Doctors Cost
Price list Doctors clinic
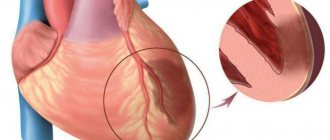
Varicose eczema is a disease that occurs as a complication of varicose veins caused by stagnation of blood in altered veins. As a result of circulatory disorders, atrophic processes occur in the skin adjacent to the causative area. This may be the result of thrombophlebitis, for which inadequate and untimely treatment was prescribed. But the most common reason is the lack of treatment for varicose veins.
According to statistics, the disease is more often observed in older people, more often in women.
What is varicose eczema
Eczema is an inflammatory process on the skin that occurs in a chronic form and is a consequence of venous stagnation. Pathology in medicine also goes by other names - venous eczema, hyperemic eczema or stasis dermatitis. Features of the disease - the lesion concerns the skin of the lower extremities, develops gradually, and if left untreated, progresses to trophic ulcers.
Trophic eczema. Reviews from patients of Dr. Semenov A.Yu.
I have been suffering from varicose veins for 10 years, although I HAVE NOT SUFFERED BEFORE!
I decided to contact the laser surgery center after reading the reviews. Already when trophic eczema appeared on the skin, it was necessary, of course, earlier, but it’s good that not later. I went to the clinic on June 29, 2011, I think that I was lucky to get an initial appointment with Artem Yuryevich Semenov. Sensitive, good-natured and, as time has shown, a professional in his field, made a diagnosis, suggested a course of treatment (radiofrequency ablation +...More details Emil Rustamovich Akhmedzhanov, Moscow, 02/10/2013.
Varicose veins were inherited from me. At the age of 30 I treated myself with sclerotherapy. The veins and bumps were gone and my left leg looked great. After the birth of my second child, the problems with my left leg returned. At first, small bumps appeared, and over time, darkening appeared on the left leg. Then a whole spot grew from a small spot, which turned out to be trophic eczema (((. My leg began to ache from a long walk. I had to constantly use Lyoton. Of course, time was lost, I...More
Tatyana Chertilina, Moscow, 03/01/2017
Reasons for the development of pathology
The only reason for the onset of the disease is venous stagnation, which occurs against the background of impaired blood flow in the veins. The result will be incomplete blood supply to the small vessels of the dermis, which provokes eczematous changes - the skin becomes as traumatic as possible, and with the existing oxygen starvation, the wounds simply do not heal. Such damage is a “gateway” for infectious agents.
Venous congestion in the lower extremities does not develop on its own; provoking factors are always present:
- phlebeurysm;
- leg injuries;
- chronic heart and vascular diseases;
- presence of excess weight, obesity 2-3 degrees;
- elderly age;
- period of bearing a child.
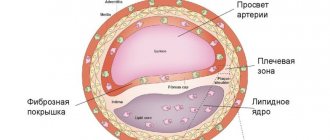
Against the background of these conditions, the veins of the lower extremities dilate and the valves (components of the vessels) begin to function incorrectly: blood flow when moving from bottom to top becomes difficult, pressure increases. Blood cannot flow through the veins at normal speed - stagnation is almost guaranteed.
The likelihood of developing varicose eczema increases significantly if a person has previously been diagnosed with:
- thrombosis, thrombophlebitis;
- renal failure;
- persistently elevated blood pressure.
Lifestyle and the specifics of work activity play an important role: physical inactivity, excessive physical activity (heavy lifting), staying in one position for a long time (sitting, standing).
How does varicose eczema manifest on the lower extremities?
Even at the very beginning of the development of blood flow disorders in the lower extremities, changes occur in the cells of the skin. At first they are invisible, but as the underlying disease progresses, the symptoms of dermatological pathology will become more pronounced:
- even with short-term immobility, the legs become numb and “heavy”;
- the skin over the changed vessels becomes very dry and begins to itch;
- by the end of the day there is always extensive swelling of the lower extremities;
- the skin takes on a red tint and microcracks appear on it.
The first signs of varicose eczema on the legs appear in the ankle area, then they spread in an ascending line. Damage to the dermis becomes deep, infectious agents penetrate into them - healing becomes prolonged, and scars remain after it.
