displacement of the eyeballs.
What genetic diseases of the fetus can be seen on ultrasound, when to undergo it
It cannot be said that an ultrasound shows 100% of all abnormalities, but with a high degree of probability a woman will know about the health status of her unborn baby. During the entire pregnancy, a woman undergoes at least three ultrasound examinations: in the 1st, 2nd and 3rd semesters. They are called screening ultrasounds.
In the 1st semester, from 10 to 14 weeks (until the 10th week, ultrasound is not informative), the pregnant woman undergoes a study called screening. It consists of a biochemical blood test and ultrasound examination of the embryo. The result of screening is the identification of the following pathologies:
- Down syndrome
- Patau syndrome
- Edwards syndrome
- Shereshevsky-Turner syndrome
- Carnelia de Lange syndrome
- Smith-Lemli-Opitz syndrome
- Prader-Willi syndrome
- Angelman's syndrome
- Langer-Gideon syndrome
- Miller-Dicker syndrome
- DiGeorge anomaly
- Williams syndrome
- Wilms tumor
- triploidy (when there are not 46 chromosomes in each pair, but 69, i.e. three, not two)
- neural tube defect
At 20-24 weeks another ultrasound is done. Among the genetic diseases of the fetus visible on ultrasound examination in the 2nd semester, the following can be noted:
- anencephaly (absence of the brain, diagnostic accuracy 100%)
- pathology of the abdominal wall (86%)
- pathology of limb development (90%)
- spinal cord herniation (87%)
- developmental pathology or absence of kidneys (85%)
- the presence of a hole in the diaphragm, which separates the abdominal cavity and chest (85%)
- hydrocephalus or dropsy of the brain (100%)
- heart abnormalities (48%)
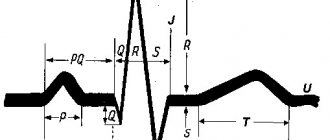
In the 3rd semester, Doppler ultrasound is performed - an ultrasound examination to determine the vascular system of the fetus, placenta and mother. Starting at 23 weeks of pregnancy, the umbilical artery, uterine artery and middle cerebral artery are checked. Systolic (when the heart muscle contracts) and diastolic (when the heart muscle relaxes) blood flow is examined. A baby with chromosomal disorders has atypical blood flow.
Also in the 3rd semester, fetal fetometry is required - measurement of size in order to identify developmental anomalies.
What does an ultrasound of general fetal pathologies look like: photos and interpretation of ultrasound results
Genetic pathologies can be both specific (Down syndrome, Wilms tumor) and general, when the internal organ develops incorrectly. To identify common abnormalities, anatomical examination of the fetus is available. It is carried out in the 2nd semester starting from the 20th week of pregnancy. During this period, you can see the baby’s face and determine its gender.
With an anatomical ultrasound, all organs of the fetus are displayed on the screen in a section, and in the image the bones will appear white, and the soft tissues will appear in various shades of gray. The specialist can clearly see the structure of the brain; he is also able to see abnormalities in development. A cleft in the upper palate, called a cleft lip, becomes noticeable.
Longitudinal and transverse projections of the spine confirm or refute the correct location of the bones; one can verify the integrity of the abdominal wall. The absence of heart pathologies is confirmed by the identical sizes of the atria and ventricles. The normal functioning of the stomach is indicated by its fullness with amniotic fluid. The kidneys should be in their place, and urine from them should flow freely into the bladder. The doctor clearly sees the fetal limbs, except for the toes.
How to prevent fetal defects and where to get a fetal ultrasound in St. Petersburg
You can prevent most problems with pregnancy and fetal pathologies by planning your pregnancy in advance. When undergoing examination during planning, both partners undergo tests that clearly show the likelihood of genetic abnormalities. A range of tests are also carried out for infections that can cause deformities in the baby (TORCH complex) and other studies.
We invite you to undergo an ultrasound scan for fetal pathology in St. Petersburg at the Diana Clinic. We have installed the latest ultrasound machine with Doppler. The examination is carried out in 3-D and 4-D formats. A disc with the recording is given to you.
