Doctors Cost
Price list Doctors clinic
Anemia is a whole category of syndromes characterized by a decrease in hemoglobin concentration and the number of red blood cells. This condition is diagnosed only by the results of laboratory tests; it is impossible to determine the disease by eye. Symptoms of anemia in adults can vary greatly. Therefore, the direction of treatment depends on the general state of health, the causes of the disease, age and gender, and concomitant pathologies.
Anemia - what is it and how dangerous is it?
This disease is also called anemia. This is a clinical-hematological syndrome that can occur as a consequence of one or another pathology. Hemoglobin protein is synthesized in the bone marrow with the participation of iron and is a component of erythrocytes - red blood cells. It delivers oxygen to the tissues and also helps to utilize carbon dioxide, delivering it to the lungs.
Such an important function easily explains the dangerous consequences of anemia. Firstly, even in conditions of a lack of iron in the diet, the body will fight anemia with all its might: first there will not be enough iron in the tissues and organs, and only lastly in the blood. This means that anemia often accompanies serious bone marrow diseases, tumors, and severe hematological diseases. It is important to pay attention to anemia as early as possible for this reason.
Secondly, a decrease in hemoglobin levels can lead to the following consequences:
- weakening of protective forces and increased susceptibility to aggressive environmental factors;
- decreased physical endurance and tolerance to intellectual stress;
- high risks of developing heart disease;
- high risks of developing purulent-septic processes.
Pregnant women deserve special attention. Anemia during pregnancy can lead to a high probability of spontaneous abortion, fetal malnutrition and intrauterine growth retardation, the appearance of hypoxia, and discoordination of labor. Physiological blood loss during childbirth or during a cesarean section will not cause complications in a healthy woman, but in an expectant mother with anemia it can also cause serious consequences.
Functions and norms of platelets
Platelets are blood cells that are necessary for blood clotting. Their production occurs in the bone marrow. Platelets create clots that clog damaged vessels and stop bleeding. They also make the walls of blood vessels elastic due to nutrients.
The normal platelet count in the analysis is 100 – 400 g/l. Exceeding the permissible values means thrombocytosis. The blood becomes thicker, increasing the risk of blood clots, which can be life-threatening. If the platelet count is low, the condition is called thrombocytopenia. In this case, the blood does not clot well and it can be very difficult to stop the bleeding. This pathology threatens the patient with significant blood loss even with small wounds. Bruises often appear on the body.
Important! In women, by the end of menstruation, hemoglobin decreases and platelet levels increase.
Symptoms of anemia
Symptoms of anemia and treatment options may vary in patients of different age groups, gender, and general health. The most characteristic signs are the following:
- pallor of the skin (from white to yellowish) and mucous membranes;
- hair loss (not patchy baldness, but uniform hair loss);
- brittle nails, changes in the structure of the nail plate, suddenly appearing white spots on the nails;
- change in taste sensations, burning sensation on the tongue;
- cracks in the corners of the mouth;
- menstrual cycle disorders in women;
- decreased physical activity, resistance to physical activity;
- muscle weakness;
- increased drowsiness;
- rapid mood changes, irritability;
- dizziness, periodic headaches, less often fainting;
- ringing in the ears, darkening or spots in the eyes;
- unusual gastronomic preferences, for example, the desire to taste paints, soil, chalk, etc.;
- pain behind the sternum, usually in the heart area.
In each specific case, not all of the listed symptoms may be observed. Sometimes anemia is discovered by chance, during the diagnosis of general health, when the patient came to the doctor for another reason. Thus, frequent respiratory diseases are a common consequence of anemia, and consulting a doctor allows you to identify the true causes of constant ailments.
Differences between anemia in adults and children
According to WHO, about 2 billion people in the world suffer from anemia. The majority are children of different ages. Almost half of them are preschoolers, and a little more than a quarter are young school-age patients. And in adults, the disease occurs quite often. This syndrome is dangerous for both children and adults, and in adults the treatment period is somewhat longer.
Anemia in children may be associated with a specific cause: periods of rapid growth. The mechanisms of hematopoiesis are still imperfect, and the growth spurt requires an increased amount of nutrients. This may be associated with a temporary decrease in hemoglobin levels in the blood. However, this is still not a variant of the norm, but a syndrome that deserves close attention from a doctor. Anemia can lead to decreased defenses, poor weight gain, loss of appetite, weakness, and tearfulness. Timely methods of diagnosing and treating anemia will allow you to correct the condition and prevent complications.
The most dangerous complication of iron deficiency anemia (IDA) in adults is hypoxic coma. With high blood loss, it can cause death. Therefore, it is important to consult a doctor in time.
Why is blood thickening dangerous?
If the blood becomes thicker, this condition is associated with many problems. Its stagnation in organs prevents them from functioning normally. The risk of blood clots increases significantly. Even one blood clot can cause death or disability.
The speed of blood flow slows down, which puts increased stress on the heart and blood vessels. Cells do not receive enough oxygen and nutrients. Radicals are released. Plaques and blood clots form in the vessels. This means that thrombosis has begun to develop. It is the most common cause of strokes and heart attacks. In pregnant women, this problem leads to the birth of an underdeveloped child or a miscarriage.
Important! Blood thinning is facilitated by an active lifestyle and regular exposure to fresh air.
How to thin thick blood in adults
Treatment for thrombocytosis will depend on its cause. Usually it includes not only taking medications, but also diet. Often, adjusting your diet and increasing the amount of fluid consumed per day gives good results. Thinning medications help make the blood less viscous and thicker. When more effective methods are needed, the doctor may prescribe a course of plateletpheresis. This procedure is carried out using an electrical device. If thrombocytosis was caused by infection or autoimmune processes, appropriate therapy is carried out.