If treatment is not carried out at this stage of the disease, then the symptoms become more pronounced and new ones are added:
- the skin in the affected area hardens and feels like a wooden surface;
- the dermis acquires a dark shade - from gray to brown-black;
- the patient complains of severe, unbearable itching in the affected areas;
- the inflamed area of the lower limb decreases in volume due to the “shrinking” of the epidermis.
The skin becomes very sensitive, any touch to it causes severe pain, the addition of a bacterial infection provokes the development of a purulent process in the deep layers of subcutaneous fat, and the resulting wounds bleed.
Using a laser
Laser radiation has proven to be very effective in eliminating the root cause of varicose eczema. In this case, the laser’s task is to restore blood flow. The procedure is very effective, painless and completely safe, but only when it is used by an experienced doctor.
The essence of the procedure is that a special catheter is inserted into the lumen of the vein through a small puncture, at the end of which a light guide is placed. By pulling the light guide along the catheter, the lumen of the vein is treated with laser radiation. The procedure is performed very carefully, at intervals; one advance of the light guide takes no more than five centimeters of the damaged vein.
This technique is good, among other things, because it does not leave scars or scars, since it does not involve stitches. Upon completion of the procedure, the puncture site is covered with a sterile bandage. After some time, the previously affected vein begins to become overgrown with connective tissue, and subsequently resolves. During the recovery process, it is important to properly monitor the condition of the skin, use restorative creams, wear compression garments, and avoid contact with direct sunlight.
Diagnosis of complications
Before prescribing treatment for varicose eczema, you need to identify the true causes of its appearance. This can only be done through clear diagnostic measures:
- laboratory blood test;
- ultrasound diagnostics of veins of the lower extremities;
- examination of the entire cardiovascular system.
The doctor will definitely study the patient’s medical history, so at the appointment you need to talk about whether leg injuries, thrombosis, heart disease were previously diagnosed and whether surgical interventions were performed in the affected area.
The choice of treatment tactics depends on the identified causes of the disease. It will be possible to eliminate the symptoms only after stopping the main pathological process. Otherwise, the pathology will progress, at times entering the stage of remission.
Treatment of venous trophic ulcers in the leading European phlebology center in Moscow
Even modern innovative treatment of trophic ulcers can be quite complex. Therefore, it is better when an experienced phlebologist deals with it in Moscow. The leading points in treatment will be:
- Local treatment of ulcers.
- Elimination of pathological venous discharge.
The stages of solving each of these issues will be determined by the condition of the wound, the extent of damage to the venous system, and the general condition of the patient’s body. For local treatment of ulcers, modern innovative wound coverings are used, which reduce the number of dressings. The use of a compression bandage or modern compression products, which is better in this situation, will be determined by the doctor at an appointment at the best phlebological center in Moscow. Elimination of the leading cause of ulcers, pathological venous reflux, requires a thorough analysis of the situation. Conventional surgery to remove varicose veins often involves damage to the lymphatic vessels and can worsen the wound. Modern innovative laser surgery is much less traumatic and allows you to completely remove varicose veins, which were the cause of the trophic ulcer.
All of the listed solutions in the treatment of venous trophic wounds are the most modern and comply with state European standards. This approach is certainly good, but the best solution would be to treat varicose veins before the appearance of trophic disorders.
Stages of pathology development
Doctors distinguish 4 stages of development of venous eczema, each with characteristic signs:
- Stage 1. The safest for health, accompanied by the periodic appearance of red spots on the skin of the legs, does not bother the patient. At this stage, you can use conservative therapy and implement doctors’ recommendations regarding nutrition and physical activity.
- Stage 2. The classic symptoms of the pathology become intense, experts recommend that patients stay in a medical facility and receive therapy under the supervision of medical professionals.
- Stage 3. Bubbles with cloudy liquid form on the affected areas of the skin. At the slightest touch they burst, liquid flows out of them and this is accompanied by an unpleasant odor. The risk of infection becomes extremely high.
- Stage 4. All existing blisters burst, the surface becomes covered with a dense crust that itches unbearably. For some time, eczema disappears - a short period of remission occurs.
Treatment methods for varicose eczema
Therapy for the disease should be comprehensive: medications, ointments, nutrition, regular care of the damaged area. Wearing elastic bandages becomes mandatory. Some patients prefer compression garments - they are no less effective, but not practical: varicose eczema is accompanied by wounds and the leakage of serous fluid and pus from them. In such conditions, changing and washing bandages is much easier.