Genetic pathologies of the fetus: what they look like on ultrasound and prognosis of the pathology
| Pathology | How and when is it detected? | What is the essence of pathology | Character traits | Mental and intellectual development |
Down syndrome | A chorionic villus biopsy is performed, enlarged nuchal translucency in the fetus, underdevelopment of the nasal bones, enlarged bladder, fetal tachycardia | Chromosomes of the 21st pair, instead of the required 2, are represented by 3 in the chain | Slanting Mongoloid eye shape, regardless of the child’s race, undeveloped bridge of the nose, shallow-set eyes, semicircular flat ear, shortened skull, flat back of the head, shortened nose | Delayed intellectual development, small vocabulary, lack of abstract thinking, lack of concentration, hyperactivity |
| FORECAST | They live up to 60 years of age; in rare cases, subject to constant activities with the child, his socialization is possible. This child needs constant supervision | |||
Patau syndrome | Small head at 12 weeks on ultrasound, asymmetrical hemispheres, extra fingers | Trisomy is present on chromosome 13 | Children are born with microcephaly (underdevelopment of the brain), low forehead, slanted palpebral fissures, cleft lip and palate, corneal clouding, heart defects, enlarged kidneys, abnormal genitals | Profound mental retardation, lack of thinking and speech |
| FORECAST | 95% of children with Patau syndrome die before the age of one year, the rest rarely live to 3-5 years | |||
Edwards syndrome | Chorionic villus biopsy, intrauterine blood sampling from the umbilical cord, microcephaly is visible on ultrasound | There is trisomy on chromosome 18 | Mostly girls (3/4) are born, and the male fetus dies in the womb. Low sloping forehead, small mouth, underdeveloped eyeball, cleft upper lip and palate, narrow ear canal, congenital dislocations, clubfoot, severe abnormalities of the heart and gastrointestinal tract, underdeveloped brain | Children suffer from oligophrenia (organic brain damage), mental retardation, imbecility (moderate mental retardation), idiocy (lack of speech and mental activity) |
| FORECAST | During the first year of life, 90% of sick children die, less than 1% die before the age of 10 years. | |||
Shereshevsky-Turner syndrome | X-ray of fetal bone structures, MRI of the myocardium | An abnormality occurring on the X chromosome | It occurs more often in girls. Shortened neck with folds, swollen hands and feet, hearing loss. Drooping lower lip, low hairline, underdeveloped lower jaw. Height in adulthood does not exceed 145 cm. Joint dysplasia. Abnormal development of teeth. Sexual infantilism (no follicles in the ovaries), underdevelopment of the mammary glands | Speech and attention suffer. Intellectual abilities are not impaired |
| FORECAST | Treatment is carried out with anabolic steroids; girls from 14 years of age are prescribed female hormonal drugs. In some cases, it is possible to overcome the disease, and the woman can become pregnant using IVF. Most patients remain infertile | |||
Polysomy on the X chromosome | Screening at 12 weeks of pregnancy, chorionic villus biopsy, amniotic fluid analysis. The enlargement of the collar area is alarming | Instead of two X chromosomes, there are three or more | It occurs in girls and rarely in boys. Characterized by sexual infantilism (secondary sexual characteristics do not develop), high growth, curvature of the spine, skin hyperpigmentation | Antisocial behavior, aggression, mental retardation in men. |
| FORECAST | With regular classes with teachers and involvement in work activities, the child’s socialization is possible | |||
Polysomy on the Y chromosome | Instead of XY chromosomes there is an extra Y chromosome | Occurs in boys. They grow tall from 186 cm, heavy massive lower jaw, convex brow ridges, narrow shoulders, wide pelvis, stoop, belly fat | Mental retardation, aggression, emotional instability | |
| FORECAST | You need to work with the child, direct him to peaceful activities, involve him in sports | |||
Carnelia de Lange syndrome | When analyzing the blood of a pregnant woman, plasma protein-A (PAPP-A), which is usually high, was not detected in the serum | mutations in the NIPBL or SMC1A gene | Thin fused eyebrows, shortened skull, high palate, abnormally erupted teeth, underdeveloped limbs, marbled skin, congenital malformations of internal organs, growth retardation | Profound mental retardation, |
| FORECAST | Average life expectancy 12-13 years | |||
Smith-Lemli-Opitz syndrome | Ultrasound shows abnormalities of the skull in the fetus, the rib bones are not visible | mutation in the DHCR7 gene, responsible for the production of cholesterol | Narrow forehead, drooping eyelids, squint, skull deformation, short nose, low-set ears, underdeveloped jaws, genital abnormalities, fusion of fingers | Increased excitability, aggression, decreased muscle tone, sleep disturbances, mental retardation, autism |