Among the traditional methods, hirudotherapy helps. The substance secreted by leeches during suction is called a natural anticoagulant. At the same time, the blood acquires new physical properties, its composition also changes for the better. It is recommended to eat more berries, beets, onions, garlic and tomatoes. Fish and fish oil are very useful for such patients. Olive and flaxseed oil, ginger and seeds have a beneficial effect. You need to avoid salty and fatty meat dishes. You should eat less bananas, white bread and lentils.
How to lower hemoglobin in children
With age, human blood becomes thicker due to the slow elimination of waste products. If hemoglobin and platelets are elevated in a child, this is an alarming symptom. It threatens possible disruption of life processes. Of course, only a specialist can find out the cause and prescribe adequate therapy for the baby. But parents can also do something to improve the condition.
Excess protein should be removed from the child’s diet. Give him less meat, liver and other offal. It is important to ensure that the patient receives plenty of clean drinking water. It is better to give preference to fish and plant products. Milk, kefir, yogurt, fermented baked milk help reduce hemoglobin. With such a diet, the child’s body will experience a lack of protein, which it needs for normal growth and development. Therefore, it is useful to replace meat with legumes, soy and chicken breast. To avoid the formation of blood clots in blood vessels, it is necessary to reduce the amount of fatty foods. But seafood is healthy because... strengthen the walls of blood vessels.
Important! Smoking and other bad habits provoke blood thickening.
The consistency of blood largely depends on the amount of hemoglobin and platelets. When it thickens, blood clots form, which pose a real threat to health and life. Medicines and diet will help fight them.
Why does anemia occur?
Anemia can be caused by many factors. There is often a combination of causes that quickly lead to blood disorders. The most common factors for the development of anemia:
- diet features. This is the most insidious reason. The lack of food rich in iron and B vitamins may not be taken seriously by a person. This is observed with a meager diet in women trying to lose extra pounds, the need to follow a certain table for gastrointestinal diseases, etc.;
- dysfunction of the digestive system. Even a complete diet does not guarantee the absence of anemia if iron cannot be absorbed in full due to gastrointestinal diseases. Iron absorption occurs in the stomach and upper small intestine. Diseases of these organs can lead to disruption of the process and the development of IDA;
- diseases leading to disruption of red blood cell production in the bone marrow. Such diseases include pathologies of the kidneys and endocrine system, protein depletion, chronic infections, cancerous tumors;
- hemolysis. This is a condition in which red blood cells are destroyed prematurely. Normally, physiological hemolysis occurs no earlier than after 120 days—that’s how long the red blood cell “lives.” In pathological conditions, the lifespan of red blood cells decreases, causing anemia. This may be due to long-term drug therapy, infectious diseases, rheumatism, systemic diseases (scleroderma, etc.), kidney diseases, etc.;
- chronic blood loss. Blood loss is a common cause of anemia. These include heavy menstruation in women or a short (21 days or less) menstrual cycle, frequent nosebleeds or bleeding gums, gastrointestinal bleeding, non-healing wounds in people with diabetes, previous surgeries, childbirth, etc.
Anemia is always the result of an underlying disorder, so it is important to get accurate information about the causes. It is not recommended to engage in self-diagnosis and self-medication. Taking iron supplements can correct the condition, but will not get rid of the underlying disease, so it will not be fully effective and there is a high probability of relapse.
The approach to treating anemia depends on what causes the disease. Thus, secondary causes of the development of the syndrome include:
- refusal of protein foods, fasting due to life circumstances or beliefs. If a person is forced or prefers to give up food of animal origin and does not find a replacement for it in terms of iron content, deficiency and associated anemia develop;
- pregnancy. Hormonal changes, an increased need for vitamins and microelements can cause deficiency, including iron; anemia in pregnant women develops quite often. It is important to regularly visit an obstetrician-gynecologist and get tested on time so as not to miss possible violations;
- blood donation. Although blood donation is carried out taking into account safe blood loss, the risks of developing anemia increase. You should consult your doctor if you are acting as a donor;
- professional sports or increased physical activity. This is due to the fact that muscles require increased amounts of iron. The peculiarity of this cause is that anemia occurs in an erased form, because usually an athlete leads an active and healthy lifestyle. It is important to pay attention to fatigue, intolerance to previously habitual stress, and shortness of breath.
MEDICAL CENTER
Interpretation of study results contains information for the attending physician and is not a diagnosis.
The information in this section should not be used for self-diagnosis or self-treatment. The doctor makes an accurate diagnosis using both the results of this examination and the necessary information from other sources: medical history, results of other examinations, etc. Hemoglobin (Hb, hemoglobin) Units of measurement in the medical center STUDIO DOCTOR: g/dl. Alternative units: g/l. Conversion factor: g/l x 0.1 ==> g/dl. Reference values
| Age, gender | Hemoglobin level, g/dl | |
| Children | ||
| 1 day - 14 days | 13,4 — 19,8 | |
| 14 days - 4.3 weeks | 10,7 — 17,1 | |
| 4.3 weeks - 8.6 weeks | 9,4 — 13,0 | |
| 8.6 weeks - 4 months | 10,3 — 14,1 | |
| 4 months – 6 months | 11,1 — 14,1 | |
| 6 months – 9 months | 11,4 — 14,0 | |
| 9 months - 12 months | 11,3 — 14,1 | |
| 12 months - 5 years | 11,0 — 14,0 | |
| 5 years - 10 years | 11,5 — 14,5 | |
| 10 years - 12 years | 12,0 — 15,0 | |
| 12 years - 15 years | Women | 11,5 — 15,0 |
| Men | 12,0 — 16,0 | |
| 15 years - 18 years | Women | 11,7 — 15,3 |
| Men | 11,7 — 16,6 | |
| 18 years - 45 years | Women | 11,7 — 15,5 |
| Men | 13,2 — 17,3 | |
| 45 years - 65 years | Women | 11,7 — 16,0 |
| Men | 13,1 — 17,2 | |
| > 65 years old | Women | 11,7 — 16,1 |
| Men | 12,6 — 17,4 | |
Increased hemoglobin levels:
- dehydration (with severe diarrhea, vomiting, increased sweating, diabetes, burn disease, peritonitis);
- physiological erythrocytosis (in residents of high mountains, pilots, athletes);
- symptomatic erythrocytosis (with insufficiency of the respiratory and cardiovascular systems, polycystic kidney disease);
- erythremia.