Most patients think that water procedures are prohibited during the inflammatory process - this is not true. Hygiene of the injured limb requires constant adherence to basic recommendations. You should wash your feet every day with soap and running water.
In addition to drug therapy, the patient must follow the following recommendations from doctors:
- Give moderate stress to the lower extremities - walking in the fresh air, exercising on an exercise bike at home, Nordic walking. It is important to discuss the frequency, duration and level of load in advance.
- Start the fight against excess weight, if any. To do this, it is worth following a protein-plant diet, and, if possible, completely eliminating carbohydrates from the diet. The basis of nutrition can be salads from fresh vegetables and fruits, seafood and fish, meat, lard, and a small amount of cereals. Sweets, bread, milk and dairy products, and citrus fruits should be completely excluded.
- Wear loose clothing and shoes that fit properly. Give preference to natural fabrics, because synthetics can be irritating to overly sensitive skin.
Drug treatment
Systemic medications are prescribed - from the group of phlebotonics Detralex, Ascorutin, Phlebodia, which eliminate swelling, improve blood flow in damaged veins, and increase the tone of the vascular walls.
As part of the treatment, anti-inflammatory drugs are also taken - Diclofenac, Dexalgin, Nimesil. They not only stop the pathological process, but also “work” as a pain reliever.
The prescription of antibacterial drugs is carried out on an individual basis and only in case of infection. Previously, the laboratory obtains the results of a study of cultures from the wound to determine a suitable remedy.
What ointments are prescribed for eczema
Damaged skin areas should be treated with antiseptic agents daily. The most appropriate solutions would be Miramistin, Prontosan or Octeniderm - they are highly effective and hypoallergenic.
1-2 times a day, ointments from the group of hormonal drugs - Hydrocortisone, Prednisolone, Lorinden S, Fluorocort - are applied to the affected areas of the legs. A specific drug will be prescribed by the attending physician; any of them is used for a limited amount of time - you must strictly follow the instructions.
Modern approach to the treatment of skin pathologies associated with venous insufficiency
Introduction
Chronic venous insufficiency (CVI) is one of the most common vascular diseases, observed, according to epidemiological studies, in 60–77% of the adult population [1].
Based on a series of large studies, risk factors for the formation of CVI have been identified as gender, obesity, prolonged bed rest, previous deep vein thrombosis, operations on the abdominal organs, pelvic organs and near the passage of large venous lines, pregnancy, and the patient’s age [2]. An integral part of CVI and, often, the first complaint with this disease are skin manifestations, which form the basis of the modern classification of this pathology - CEAP. According to CEAP, hyperpigmentation, venous eczema, lipodermatosclerosis, white skin atrophy, open and healed venous ulcers are identified as trophic disorders [3]. The appearance of these symptoms, along with the pronounced polymorphism of the clinical picture of the disease and in the absence of visible varicose changes in the saphenous veins, forces the patient to consult a dermatologist for the first time. Complaints
The main complaints of the patient with trophic disorders of venous etiology: swelling of the lower extremities, soreness of the skin of the legs, the presence of petechial elements and a change in skin color to reddish-brown, which occurs as a result of the breakdown of hemoglobin in the petechial elements and the conversion of the remaining iron into hemosiderin. In addition, patients quite often complain about the presence of blisters, weeping, erosive and ulcerative skin defects, and erythema - a sign of chronic dermatitis.
Inspection
Upon examination, a specialist dermatologist identifies in such patients a certain complex of pathological skin processes typical of CVI. These include such manifestations of static dermatitis (caused by direct disruption of microcirculation in the vascular bed of the skin), such as edema, hyperemia, lack of hair, lipodermatosclerosis and ulceration [4]. Hemosiderosis of the skin, manifestations of hyperkeratosis in the form of peeling, nummular eczema, contact dermatitis (due to the use of various non-physiological dressings, patches and irritating drugs), erosive and ulcerative skin defects, dystrophic changes in the nail plates and onychomycosis, panniculitis are often observed [5].
