Vasculitis ( angiitis, arteritis ) is a general name for a group of diseases associated with inflammation and destruction of the walls of blood vessels. Inflammation of blood vessels can occur in any organ.
The disease vasculitis leads to the fact that the vessels cease to properly perform their function (supplying blood to tissues and removing metabolic products), so the organs adjacent to them are affected.
Vasculitis has different classifications and may differ in localization, etiology and severity of the clinical picture. Some vasculitis affects only the skin, while others affect vital organs.
Left untreated, vasculitis can result in serious complications. Intestinal and pulmonary bleeding, thrombosis, renal failure, liver failure, heart attack - this is not a complete list of the dangerous consequences of the disease. Vasculitis can lead the patient to disability and even death.
1 Consultation with a rheumatologist
2 Consultation with a rheumatologist
3 Consultation with a rheumatologist
What is vasculitis?
Vasculitis is a group of diseases characterized by the development of inflammation of the walls of blood vessels. This inflammation begins due to an impaired immune response. The cause may be a past infection or allergy. Inflammation can affect small, medium, and large vessels. Because of it, blood circulation and blood supply to individual organs are disrupted, which can cause complications. Without treatment of vasculitis, necrosis of the vessel walls (death of their tissue), bleeding, and ischemia (impaired blood flow) begin. Both children and adults can get vasculitis. The disease can be primary (when inflammation of the walls of blood vessels is the only manifestation without an apparent cause) or secondary. With secondary vasculitis, the walls of blood vessels become inflamed due to other diseases (infectious, oncological, rheumatic).
TREATMENT FOR VASCULITIS IS AVAILABLE AT BRANCHES:
Treatment of vasculitis in the Primorsky region
Address: St. Petersburg , Primorsky district, st. Repisheva, 13
Treatment of vasculitis in the Petrograd region
Address: St. Petersburg , Petrogradsky district, st. Lenina, 5
The disease is usually accompanied by complications. Intestinal bleeding may occur from the gastrointestinal tract. Vasculitis can also cause liver damage. In the cardiovascular system, disorders such as cardiomyopathy and disruption of the heart valves can form. The most dangerous consequence of vasculitis is stroke. In the excretory system, a possible complication is glomerulonephritis.
Pathogenesis of vasculitis
Vasculitis develops due to a failure of immune mechanisms, but the exact causes of the disease have not been identified. The main hypothesis assumes that the nature of the disease is multi-etiological, associated with many factors. These include:
- acute or chronic bacterial or viral infections;
- allergy. A severe allergic reaction to drug components or food can cause immune failure;
- complication of vaccination. If after vaccination the immune response is impaired, vasculitis may occur. Such complications are very rare;
- severe or prolonged effects of stress, hypothermia or overheating, injuries.
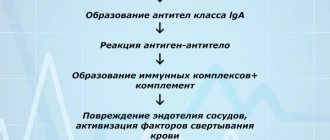
Under the influence of these factors, the production of pathogenic immune complexes begins. Normally, they attack the pathogen, but due to an immune failure, the attack is directed at the body’s cells. Immune complexes attach to the walls of blood vessels, damage them and provoke inflammation.
Figure 1. The difference between a healthy vessel and one affected by vasculitis. Source: sl.smithhealthcentre.com
General overview
Vasculitis can affect any of the body's blood vessels. These include arteries, veins and capillaries. Arteries carry blood from the heart to the organs of your body. Veins move blood from your organs and limbs back to your heart. Capillaries connect the small arteries and veins in your body.
When a blood vessel becomes inflamed, it narrows or becomes blocked, restricting or preventing the flow of blood to other vessels. In the process, the blood vessels stretch and weaken, creating bulges that cannot be seen with the naked eye on the skin. These bulges are called an aneurysm.
Classification
Vasculitis is a large group of diseases, and two classifications are used for them. The first is by etiology - it takes into account the reasons for which the disease appears. The second is by localization, taking into account which vessels are affected.