Decreased hemoglobin:
- anemia of various etiologies;
- overhydration.
Hematocrit (Ht, hematocrit)
Units of measurement in the medical center STUDIO DOCTOR: %.
Reference values
| Age, gender | Hematocrit indicator, % | |
| Children | ||
| 1 day - 14 days | 41,0 — 65,0 | |
| 14 days - 4.3 weeks | 33,0 — 55,0 | |
| 4.3 weeks - 8.6 weeks | 28,0 — 42,0 | |
| 8.6 weeks - 4 months | 32,0 — 44,0 | |
| 4 months – 9 months | 32,0 — 40,0 | |
| 9 months - 12 months | 33,0 — 41,0 | |
| 12 months - 3 years | 32,0 — 40,0 | |
| 3 years - 6 years | 32,0 — 42,0 | |
| 6 years - 9 years | 33,0 — 41,0 | |
| 9 years - 12 years | 34,0 — 43,0 | |
| 12 years - 15 years | Women | 34,0 — 44,0 |
| Men | 35,0 — 45,0 | |
| 15 years - 18 years | Women | 34,0 — 44,0 |
| Men | 37,0 — 48,0 | |
| 18 years - 45 years | Women | 35,0 — 45,0 |
| Men | 39,0 — 49,0 | |
| 45 years - 65 years | Women | 35,0 — 47,0 |
| Men | 39,0 — 50,0 | |
| 65 years - 120 years | Women | 35,0 — 47,0 |
| Men | 37,0 — 51,0 | |
Increased hematocrit:
- dehydration (with severe diarrhea, vomiting, increased sweating, diabetes, burn disease, peritonitis);
- physiological erythrocytosis (in residents of high mountains, pilots, athletes);
- symptomatic erythrocytosis (with insufficiency of the respiratory and cardiovascular systems, polycystic kidney disease);
- erythremia.
Decreased hematocrit:
- anemia of various etiologies;
- overhydration.
Red blood cells
Units of measurement at the STUDIO DOCTOR medical center: million/µl (106/µl). Alternative units: 1012 cells/L.
Conversion factors: 1012 cells/l = 106 cells/μl = million/μl.
Reference values
| Age, gender | Red blood cells, million/µl (x106/µl) | |
| Children | ||
| 1 day - 14 days | 3,90 — 5,90 | |
| 14 days - 4.3 weeks | 3,30 — 5,30 | |
| 4.3 weeks - 4 months | 3,50 — 5,10 | |
| 4 months – 6 months | 3,90 — 5,50 | |
| 6 months – 9 months | 4,00 — 5,30 | |
| 9 months - 12 months | 4,10 — 5,30 | |
| 12 months - 3 years | 3,80 — 4,80 | |
| 3 years - 6 years | 3,70 — 4,90 | |
| 6 years - 9 years | 3,80 — 4,90 | |
| 9 years - 12 years | 3,90 — 5,10 | |
| 12 years - 15 years | Women | 3,80 — 5,00 |
| Men | 4,10 — 5,20 | |
| 15 years - 18 years | Women | 3,90 — 5,10 |
| Men | 4,20 — 5,60 | |
| 18 years - 45 years | Women | 3,80 — 5,10 |
| Men | 4,30 — 5,70 | |
| 45 years - 65 years | Women | 3,80 — 5,30 |
| Men | 4,20 — 5,60 | |
| 65 years - 120 years | Women | 3,80 — 5,20 |
| Men | 3,80 — 5,80 | |
Increased red blood cell concentration:
- dehydration (with severe diarrhea, vomiting, increased sweating, diabetes, burn disease, peritonitis);
- physiological erythrocytosis (in residents of high mountains, pilots, athletes);
- symptomatic erythrocytosis (with insufficiency of the respiratory and cardiovascular systems, polycystic kidney disease);
- erythremia.
Decreased red blood cell concentration:
- anemia of various etiologies;
- overhydration.