Lead tactics
When determining the management tactics for such patients, it is necessary to take into account that a patient with skin pathology due to CVI needs a comprehensive, comprehensive examination of the condition of the skin, identification of vascular bed pathology and concomitant diseases, and assessment of endocrinological status. Thus, the presence of undiagnosed decompensated hyperglycemia will negate the effect of using the most modern topical agents, not counting the time and money spent on inadequate therapy. However, even within one class of clinical manifestations, the severity of this disease is determined by the presence of infection of the zone of trophic disorders, in particular microbial eczema, accompanied by secondary infection of skin defects. Bacterial contamination significantly changes the symptoms of the disease, aggravates its course, complicates the choice of patient management tactics and causes relapses and the addition of other diseases, including lymphostasis and erysipelas [5].
Diagnostic measures
In accordance with the standards, in addition to identifying complaints, collecting anamnesis and clinical examination, the patient is shown an ultrasound examination of the veins in the volume of duplex or triplex angioscanning of deep, superficial, saphenous and perforating veins with determination of the anatomical features of the structure and course of the vessels, the patency of their lumen and the characteristics of blood flow. Next, a consultation with a surgeon is indicated, who, if indicated, determines the tactics of further examination, conservative and surgical treatment [6]. We emphasize that in the presence of severe chronic pathology of the deep main veins, only joint, coordinated actions of the surgeon and dermatologist can ensure successful treatment of the patient and prevention of possible complications and chronicity of the process with a sharp decrease in the patient’s quality of life.
Treatment
General measures Regardless of the nature of the patient’s complaints, any specialist must motivate the patient to a certain lifestyle that corresponds to his condition. Thus, it is necessary to minimize periods of physical inactivity, static loads, heavy lifting, eliminate exposure to high temperatures, normalize body weight, follow a diet that promotes weight normalization and adequate intestinal motility, wear comfortable clothes, shoes and maintain a physical activity regimen. In most cases, the factor predisposing to the development of an erosive or ulcerative skin defect with CVI is trauma, often very minor. In this regard, we consider it very important to wear compression hosiery not only as a means of relieving the phenomena of phlebohypertension, but also as protection that protects compromised skin from unwanted mechanical effects. Unfortunately, patients perceive recommendations for wearing compression hosiery as something auxiliary and of little importance for treatment; they often complain that it is “difficult to put on” or “it is very hot.” Therefore, the task of both the surgeon and the dermatologist is to select a high-quality compression product with strict adherence to the dimensions and indications for use of a particular compression class and knitwear model, as well as a detailed explanation of the risks that arise when refusing to wear compression stockings.
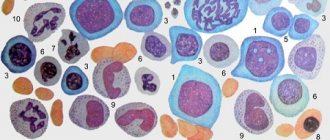
Drug therapy An integrated approach to the treatment of CVI associated with skin pathology can and should include multidirectional drugs, the prescription of which is determined individually, based on the clinical manifestations of a particular patient. These include: • drugs that improve microcirculation and phlebotropic drugs; • compression therapy; • topical preparations containing heparin and dimethyl sulfoxide; • local antibiotics in various forms; • solutions of aniline dyes; • keratoplasty ointments; • topical glucocorticosteroids and their combinations with other drugs; • moisturizers; • drugs that create a protective film, or physiological dressings, selected depending on the phase of the wound process; • systemic antibiotics; • systemic glucocorticosteroids; • multivitamin preparations. An important factor influencing the healing of erosive and ulcerative defects formed during CVI is the open method of managing the wound surface, usually used by dermatologists. At the same time, the wound surface remains free from dressing material, which allows not to disturb the formed epithelium in the marginal zone of the lesion during dressing. A negative attitude towards the traditional gauze bandage is also associated with fairly frequent cases of an inflammatory reaction in the skin surrounding the lesion, as a manifestation of contact dermatitis. The inflammatory reaction is caused by the drugs used and the mechanical effect of the bandage itself (gauze or adhesive). Accordingly, inflammatory changes in the area of skin surrounding the wound prevent epithelization of the lesion. In the case when the surface of the lesion really needs to be closed, it is preferable to use dressings that have an adsorbing, absorbent effect, and select them depending