By etiology
This classification takes into account the causes of vasculitis:
- primary. Inflammation of the walls of blood vessels is not associated with other diseases, is not their manifestation and develops as an independent disease. The exact causes of primary vasculitis have not been established, but it is known that hereditary predisposition plays an important role;
- secondary. The walls of blood vessels become inflamed due to other diseases, inflammation is one of their manifestations.
There are several types of secondary vasculitis based on the underlying disease or condition that caused inflammation of the vessel walls:
- hepatitis B and C viruses;
- syphilis;
- oncological diseases;
- reaction to taking medications.
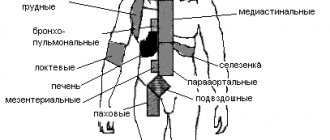
By localization
Division by localization takes into account which vessels are affected by vasculitis and where they are located. This determines the clinical picture, treatment approaches, prognosis and possible complications. The walls of small, medium and large blood vessels can become inflamed; inflammation can affect blood vessels of different sizes or vessels of individual organs.
Vasculitis of large blood vessels
When the walls of large blood vessels become inflamed, there are several common symptoms. These are large deviations from the norm when blood pressure changes and anomalies in the propagation of pulse waves. With each such wave after the heart contracts, the pressure in the arteries increases. If the wave is asymmetrical or absent on the arms or legs, this may be a sign of vasculitis. The disease is also indicated by the development of ischemia (decreased blood flow in a particular area), intermittent claudication (pain that occurs when walking and goes away after rest). Each type of vasculitis of large blood vessels has its own additional symptoms.
Giant cell arteritis. Inflammation affects the thoracic aorta, as well as the large arteries running from it to the neck, and the extracranial section of the carotid artery. Polymyalgia rheumatica is often the cause of giant cell arteritis. Symptoms include: headaches, blurred vision, fever, weight loss, fatigue, and general malaise.
Takayasu arteritis. Inflammation of the walls of the aorta and its branches, the walls of the pulmonary arteries, most often develops in young women. The first signs of the disease are weakness, spastic pain in the limbs, periodic visual disturbances, hypertension, differences in pulse or blood pressure values on different legs or arms or on an arm and leg on the same side.
Vasculitis of medium-sized vessels
The general manifestation is symptoms of infarction of the tissues of the affected organs: their necrosis occurs due to insufficient blood supply. On the skin this is manifested by the formation of nodules, ulcers, and livedo reticularis (discoloration). With a muscle tissue infarction, severe pain appears. It is possible to develop multiple neuropathy (damage to several nerves), kidney damage (increased pressure in the renal arteries), and mesenteric ischemia, which disrupts blood flow in the intestinal vessels. The exact symptoms depend on where exactly the affected vessels are located.
Cutaneous vasculitis. It affects the vessels of the subcutaneous tissue, which is why ulcers, purpura (hemorrhages in or under the skin, look like scatterings of small red dots), petechiae (bright red rash) appear on the skin.
Polyarteritis nodosa. With this disease, the walls of the muscle arteries become inflamed, causing secondary tissue ischemia to develop. With nodular arteritis, damage to the skin, kidneys, peripheral nerves, gastrointestinal tract, and any other organs is possible. Lung damage is not typical. First, general symptoms appear: fatigue, fever. Other manifestations depend on which organ is affected.
Vasculitis of small vessels
When the walls of small vessels become inflamed, symptoms of tissue infarction develop in the affected area. Often these manifestations are similar to the symptoms of vasculitis of medium vessels.
Cryoglobulinemic vasculitis. It is systemic and affects mainly small vessels. Blood serum analysis reveals cryoglobulins. Symptoms are varied and are determined by the location of the inflammation. Damage to the kidneys and peripheral nervous system often develops, and vascular purpura appears. General manifestations are weakness, slight increase in temperature, fatigue. In 90% of cases, purpura appears, most often it forms on the skin of the legs. When the kidneys are damaged, peripheral edema and increased pressure in the renal artery develop. It is also possible to experience muscle and joint pain and enlarged lymph nodes.