MCV (mean erythrocyte volume) Determination method: calculated value. Units of measurement at the STUDIO DOCTOR medical center: fl (femtoliter). Reference values
| Age, gender | Mean erythrocyte volume, MCV, fl | |
| Children | ||
| 1 day - 14 days | 88,0 — 140,0 | |
| 14 days - 4.3 weeks | 91,0 — 112,0 | |
| 4.3 weeks - 8.6 weeks | 84,0 — 106,0 | |
| 8.6 weeks - 4 months | 76,0 — 97,0 | |
| 4 months – 6 months | 68,0 — 85,0 | |
| 6 months – 9 months | 70,0 — 85,0 | |
| 9 months - 12 months | 71,0 — 84,0 | |
| 12 months - 5 years | 73,0 — 85,0 | |
| 5 years - 10 years | 75,0 — 87,0 | |
| 10 years - 12 years | 76,0 — 90,0 | |
| 12 years - 15 years | Women | 73,0 — 95,0 |
| Men | 77,0 — 94,0 | |
| 15 years - 18 years | Women | 78,0 — 98,0 |
| Men | 79,0 — 95,0 | |
| 18 years - 45 years | Women | 81,0 — 100,0 |
| Men | 80,0 — 99,0 | |
| 45 years - 65 years | Women | 81,0 — 101,0 |
| Men | 81,0 — 101,0 | |
| 65 years - 120 years | Women | 81,0 — 102,0 |
| Men | 83,0 — 103,0 | |
Increasing MCV values:
- B12 deficiency and folate deficiency anemia;
- aplastic anemia;
- liver diseases;
- hypothyroidism;
- autoimmune anemia;
- smoking and drinking alcohol.
Reducing MCV values:
- Iron-deficiency anemia;
- anemia of chronic diseases;
- thalassemia;
- some types of hemoglobinopathies.
It should be taken into account that the MCV value is not specific; the indicator should be used to diagnose anemia only in combination with other indicators of a general blood test and biochemical blood test.
RDW (Red cell Distribution Width, distribution of red blood cells by size)
Method of determination: calculated value Units of measurement in the medical center STUDIO DOCTOR: %
Reference values
< 6 months — 14.9 – 18.7
> 6 months — 11.6 – 14.8
Increasing RDW values:
- anemia with heterogeneity of red blood cell size, including those associated with nutrition; myelodysplastic, megaloblastic and sideroblastic types; anemia accompanying myelophthisis; homozygous thalassemia and some homozygous hemoglobinopathies;
- a significant increase in the number of reticulocytes (for example, due to successful treatment of anemia);
- condition after red blood cell transfusion;
- interferences – cold agglutinins, chronic lymphocytic leukemia (high number of leukocytes), hyperglycemia.
There are also a number of anemias that are not characterized by an increase in RDW:
- anemia of chronic diseases;
- anemia due to acute blood loss;
- aplastic anemia
- some genetically determined diseases (thalassemia, congenital spherocytosis, presence of hemoglobin E).
It should be taken into account that the value of the RDW indicator is not specific; the indicator should be used to diagnose anemia only in combination with other indicators of a general blood test and biochemical blood test.
MCH (average amount of hemoglobin in 1 red blood cell)
Determination method: calculated value.
Units of measurement and conversion factors: pg (picograms).
Reference values
| Age, gender | Average hemoglobin content in 1 red blood cell, MCH, pg | |
| Children | ||
| 1 day - 14 days | 30,0 — 37,0 | |
| 14 days - 4.3 weeks | 29,0 — 36,0 | |
| 4.3 weeks - 8.6 weeks | 27,0 — 34,0 | |
| 8.6 weeks - 4 months | 25,0 — 32,0 | |
| 4 months – 6 months | 24,0 — 30,0 | |
| 6 months – 9 months | 25,0 — 30,0 | |
| 9 months - 12 months | 24,0 — 30,0 | |
| 12 months - 3 years | 22,0 — 30,0 | |
| 3 years - 6 years | 25,0 — 31,0 | |
| 6 years - 9 years | 25,0 — 31,0 | |
| 9 years - 15 years | 26,0- 32,0 | |
| 15 - 18 years old | Women | 26,0 — 34,0 |
| Men | 27,0 — 32,0 | |
| 18 – 45 years old | Women | 27,0 — 34,0 |
| Men | 27,0 — 34,0 | |
| 45 – 65 years | Women | 27,0 — 34,0 |
| Men | 27,0 — 35,0 | |
| 65 years - 120 years | Women | 27,0 — 35,0 |
| Men | 27,0 — 34,0 | |
Increasing MCH values:
- B12 deficiency and folate deficiency anemia;
- aplastic anemia;
- liver diseases;
- hypothyroidism;
- autoimmune anemia;
- smoking and drinking alcohol.
MCH Downgrade:
- Iron-deficiency anemia;
- anemia of chronic diseases;
- some types of hemoglobinopathies.
It should be taken into account that the MCH value is not specific; the indicator should be used to diagnose anemia only in combination with other indicators of a general blood test and biochemical blood test. MCHC (mean erythrocyte hemoglobin concentration) Determination method: calculated value
Units of measurement at the STUDIO DOCTOR medical center: g/dl. Alternative units: g/l. Conversion factor: g/l x 0.1 ==> g/dl.
Reference values
| Age, gender | Average hemoglobin concentration in erythrocytes, MSHC, g/dl | |
| Children | ||
| 1 day - 14 days | 28,0 — 35,0 | |
| 14 days - 4.3 weeks | 28,0 — 36,0 | |
| 4.3 weeks - 8.6 weeks | 28,0 — 35,0 | |
| 8.6 weeks - 4 months | 29,0 — 37,0 | |
| 4 months – 12 months | 32,0 — 37,0 | |
| 12 months - 3 years | 32,0 — 38,0 | |
| 3 years - 12 years | 32,0 — 37,0 | |
| 12 years - 15 years | Women | 32,0 — 36,0 |
| Men | 32,0 — 37,0 | |
| 15 years - 18 years | Women | 32,0 — 36,0 |
| Men | 32,0 — 36,0 | |
| 18 years - 45 years | Women | 32,0 — 36,0 |
| Men | 32,0 — 37,0 | |
| 45 years - 65 years | Women | 31,0 — 36,0 |
| Men | 32,0 — 36,0 | |
| 65 years - 120 years | Women | 32,0 — 36,0 |
| Men | 31,0 — 36,0 | |
Increased MSHC values: hereditary microspherocytic anemia. Decrease in MCHC values:
- Iron-deficiency anemia;
- anemia of chronic diseases;
- some types of hemoglobinopathies.