| FORECAST | Therapy using dietary cholesterol | |||
Prader-Willi syndrome | There is low fetal mobility, abnormal position, | Chromosome 15 is missing the paternal part of the chromosome | Obesity with short stature, poor coordination, weak muscle tone, squint, thick saliva, bad teeth, infertility | Mental retardation, speech delay, lack of communication skills, poor fine motor skills. Half of the patients have an average level of intelligence and can read |
| FORECAST | With constant practice, a child can learn to read, count, and remember people. Overeating should be fought | |||
Angelman syndrome | Starting from the 12th week, there is a delay in fetal development in height and weight | The UBE3A gene is absent or mutated on chromosome 15 | Frequent unreasonable laughter, small tremors, many unnecessary movements, wide mouth, tongue hanging out, walking with absolutely straight legs | “Happy puppet syndrome”: the child laughs often and for no reason. Mental retardation, hyperactivity, impaired motor coordination, chaotic hand waving |
| FORECAST | Antiepileptic therapy is carried out, muscle hypotonicity is reduced by massage, in the best case, the child will learn non-verbal communication and self-care skills | |||
Langer-Gideon syndrome | Maxillofacial anomaly is visible on 4D ultrasound | trichorinophalangeal syndrome, which consists of a violation of the 8th chromosome | Long pear-shaped nose, underdeveloped lower jaw, very protruding ears, uneven limbs, curvature of the spine | Mental retardation, varying degrees of mental retardation, lack of speech |
| FORECAST | Poorly amenable to correction, low life expectancy | |||
Miller-Dicker syndrome | Ultrasound shows an abnormal structure of the skull, facial disproportions | Pathology in the 17th chromosome, causing smoothing of the cerebral convolutions. Caused by fetal intoxication with aldehydes due to maternal alcohol abuse | Dysmorphia (alcohol syndrome), heart defects, kidney defects, seizures | Lissencephaly (smooth gyri of the cerebral hemispheres), underdevelopment of the brain, mental retardation |
| FORECAST | Survival up to 2 years. Children can only learn to smile and make eye contact. | |||
DiGeorge Anomaly | In some cases, ultrasound reveals various defects of the baby’s organs, especially the heart (tetralogy of Fallot) | Disease of the immune system, a violation of a region of the 22nd chromosome | Hypoplasia of the thymus (underdevelopment of the organ responsible for the production of immune cells), deformation of the face and skull, heart disease. There are no parathyroid glands responsible for the metabolism of calcium and phosphorus | Atrophy of the cerebral cortex and cerebellum, mental retardation, difficulties with motor skills and speech |
| FORECAST | Treatment with immunostimulants, thymus transplantation, calcium-replenishing therapy. Children rarely live past the age of 10 and die from the consequences of immunodeficiency | |||
Williams syndrome | Ultrasound shows imbalances in skeletal development and joint elasticity | Genetic disease caused by a missing link on chromosome 7 | The synthesis of elastin protein is impaired; children have a typical “Elf face”: swollen eyelids, low-set eyes, sharp chin, short nose, wide forehead | Increased sensitivity to sound, impulsivity, obsessive sociability, emotional instability, anxiety, expressive speech |
| FORECAST | Speech is well developed, even better than that of healthy peers. Pronounced musical abilities (absolute pitch, musical memory). Difficulty solving math problems | |||
Beckwith-Wiedemann syndrome | Ultrasound reveals abnormally disproportionate limbs, excess body weight, and kidney pathology | Genetic disease caused by a missing link on chromosome 11 | Rapid growth at an early age, abnormally large internal organs, a tendency to cancer. The child has an umbilical hernia, an abnormally large tongue, and microcephaly (underdevelopment of the brain). | Emotional and mental development in some cases does not lag behind the norm. Severe mental retardation sometimes occurs |
| FORECAST | Life expectancy is the same as that of ordinary people, but there is a tendency to cancerous tumors | |||
Treacher Collins syndrome | Ultrasound shows pronounced asymmetry of facial features | Genetic mutation on chromosome 5 that causes abnormal bone structures | The child has practically no face, a pronounced physical deformity | Absolutely normal psycho-emotional development |
FORECAST | Surgical interventions are performed to eliminate deformities | |||