Wegener's granulomatosis. The lesion can affect any organs, but most often it is the respiratory organs or kidneys. If the respiratory organs are affected, the first symptoms are cough and runny nose, after which swelling develops, increased pressure, and symptoms of damage to several organs at once appear.
Hemorrhagic vasculitis. More often children get it. There are four forms of the disease: cutaneous (cutaneous-articular), abdominal (with damage to the digestive organs), renal, mixed. Accordingly, characteristic symptoms are identified, including palpable purpura, abdominal or joint pain, renal syndrome, vomiting, and nausea.
Microscopic polyangiitis. A rare disease that most often affects the kidneys. In about a third of cases, additional purpura appears on the skin. Possible damage to the respiratory system with the rapid development of shortness of breath, hemoptysis, and anemia. If alveolar bleeding develops against this background, the patient needs emergency help. Abdominal pain, vomiting and nausea, and damage to the nervous system are also possible.
Vasculitides that can affect blood vessels of varying sizes
Behçet's disease. Inflammation develops on the walls of small or medium-sized vessels. Symptoms depend on location. The disease can affect the lungs, kidneys, stomach, and brain. A peculiarity is the frequent appearance of ulcers on the mucous membranes of the mouth, in the genital area, and other mucous membranes.
Cogan's syndrome. A rare disease in which blood vessels of different sizes become inflamed. The disease is often accompanied by fever, joint pain, neurological disorders, decreased vision, hearing loss (may be irreversible).
Systemic vasculitis
This group includes vasculitis associated with systemic diseases:
- systemic lupus erythematosus. The immune system begins to produce antibodies that damage healthy cells. Because of this, the walls of blood vessels become inflamed and lupus vasculitis develops;
- rheumatoid arthritis. This is a systemic inflammatory disease affecting small joints. May be accompanied by rheumatoid vasculitis;
- sarcoidosis The disease is accompanied by the formation of granulomas (nodules) in inflamed tissues. Foci of inflammation in sarcoidosis form in the lymph nodes, lungs, liver, spleen, skin, and bones. Sarcoidosis may be accompanied by sarcoid vasculitis.
Vasculitis of individual organs
Inflammation of blood vessels can affect only one, separate organ. Such diseases include:
- cutaneous vasculitis. Affects small and medium-sized vessels in the skin and subcutaneous tissue, manifested by the formation of ulcers, purpura, petechiae;
- cutaneous leukocytclastic angiitis. Inflammation of blood vessels in the skin is isolated and is not accompanied by systemic vasculitis or other associated conditions;
- primary angiitis of the central nervous system. It affects the vessels of the spinal cord, brain, and pia mater. There are no signs of systemic inflammation;
- isolated aortitis. A form of vasculitis with limited localization of inflammation of the vessel walls.