on the phase of the wound process [7]. When choosing treatment tactics, it is necessary to take into account that in conditions of impaired hemodynamics and a decrease in the protective properties of the skin (decreased turgor, dryness, impaired keratogenesis, imbalance of microflora), when the integrity of the skin is violated, favorable conditions are created for secondary infection of the skin [8]. A favorable factor for the occurrence of a secondary infection is the appearance on the surface of the skin of cavity elements that form during eczematization, contact dermatitis, combined arterial-venous insufficiency, and the appearance of “diabetic blisters.” The most common variants of the course of bacterial infection are lesions of the skin itself and subcutaneous fat [9]. Among the causative agents of this process, the most common are various types of staphylococcus and beta-hemolytic streptococcus of group A, and among anaerobic microorganisms, representatives of the genera Clostridium, Bacteroides and Peptostreptococcus are most often identified, and the latter are usually present in association with aerobic microorganisms [10]. The traditional choice of the surgeon in this case is cephalosporin antibiotics, but practice shows that recently there has been a tendency to reduce the sensitivity of the bacterial flora to cephalosporins and a positive effect is achieved by increasing the dosage of the drug, which can lead to adverse consequences. In dermatological practice, preference in the treatment of bacterial skin infections is currently given to tetracycline drugs and macrolides, which have a wide spectrum of action and are less commonly used in routine surgical practice, while minimizing the risk of developing microbial resistance. Undesirable effects from tetracyclines include increased photosensitivity (which precludes the use of these drugs in the summer), discomfort from the gastrointestinal tract, and a teratogenic effect. One of the main undesirable effects of using macrolides is an increase in gastrointestinal motility. However, when treated with semisynthetic macrolides, compared with erythromycin and oral beta-lactam antibiotics, the frequency of adverse reactions is much less pronounced [11]. The antimicrobial effect of macrolides is due to a disruption of protein synthesis on the ribosomes of the microbial cell. When the antibiotic is removed from the body, bacterial growth does not resume, i.e., a post-antibiotic effect occurs. The same feature of action is characteristic of fluoroquinolones, aminoglycosides and tetracyclines. At the same time, antibiotics of this group have immunomodulatory activity and the ability to activate the activity of phagocytic cells [12]. Another important feature of the above group of drugs is their long circulation time in the blood. Roxithromycin has one of the broadest spectrums of action: Streptococcus spp. are sensitive to it. groups A and B, including Str. pyogenes, Str. agalactiae, Str. mitis, Str. saunguis, Str. viridans, Str. pneumoniae, as well as Neisseria meningitidis, Moraxella catarrhalis, Bordetella pertussis, Listeria monocytogenes, Corynebacterium diphtheriae, Clostridium spp., Mycoplasma pneumoniae, Pasteurella multocida, Ureaplasma urealyticum, Chlamydia trachomatis, Chl. pneumoniae, Chl. psittaci, Legionella pneumophila, Campylobacter spp., Gardnerella vaginalis [13]. In our practice, we prescribe individual local therapy to patients with varying degrees of severity of CVI of the lower extremities and skin changes with manifestations of secondary infection, including: local antibacterial drugs in combination with topical glucocorticosteroids in the appropriate form (cream, emulsion, aerosol, powder); solutions of aniline dyes; topical preparations containing heparin and dimethyl sulfoxide; topical silver preparations; keratoplasty ointments for severe peeling, containing salicylic and lactic acid; moisturizers with epithelializing effect; angioprotectors. In order to inhibit the vital activity of microorganisms pathogenetically associated with the occurrence and development of infection in the zone of trophic disorders, we recommend that all patients take oral roxithromycin (Esparoxy) 150 mg 2 times a day, with an interval of 12 hours, or 300 mg once for 10 days. In all patients, a week after the start of the therapy described above, there was a complete disappearance of clinical signs of bacterial infection and a visible decrease in the severity of inflammatory changes on the skin (Fig. 1–3). Patients note a significant reduction in pain and itching.
We attribute the achieved effect to the fact that the semisynthetic antibiotic of the macrolide group has a bacteriostatic effect: by binding to the 50S subunit of ribosomes, it suppresses translocation and transpeptidation reactions, the process of formation of peptide bonds between amino acids and the peptide chain, inhibits protein synthesis by ribosomes, resulting in inhibition of growth and reproduction bacteria. Oral administration of the macrolide antibiotic roxithromycin (Esparoxy) allows these patients to be treated in an outpatient setting, significantly increasing patient compliance.