It should be taken into account that the MCHC value is not specific; the indicator should be used to diagnose anemia only in combination with other indicators of a general blood test and biochemical blood test.
Platelets Determination method: conductometry using the hydrodynamic focusing method.
Determination method: conductometry using the hydrodynamic focusing method. Units of measurement at the STUDIO DOCTOR medical center: thousand/μL (103 cells/μL). Alternate units: 109 cells/L. Conversion factors: 109 cells/l = 103 cells/µl = thousand/µl. Reference values:
| Age | Platelet concentration, thousand/µl (103 cells/µl) | |
| Children | boys | girls |
| 1 day - 14 days | 218 — 419 | 144 — 449 |
| 14 days - 4.3 weeks | 248 — 586 | 279 — 571 |
| 4.3 weeks - 8.6 weeks | 229 — 562 | 331 — 597 |
| 8.6 weeks - 6 months | 244 — 529 | 247 — 580 |
| 6 months - 2 years | 206 — 445 | 214 — 459 |
| 2 years - 6 years | 202 — 403 | 189 — 394 |
| Age | Platelet concentration, thousand/µl (103 cells/µl) | |
| 6 years - 120 years | 150 — 400 | |
Increased platelet concentration:
- physical stress;
- inflammatory diseases, acute and chronic;
- hemolytic anemia;
- anemia due to acute or chronic blood loss;
- conditions after surgical interventions;
- condition after splenectomy;
- oncological diseases, including hemoblastosis.
Decreased platelet concentration:
- pregnancy;
- B12 deficiency and folate deficiency anemia;
- aplastic anemia;
- viral and bacterial infections;
- taking medications that inhibit platelet production;
- congenital thrombocytopenia;
- splenomegaly;
- autoimmune diseases;
- conditions after massive blood transfusions.
Leukocytes Determination method: conductometry using the hydrodynamic focusing method. Units of measurement at the STUDIO DOCTOR medical center: thousand/μL (103 cells/μL). Alternate units: 109 cells/L. Conversion factors: 109 cells/l = 103 cells/µl = thousand/µl. Reference values:
| Age | Leukocyte concentration, thousand/µl (103 cells/µl) |
| 1 day – 12 months | 6,0 – 17,5 |
| 12 months – 2 years | 6,0 – 17,0 |
| 2 years – 4 years | 5,5 – 15,5 |
| 4 years – 6 years | 5,0 – 14,5 |
| 6 years – 10 years | 4,50 – 13,5 |
| 10 years – 16 years | 4,50 – 13,0 |
| 16 years – 120 years | 4,50 – 11,0 |
Increased leukocyte concentration:
- physiological leukocytosis (emotional and physical stress, exposure to sunlight, cold, food intake, pregnancy, menstruation);
- inflammatory processes;
- viral and bacterial infections;
- conditions after undergoing surgical interventions;
- intoxication;
- burns and injuries;
- heart attacks of internal organs;
- malignant neoplasms;
- hemoblastoses.
Decreased leukocyte concentration:
- viral and some chronic infections;
- taking medications (antibiotics, cytostatics, non-steroidal anti-inflammatory drugs, thyreostatics, etc.);
- autoimmune diseases;
- exposure to ionizing radiation;
- wasting and cachexia;
- anemia;
- splenomegaly;
- hemoblastoses.
Classification of anemia
Anemia is classified according to the color index, which shows the level of saturation of the red blood cell with hemoglobin. The following types of syndrome are distinguished:
- hypochromic (iron deficiency, thalassemia, anemia associated with a lack of vitamin B6, etc.);
- normochromic (hemolytic, posthemorrhagic, i.e. resulting from blood loss/surgery, aplastic, etc.);
- hyperchromic (vitamin B12 deficiency, folate deficiency, etc.).
We see that anemia is not always synonymous with iron deficiency. Deficiency of B vitamins can also cause the development of the syndrome, and quite often it is associated with diet or absorption of nutrients in the intestines. And in this regard, independent diagnosis is impossible: only a doctor can determine the type of anemia, identify the causes and correctly correct the condition.
Treatment also depends on the severity of the anemia. It is determined by the severity of the decrease in hemoglobin levels. There are three degrees of severity:
- light. Hemoglobin level from 90 g/l;
- average. Hemoglobin level 70–90 g/l;
- heavy. Hemoglobin level is less than 70 g/l.
Features and diagnostic methods
Diagnosis of anemia includes not only determining the fact of a decrease in hemoglobin levels. The doctor must understand the causes, assess the general state of health, and exclude severe pathologies that occur in a latent form, if they were not detected earlier. For this purpose, laboratory tests may be involved: a detailed clinical blood test is required. It will help assess the size, structural and other characteristics of blood cells.
The content of hemoglobin, erythrocytes, platelets, leukocytes, and several calculated erythrocyte indices are assessed. These indicators allow you to obtain data on the size, hemoglobin saturation, and uniformity of red blood cells. Determination of reticulocytes (young red blood cells) helps to understand the nature of anemia, as well as assess the reactivity of the hematopoietic system to the pathological condition. This is also important for monitoring treatment - the doctor can evaluate the response to the course of therapy.