Systemic vasculitis: modern standards of diagnosis and treatment
Most systemic vasculitis belongs to the ICD-XIII group (systemic connective tissue lesions) and is classified into subgroups M30 and M31. Henoch-Schönlein purpura has the code D69.0, Behcet's disease has the code M35.2, essential cryoglobulinemia has the code D89.1, and thromboangiitis obliterans (Buerger's disease) has the code I73.1. Epidemiology The prevalence of systemic vasculitis ranges from 0.4 to 14 or more cases per 100 thousand population. Systemic vasculitis is a relatively rare disease, but in recent years there has been a tendency to increase its prevalence [1,2,3]. Systemic vasculitis is more common in men than in women and can develop at any age, but mainly in the 4th–5th decades of life, with the exception of hemorrhagic vasculitis and Kawasaki disease, which are often characterized by a predominance of patients in childhood and adolescence. The peak incidence often occurs in winter and spring. Prevention • The etiology of most primary systemic vasculitis is unknown, and therefore primary prevention of these diseases is not carried out. • Some forms of systemic vasculitis (and in individual patients) can be clearly associated with certain causative (or “trigger”) factors, such as hepatitis B virus (classical polyarteritis nodosa), hepatitis C virus (essential cryoglobulinemic vasculitis). In these cases, preventive measures could potentially be aimed at preventing infection of certain risk groups (vaccination against the hepatitis B virus). Classification Depending on the caliber of the affected vessels, the following main forms of systemic vasculitis are distinguished [4]: Damage to large-caliber vessels • Giant cell (temporal) arteritis: granulomatous inflammation of the aorta and its large branches with damage to the extracranial branches of the carotid artery, mainly the temporal artery; usually develops in patients over 50 years of age and is often combined with polymyalgia rheumatica. • Takayasu arteritis: granulomatous inflammation of the aorta and its main branches, usually beginning before the age of 50 years. Damage to medium-sized vessels • Polyarteritis nodosa: necrotizing inflammation of medium and small arteries without glomerulonephritis or vasculitis of arterioles, capillaries and venules. • Kawasaki disease: arteritis, usually found in children, affecting large, medium and small arteries (mainly coronary, sometimes veins) and often combined with mucocutaneous lymphonodular syndrome. Small vessel involvement • Wegener's granulomatosis: granulomatous inflammation involving the respiratory tract and necrotizing vasculitis affecting small and medium-sized vessels (capillaries, venules, arterioles and arteries), with the development of necrotizing glomerulonephritis. • Churg-Strauss syndrome: granulomatous inflammation involving the respiratory tract associated with asthma and eosinophilia, and necrotizing vasculitis affecting small and medium-sized vessels. • Microscopic polyangiitis (polyarteritis): necrotizing vasculitis with a small amount or absence of immune deposits, affecting mainly small vessels (capillaries, venules or arterioles), rarely small and medium-sized arteries, the clinical picture of which is dominated by the phenomena of necrotizing glomerulonephritis and pulmonary capillaritis. • Henoch-Schönlein purpura: vasculitis with predominant IgA deposits, affecting small vessels (capillaries, venules, arterioles), which typically involves the skin, intestines and glomeruli of the kidneys, often combined with arthralgia or arthritis. • Essential cryoglobulinemic vasculitis: vasculitis with cryoglobulin-immune deposits, affecting small vessels (capillaries, venules and arterioles) mainly of the skin and glomeruli of the kidneys and associated with the presence of cryoglobulins in the blood serum. • Cutaneous leukocytoclastic vasculitis: isolated cutaneous leukocytoclastic angiitis without systemic vasculitis or glomerulonephritis. Diagnosis The diagnosis of the disease is based on a detailed clinical examination of the patient and the exclusion of other diseases, and is necessarily confirmed by tissue biopsy data or the results of instrumental and laboratory examination methods. In each case, the disease should be classified according to the classification criteria of the American College of Rheumatology (1990), which, however, are intended for epidemiological studies and not for the diagnosis of systemic vasculitis, especially in the early stages of the disease. Main clinical manifestations • General (constitutional) symptoms: all forms of vasculitis. • Non-destructive oligoarthritis: polyarteritis nodosa, Wegener's granulomatosis, Churg-Strauss syndrome, Henoch-Schönlein purpura. • Skin lesions: – livedo reticularis, digital infarcts, ulcers, nodules: polyarteritis nodosa, Churg-Strauss syndrome, Wegener’s granulomatosis; – palpable purpura: any form of vasculitis, with the exception of giant cell arteritis and Takayasu arteritis. • Multiple mononeuritis: polyarteritis nodosa, cryoglobulinemic vasculitis, Wegener's granulomatosis, Churg-Strauss syndrome. • Kidney damage: – ischemic damage: polyarteritis nodosa, Takayasu arteritis; – glomerulonephritis: microscopic polyangiitis, Wegener’s granulomatosis, cryoglobulinemic vasculitis, Churg-Strauss syndrome, Henoch-Schönlein purpura. • Damage to the ENT organs: Wegener's granulomatosis, less commonly microscopic polyangiitis and Churg-Strauss syndrome. • Lung damage: Wegener's granulomatosis, microscopic polyarteritis, Churg-Strauss syndrome. • Bronchial asthma or allergic rhinitis: Churg-Strauss syndrome. Assessment of activity • When assessing the activity of vasculitis, only signs caused by vasculitis at the time of examination, as well as those that appeared or progressed during the last month before examination of the patient are taken into account [5]. • Depending on the activity, the following phases of the disease are distinguished: – complete remission – absence of signs of activity (total score 0–1 point) and the need for therapy with a normal level of CRP; – partial remission – a decrease in the total score during treatment by 50% of the original; – inactive phase – remission, which does not require maintenance therapy; – “major” exacerbation – involvement of vital organs or systems (lungs, kidneys, central nervous system, cardiovascular system) in the inflammatory process. In this case, there is an increase in the total score by 6 or more points and the prescription of adequate therapy (glucocorticoids and/or cytostatics, intravenous immunoglobulin, plasmapheresis) is required; – “minor” exacerbation – return of the disease with an increase in the total score from 0–1 to 5 points. Recommended inpatient examination Clinical • Assessment of subjective symptoms Laboratory • Complete blood count • Creatinine • Liver enzymes • Creatine phosphokinase: if myopathy is suspected • Complete urinalysis • Bacteriological blood test: exclude infection • Serological tests for syphilis: exclude syphilitic infection • Serological examination: – ANF, RF – exclusion of systemic rheumatic disease; – ANCA – to confirm diagnoses of Wegener’s granulomatosis, microscopic polyangiitis, Churg-Strauss syndrome; – cryoglobulins – to confirm the diagnosis of cryoglobulinemic vasculitis; – APL – exclusion of primary antiphospholipid syndrome; – aBMK – exclusion of Goodpasture syndrome. • Markers of hepatitis B and C virus, HIV (if polyarteritis nodosa and cryoglobulinemic vasculitis are suspected, respectively); cytomegalovirus, Epstein-Barr virus, parvovirus B19 - as needed. Morphological examination An obligatory component of diagnosis (diagnostic criteria) for polyarteritis nodosa, Wegener's granulomatosis, microscopic polyarteritis, Churg-Strauss syndrome, giant cell arteritis. Instrumental examination Angiography: – polyarteritis nodosa – if it is impossible to perform a biopsy or if nonspecific results are obtained; indicated before liver or kidney biopsy to identify microaneurysms that may lead to bleeding during biopsy; – Takayasu arteritis, thromboangiitis obliterans: is important both for confirming the diagnosis and for assessing the dynamics and spread of the inflammatory process. Doppler ultrasound: vascular damage in Takayasu arteritis and thromboangiitis obliterans. R-graphy of the lungs: diagnosis of lung lesions in Wegener's granulomatosis, microscopic polyangiitis, Churg-Strauss syndrome Computer and magnetic resonance imaging: determination of the localization of the process in Wegener's granulomatosis, microscopic polyangiitis, giant cell arteritis, Takayasu arteritis. Differential diagnosis • Clinical signs observed in systemic vasculitis occur in systemic