Conclusion
Patients with pathology of hemodynamics of the extremities require joint supervision of a surgeon and a dermatologist. The success of therapy depends on clear and coordinated actions of specialists. Treatment of the patient should be comprehensive, including therapy not only with vascular agents, but also an optimal combination of topical drugs, as well as timely systemic antibiotic therapy. At the same time, macrolide antibiotics, including roxithromycin (Esparoxy), can be successfully used in the treatment of secondary infection of the skin and soft tissues in patients with CVI.
Is it worth using folk remedies?
You can find a lot of “folk art” recipes that help with varicose veins and combat its consequences. They contain cabbage leaves, nettles, green tomatoes, butter with garlic and other familiar products.
Some “healers” advise walking barefoot through the dew at dawn, wiping the affected areas of the skin with apple cider vinegar, and applying horseradish leaves to the wounds.
Doctors warn that such treatment will be absolutely useless. Moreover, ignoring drug therapy and doctor’s recommendations provokes rapid progression of the problem. The result will be deep trophic ulcers - bleeding, with purulent filling: a photo of varicose eczema in an advanced stage clearly demonstrates this.
The only thing phlebologists allow is taking infusions with a diuretic effect, which will remove excess fluid from the body and make swelling less pronounced. The following will be useful:
- infusion of lingonberry leaves - 2 tablespoons of dry raw material per 300 ml of boiling water, leave for 1 hour and drink;
- decoction of rose hips - 1 tablespoon per 200 ml of water, boil in a water bath for 5 minutes, leave for 20 minutes and drink;
- bearberry infusion - the raw material is sold at the pharmacy, 1 teaspoon per 300 ml of boiling water will be enough.
Treatment of the root cause of eczema with varicose veins
In order for the treatment to be successful and for complete recovery to occur, the doctor will also prescribe therapy for the underlying disease. Most often it is varicose veins of the lower extremities, which is treated:
- sclerotherapy – a drug is injected into a vein, which “glues” the walls of the damaged vessel;
- laser therapy – vessels with a diameter of 2-3 mm are removed, the effect is carried out without incisions;
- laser coagulation - used to treat large vessels, during which the expansion is simply narrowed;
- miniphlebectomy – altered vessels are completely removed;
- full phlebectomy – the entire trunk of the saphenous vein is removed.
Preventive actions
You can avoid the development of venous eczema by following doctors’ recommendations for prevention:
- stop drinking alcohol and tobacco;
- drink 1.5-2 liters of clean water per day - this prevents blood thickening and facilitates blood flow in the affected vessels;
- Take daily walks, give moderate stress to the lower limbs.
The most important point is that you can avoid problems with the skin and prevent the formation of trophic ulcers only with the help of doctors: treatment of the underlying disease, normalization of nutrition.
Eczema is a serious lesion of the skin of the lower extremities, which is not included in the list of independent diseases. This is a complication of varicose veins and other vascular pathologies. Treatment should proceed only under the supervision of a doctor and with the obligatory elimination of the underlying cause.
Still have questions about varicose eczema?
Free consultation with AngioClinic specialists
Author
Salmina Daria Vladimirovna
Geneticist. Graduated from the Chelyabinsk State Medical Academy. She completed an internship at the Northwestern State Medical University named after I.I. Mechnikov.
Bibliography
- Dakhovsky, A. Skin diseases / A. Dakhovsky, N. Stogova. - M.: Book on Demand, 2011. - 761 p.
- Gadzhimuradov, M. N. Clinical features of Kirle’s disease [Text] / M. N. Gadzhimuradov // Clinical dermatology and venereology. - 2021. - No. 1. - P. 16-19.
- Zudin B.I. Skin and venereal diseases. Textbook. Ed. 2nd, revised and additional - M.: Medicine, 1996, 256 p.
- Sokolova, T. V. Strategy for choosing external therapy for microbial eczema [Text] / T. V. Sokolova, A. P. Malyarchuk, L. A. Safonova // Clinical dermatology and venereology. - 2021. - No. 3. - P. 46-63.
- Therapy of chronic dermatoses [Text]: [conversation with Ph.D. Assoc. department Dermatovenerology of the First Moscow Moscow. honey. University named after I. M. Sechenova T. A. Belousova / interviewed by N. Marchenko] // Medical Council. - 2017. - No. 11. - P. 80-82. 88.
- UVB 311 NM phototherapy for immune-dependent dermatoses [Text]: educational method. allowance / E. S. Ponich [etc.] // Physiotherapist. - 2017. - No. 2. - P. 57-64.