Determination of erythrocyte parameters includes assessment of the following indicators:
- red blood cell count;
- hemoglobin concentration;
- average erythrocyte volume;
- hematocrit;
- width of distribution of red blood cells by volume;
- normoblasts.
The average volume and diameter of red blood cells are also assessed. An increase in these parameters may indicate a vitamin B12 deficiency. A decrease indicates a lack of iron.
Reticulocytosis or quantitative indicators of immature red blood cells may indicate certain features of bone marrow activity. In aplastic anemia associated with bone marrow suppression, the indicator may drop to zero. Reticulocytosis increases with blood loss and hemolytic anemia.
The doctor will also pay attention to those blood parameters that are not directly related to red blood cells. For example, an increase in platelet levels may be a consequence of IDA due to chronic blood loss. If leukocytes and platelets are reduced, we can talk about aplastic anemia. Detection of blast cells requires special attention; there is a high probability of acute leukemia.
Although laboratory diagnosis is critical, it is important to resort to other research methods. An examination is mandatory - the doctor evaluates the color of the skin and mucous membranes. Palpation helps to suspect possible disorders of internal organs and tumors. A thorough survey allows you to identify lifestyle features, probable causes, and the duration of symptoms.
If you have symptoms of anemia, it is important to consult a general practitioner or hematologist. He will order the necessary tests and make suggestions as to the reasons. To clarify them, it is sometimes necessary to resort to additional diagnostic tools:
- fibrogastroduodenoscopy. Assessing the condition of the mucous membranes of the esophagus and stomach will help in identifying gastric bleeding;
- Ultrasound of the liver and kidneys;
- examination of the pelvic organs in women;
- CT or MRI if indicated;
- colonoscopy;
- X-ray of the lungs, etc.
A complete list of diagnostic methods is not required: a specialist will find out the possible causes and refer you to certain studies according to indications. If necessary, he can refer you to another doctor. So, if the cause of anemia is heavy and prolonged menstruation or a short cycle, an examination by a gynecologist will be required. Detection of gum problems (bleeding) and symptoms of periodontal disease will require a visit to a periodontist. Frequent nosebleeds are a reason to consult an otolaryngologist, assess blood pressure parameters, etc.
Hematologist: who is he, for what symptoms and diseases should you make an appointment with a doctor?
Table of contents
- Hematologist: what does it treat?
- Pediatric hematologist: who is he and what does he treat?
- Help from a hematologist during pregnancy
- When to go to a hematologist?
- Preparing for a consultation
- Blood tests to be taken before consultation
- Stages of consultation with a hematologist
- Diagnostics
- Treatment
- Advantages of visiting a hematologist at MEDSI
A hematologist is a doctor who deals with the prevention, diagnosis and treatment of diseases of the blood and hematopoietic organs.
This specialist works with children and adults and uses both traditional and modern techniques in his practice. It can successfully identify even hidden pathologies that do not manifest significant symptoms.
Hematologist: what does it treat?
These specialists provide therapy for the following diseases:
- Anemia.
This pathology is characterized by a decrease in red blood cells and hemoglobin. Anemia is not a separate disease! This is a symptom of mycosis, pyelonephritis, tuberculosis and other dangerous conditions. It is usually accompanied by weakness, general malaise, appetite and sleep disturbances, shortness of breath even with moderate exertion, and poor concentration. - Lymphocytic leukemia.
This disease is malignant and is characterized by the proliferation of atypical B lymphocytes that accumulate in the bone marrow, spleen, liver and lymph nodes. A predisposition to the pathology is inherited, and its main symptoms include enlarged lymph nodes, excessive sweating, weakness and sudden weight loss. As lymphocytic leukemia develops, an enlarged spleen and liver, anemia, dizziness, and spontaneous bleeding are detected - Multiple myeloma.
This pathology is malignant and is distinguished by the ability of tumor cells to synthesize homogeneous immunoglobulins or their fragments. The tumor is formed predominantly in the bone marrow and can be focal, diffuse or focal-diffuse - Myeloid leukemia.
This form of leukemia is characterized by the rapid division of special cells in the bone marrow and their accumulation in the blood. Usually it is diagnosed only during a clinical analysis, since often the pathology does not manifest itself in any way. In some cases, patients complain of a slight increase in body temperature, decreased immunity and general malaise. It is also possible to detect anemia and an enlarged spleen - Lymphomas.
This pathology is characterized by enlarged lymph nodes. The primary tumor site usually metastasizes and spreads throughout the body. There are several forms of lymphoma, which differ in symptoms and degree of malignancy.
Specialists also treat other diseases.
Pediatric hematologist: who is he and what does he treat?
This specialist deals with the treatment and prevention of diseases that occur in both children and adults. Working with patients under 18 years of age, he takes into account all the features of their age and development.
They are referred to such doctors if they suspect various forms of anemia, thrombocytopenia (decreased platelet count), hemorrhagic vasculitis (inflammation of microvessels), hemophilia and other congenital hereditary disorders.
Important! If blood diseases are detected at an early age, the patient should be under medical supervision for as long as possible. It is very important not only to detect pathology, but also to control it. Only in this case can the correct growth and development of the child be ensured.
Help from a hematologist during pregnancy
A large number of blood diseases are inherited, for this reason it is very important to visit a doctor when planning a child and during pregnancy. The specialist will provide the necessary genetic tests and determine the likelihood of developing abnormalities. It is especially important to contact a hematologist if one or both future parents have pathologies.
In addition, it is very important for a pregnant woman to monitor all blood parameters, since the supply of oxygen and other nutrients to the fetus largely depends on them. Consultation with a doctor is required for various deviations from the norm. It is especially important to quickly seek medical help if you suspect the development of iron deficiency anemia. This problem is one of the most common and needs correction and observation until birth.