connective tissue diseases (including antiphospholipid syndrome), infections (infective endocarditis, syphilis, other systemic infections) and tumors (atrial myxoma, lymphoproliferative tumors, etc.), severe atherosclerotic lesions vessels. • The need for timely diagnosis of the disease is dictated by the need for early (before the development of irreversible damage to vital organs) administration of aggressive therapy. • Systemic vasculitis should be excluded in all patients with fever, weight loss and signs of multiple organ damage (vascular purpura, multiple mononeuritis, urinary syndrome). Indications for consultation with a rheumatologist: • The presence of any clinical manifestations that suggest systemic vasculitis. Indications for consultation with other specialists: Management of patients with systemic vasculitis requires a multidisciplinary approach. • Dermatologist: vasculitis with skin lesions • Neurologist: when identifying neurological symptoms • Ophthalmologist: for eye damage in patients with Behçet's syndrome, Wegener's granulomatosis, Takayasu's arteritis, giant cell arteritis • Otolaryngologist: for damage to the ENT organs in Wegener's granulomatosis • Nephrologist: kidney damage for systemic necrotizing vasculitis • Pulmonologist: lung damage with Wegener's granulomatosis, microscopic polyarteritis, Churg-Strauss syndrome • Infectious disease specialist and phthisiatrician: carriage of hepatitis B and C viruses, development of opportunistic infections, tuberculosis • Vascular surgeon: vascular damage with Takayasu arteritis • Surgeon: development abdominal pain syndrome with Takayasu arteritis, polyarteritis nodosa, hemorrhagic vasculitis Indications for hospitalization in the rheumatology department: • Clarification of the diagnosis and assessment of the prognosis • Selection of therapy • Exacerbation of the disease • Development of complications Treatment Treatment is always prescribed individually depending on the clinical manifestations of the disease and the type of vasculitis. Goals of therapy • Achieving clinical and laboratory remission • Reducing the risk of exacerbations • Preventing irreversible damage to vital organs • Reducing the risk of developing side effects of drug therapy • Increasing life expectancy. Drug therapy The main groups of drugs used for systemic vasculitis include glucocorticoids and cytostatics (cyclophosphamide, methotrexate, azathioprine) [6,7,8,9,10,11]. For a number of forms of systemic vasculitis, extracorporeal methods of blood purification (plasmapheresis) and the administration of intravenous immunoglobulin are used [8,9,10]. Glucocorticoids • The main treatment for giant cell arteritis and Takayasu arteritis, as well as certain systemic necrotizing vasculitis in the absence of signs of progression, for example, Churg-Strauss syndrome and cryoglobulinemic vasculitis; are used to treat severe forms of hemorrhagic vasculitis with damage to the gastrointestinal tract and kidneys. • Due to the high rate (96%) of disease progression, glucocorticoid monotherapy is not used for the treatment of Wegener's granulomatosis, microscopic polyangiitis and polyarteritis nodosa. • The rapid effect of glucocorticoids can be considered a diagnostic sign of giant cell arteritis and polymyalgia rheumatica. Tactics for prescribing glucocorticoids: • At the onset of the disease, glucocorticoids are usually prescribed in several doses at a dose of 1 mg/kg/day, and then (after 7–10 days) with positive dynamics of clinical and laboratory parameters, they switch to a single dose in the morning. • The duration of suppressive therapy with glucocorticoids is at least 3–4 weeks. • After achieving the effect, the dose of drugs is gradually reduced by 5 mg every 2 weeks. to maintenance (0.15–0.2 mg/kg/day), which is prescribed from 1 year to 3–5 years. • Pulse therapy: – used in patients refractory to standard therapy; – used to induce remission of vasculitis and to suppress its exacerbations (escalation therapy). Cyclophosphamide Drug of choice for: • systemic necrotizing vasculitis (Wegener's granulomatosis, microscopic polyarteritis), polyarteritis nodosa (in the absence of markers of hepatitis B virus replication); • severe forms of hemorrhagic vasculitis and Churg-Strauss syndrome, in which severe, rapidly progressive vascular and renal damage is observed, even despite a good initial clinical response to glucocorticoids. Treatment tactics: • 1–2 mg/kg/day. (orally) for 10–14 days, followed by a decrease depending on the level of leukocytes in the peripheral blood. With very rapid progression of vasculitis, cyclophosphamide is prescribed at a dose of 4 mg/kg/day. per os for 3 days, then 2 mg/kg/day. for 7 days or in the form of pulse therapy (10–15 mg/kg/day) • The total duration of treatment is at least 12 months. after achieving complete remission. Then the dose of the drug is gradually reduced over 2–3 months. 