When to go to a hematologist?
Consultation with a doctor is required for the following signs of various disorders:
- Enlarged lymph nodes
- Weakness and drowsiness
- Increased body temperature (not due to colds and inflammatory processes)
- Weight loss
- Sleep disorders
- Excessive sweating
- Pale skin
- Decreased appetite
- The appearance of bruises on the body without objective reasons
- Dizziness
Help is required for patients who complain of joint pain, itching, dry skin, tingling and numbness of the fingers. You should make an appointment with a hematologist if you have a hereditary predisposition to blood diseases and low hemoglobin detected as part of a general diagnosis. Both general practitioners, gastroenterologists, neurologists and other doctors can refer you to this specialist.
Preparing for a consultation
No special preparation is required for the standard appointment. Some restrictions are imposed only if the patient must first undergo tests.
Before research you must:
- Try to quit drinking alcohol and smoking for a few days
- Limit fluid intake (per day)
- Refuse to eat (10-12 hours before)
- Avoid the use of medications. If this is not possible, you should tell your doctor what medications are being taken, on what schedule and in what dosages. This will allow you to correctly decipher the diagnostic results
Blood tests to be taken before consultation
Before visiting a hematologist, you should undergo the following tests:
- Common with determination of the number of reticulocytes
(“young” red blood cells). This test will reveal the rate of red blood cell production in the bone marrow - For HIV, hepatitis and other infections
- For ferritin.
Such a study will determine the content of a protein in the blood that preserves iron in cells. - Percentage of transferrin saturation.
This test identifies a protein that binds to iron and distributes it throughout the body.
The research results will allow the specialist to immediately make a diagnosis and prescribe the necessary treatment. If necessary, other examinations will be recommended.
Stages of consultation with a hematologist
Conversation
It is aimed at collecting anamnesis. The patient is asked about the symptoms of the disease that have arisen. The doctor clarifies the time of appearance of signs of pathologies, their intensity and other features. The specialist also finds out hereditary predisposition to various diseases.
Inspection
The doctor assesses the condition of the skin and mucous membranes. During the examination, signs of disturbances in the functioning of the hematopoietic system may be revealed, such as pale skin, rashes, hematomas, cyanosis (bluish coloration).
Making a diagnosis or ordering additional examinations
If a patient contacts a hematologist with the results of blood tests, a diagnosis can be made immediately. If studies have not been carried out, the doctor will refer you to them. In some cases, not only laboratory but also instrumental examinations are required. The doctor writes out directions for them.
Diagnostics
Blood diseases have a variety of manifestations that are similar to other pathological conditions. Therefore, a wide range of examination techniques are used to identify them. The patient is required to undergo blood tests.
Also held:
- Urine tests
- Coagulogram
- Lymph node puncture
- Scintigraphy
- CT and MRI (computer and magnetic resonance imaging)
- X-ray of flat bones
- Ultrasound of the abdominal organs and lymph nodes
- Bone marrow puncture, etc.
Comprehensive diagnostics makes it possible to identify even hidden pathologies that have not yet manifested themselves.
Treatment
The treatment regimen and program are developed depending on the individual characteristics of the patient, general current condition, and the presence of concomitant diseases.
The main areas of treatment include:
- Antibacterial.
It is required for patients who suffer from a general decrease in immunity and are more susceptible to various infections than others. - Transfusion.
This therapy involves transfusion of blood and its components. - Supportive.
It is aimed at eliminating the symptoms of the disease and improving the general well-being of the patient. - Chemotherapy.
Prescribed to disrupt the processes of growth and reproduction, as well as necrosis of malignant cells - Medication.
This treatment is carried out to replenish the deficiency of various elements, correct the functioning of the blood coagulation system and accelerate metabolic processes - Radiation therapy.
Prescribed in combination with other manipulations to combat cancer pathologies
Doctors can also resort to hormonal treatment, bone marrow cell transplantation, and surgical interventions.
Important! As a rule, therapy is complex.
Advantages of visiting a hematologist at MEDSI
- Experienced doctors.
Our specialists have all the knowledge and skills necessary to treat pathologies even in advanced cases. If necessary, endocrinologists, gastroenterologists, etc. are involved in the work. - Comprehensive expert-level diagnostics.
We have modern equipment to conduct any examinations. Laboratory research can be performed in Cito mode (urgent) - Application of modern methods of treatment of various identified diseases.
This increases patients' chances of a full recovery. - Comfort of visiting a doctor.
We have ensured that there are no queues and offer to make an appointment for a consultation at a convenient time.
If you want to consult a hematologist, just contact us in any convenient way.
Treatment of anemia
Clinical recommendations for the treatment of anemia depend on many factors: gender, age and condition of the patient, type and severity of the syndrome. There are several general principles that apply in medical practice. These include the following:
- Mandatory diet correction for B12 deficiency and iron deficiency anemia. This complements the main course of treatment - taking medications that will compensate for the lack of substances;
- timely correction of deficiency of vitamins and microelements in pregnant women;
- mandatory consultation with a specialist when identifying specific causes: chronic bleeding, features of the functioning of the reproductive system in women, etc.;
- examination by a specialist in cases where anemia has caused complications in organs and systems. For example, consultation with a cardiologist for angina pectoris, low blood pressure, etc.
An integrated approach allows you to cope with the cause of the syndrome, rather than mask the symptom, and also eliminate or correct the consequences of the disease.
The main objectives of the treatment of anemia:
- eliminating the cause. Identification and elimination of the source of chronic blood loss, normalization of iron absorption in the intestines, reduction of blood loss during menstruation, etc.;
- replenishing the lack of important substances;
- prevention of the development of dystrophic changes in internal organs, restoration of their normal function.
It is important to remember that it is impossible to eliminate anemia with diet alone. This is explained by the fact that the absorption of iron from food is no more than 2.5 mg/day. From drugs, it is absorbed 20 times more. However, following a diet is very important as an addition to a course of drug therapy. Patients are recommended foods containing large amounts of digestible protein and iron.
Meat contains heme iron, which is absorbed by 30%. Also, liver, eggs and fish contain iron, which is absorbed by 10–15%. The microelement is also found in products of plant origin; absorption of Fe from legumes, spinach, soybeans, dill, and bread is up to 3–5%. It is advisable to include apples, pomegranates and pomegranate juice, beets, and buckwheat in your diet. But in terms of their overall benefits, the absorption of iron ions from them is limited, as demonstrated by numerous studies. That is why it is important to understand that eating apples will not help cure anemia; this is nothing more than a myth.
People who eat meat get more iron than those who are vegetarian. Strict vegetarianism can cause anemia because vegetables and grains contain substances that interfere with the absorption of iron. If you follow a normal, balanced diet, they do not entail serious consequences.
It is important to understand that a balanced diet helps cover the daily requirement, but will not eliminate iron deficiency. The basis of correction is drug therapy.
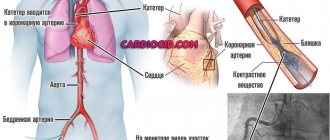
Blood transfusions (transfusions) are performed according to vital indications. They are usually carried out when hemoglobin drops below 50−40 g/l.
If the situation is not so severe, the doctor prescribes medication. IDA is corrected with oral medications; the course of treatment in adults is quite long. Interim monitoring is mandatory - detailed blood tests are performed. The principles of treatment in this case are as follows:
- prescribing iron supplements with a dose of divalent or trivalent iron sufficient for a person;
- supplementing the course of treatment with substances that enhance absorption. Succinic and ascorbic acid are used;
- refusal of antacids, oxalates and other drugs that reduce iron absorption whenever possible or recommendations for taking them at different times;
- therapy for at least 6–8 weeks until normalization and for at least another 4 weeks after improvement.
Let’s take a closer look at the recommendations about avoiding medications and foods that interfere with the absorption of iron. This can be prevented by phosphoric acid, calcium, tannin, phytin, and salts. Therefore, you should not drink tea, coffee, or Coca-Cola at the same time as taking iron.
For women suffering from long and heavy menstruation, not associated with diseases of the endocrine and reproductive systems, it is important to maintain monthly short courses of treatment: take average therapeutic doses of Fe for 3-5 days.
Clinical guidelines for the treatment of anemia dictate regular monitoring. The criterion for the effectiveness of therapy is an increase in reticulocytes at least three times 7-10 days after the start of treatment.
All iron preparations are classified into two groups: ionic (salt or polysaccharide compounds of ferrous iron) and non-ionic, consisting of a ferric iron complex.
Ferrous sulfate is included in mono- and polycomponent products and is well absorbed, and also has a relatively smaller list of side effects. Chloride compounds are absorbed less well and can also cause undesirable consequences: metallic taste in the mouth, dyspepsia, darkening of tooth enamel, etc. Modern treatment standards call for the use of ferrous or trivalent iron preparations.
Sometimes iron supplements are indicated to be administered parenterally. This is relevant for cases where there is a malabsorption in the intestine and other features. The main indications for drip infusion are the following:
- impaired intestinal absorption - malabsorption, previous surgery, etc.;
- intolerance to oral medications;
- the need for quick saturation. For example, in case of emergency surgery;
- treatment with erythropoietin: with it, the need for iron sharply increases, since it is actively consumed by red blood cells.
Important: parenteral administration requires no more than 100 mg/day. Otherwise, there is a risk of complications.
Treatment regimens for anemia associated with vitamin deficiency include additional intake of vitamin B12, folic acid and certain microelements.
Treatment of anemia associated with diseases of the hematopoietic organs and bone marrow tumors is developed individually and requires special attention to the cause.
Features of prevention
Prevention of anemia should be carried out in case of hidden signs of iron deficiency or the presence of risk factors for the development of the syndrome. Thus, if there are grounds for the rapid development of anemia, it is important to examine the level of hemoglobin and serum iron annually. The following patients are at risk:
- blood donors, especially females;
- pregnant women, especially those with frequent pregnancies;
- women with long (more than 5 days), heavy menstrual bleeding, short cycle (21–25 days);
- children from multiple pregnancies, premature babies;
- children during growth spurts;
- people with dietary restrictions;
- people suffering from chronic bleeding. For example, with hemorrhoids, etc.;
- patients taking non-steroidal anti-inflammatory drugs;
- professional athletes and people engaged in active physical labor.
Necessary diagnostics
The main method of diagnosis is a detailed blood test. One study will not be enough; it will have to be repeated a couple more times. This is done to eliminate errors and omissions. They rent it out at intervals of several days. The doctor should prescribe additional diagnostic tests.
Great importance is attached to the amount of serum ferritin. This protein contains iron, its content increases in the presence of inflammation. A hematologist will most likely refer such a patient for an ultrasound of the pelvic and abdominal organs. Women will have to visit a gynecologist, and men - a urologist. A colonoscopy may also be required. It is done when there is a possibility of pathologies in the intestines. The patient will need to monitor their temperature for a week. After receiving all the results, the doctor will be able to make a final diagnosis.