25–50 mg. • Dose selection: the concentration of leukocytes should not be lower than 3000–3500/mm3, and neutrophils – 1000–1500/mm3. At the beginning of treatment, it is advisable to monitor the concentration of leukocytes every other day, and after stabilizing their number - at least once every 2 weeks. • There is evidence of the effectiveness of intermittent therapy with high doses of cyclophosphamide (in combination with glucorticoids) and a decrease in the number of side effects of this drug (500–700 mg/m2 monthly for 6–12 months). However, in Wegener's granulomatosis, this regimen is associated with a high rate of exacerbations [12]. • In patients with renal impairment (serum creatinine > 500 mmol/L), the dose of cyclophosphamide should be reduced by 25–50%. • Treatment with cyclophosphamide should be continued for at least 1 year after remission has been achieved. • Treatment with cyclophosphamide is associated with an increased incidence of side effects (primarily pulmonary infectious complications and bladder cancer in Wegener's granulomatosis), which determine high morbidity and mortality. Azathioprine • Used to maintain remission [13] in necrotizing vasculitis: less likely to cause side effects than cyclophosphamide [14]. • optimal dose – 1–3 mg/kg/day; maintenance dose – 50 mg/day. Methotrexate • Drug dose – 12.5–17.5 mg per week. • In combination with glucocorticoids, it is used to treat Wegener's granulomatosis without rapidly progressive nephritis and severe lung damage, usually in cases of intolerance to cyclophosphamide or to maintain remission of the disease [15,16,17]. • For Takayasu arteritis, the use of methotrexate (17.5 mg/week) in combination with small doses of glucocorticoids allows to achieve remission in 81% of patients and prevent disease progression in 50% of patients, quickly reduce the dose of glucocorticoids and maintain longer remission; low doses of methotrexate (7.5 mg/week) are ineffective [18]. Intravenous immunoglobulin • There are observations of a positive clinical effect when using this drug at a dose of 2 mg/kg (monthly for 6 months) in combination with plasmapheresis for Churg-Strauss syndrome [19]. • Its effectiveness has not been proven in other systemic necrotizing vasculitis. Plasmapheresis • Main indication: as part of combination therapy for acute, progressive disease, manifested by rapidly progressive nephritis (creatinine level more than 500 µmol/l) and severe vasculitis [8,9,10,20]. • In combination with glucocorticoids, they are used for the treatment of essential cryoglobulinemic vasculitis and polyarteritis nodosa associated with the hepatitis B virus. • The use of plasmapheresis in patients with polyarteritis nodosa and Churg-Strauss syndrome, who have unfavorable prognosis factors, does not increase the five-year survival rate of patients compared with standard glucocorticoid therapy and cytostatics [21]; the use of plasmapheresis for the treatment of glomerulonephritis in Churg-Strauss syndrome has no advantages compared to standard therapy for this disease. Combined therapy of systemic necrotizing vasculitis is currently in most cases with systemic necrotic vasculitis (granulomatosis of the vegenera, microscopic polyangita, nodular polyiaritis, Charg -Strass syndrome) is used combined therapy with glucocorticoids and cytostatics [6,8,9,10]. • induction therapy (4-6 months): cyclophosphamide 2 mg/kg/day. Within 1 month. (maximum 150 mg/day); Reduce the dose by 25 mg, if the patient is> 60 years (the number of leukocytes should be> 4.0 × 109/l) in combination with a prenisolone of 1 mg/kg/day. (maximum 80 mg/day); Reduce to 10 mg/day every week. within 6 months. • Supporting therapy: Azatioprine 2 mg/kg/day. or cyclophosphamide 1 mg/kg/day. In combination with a prednisone 5-10 mg/day. • escalation therapy (active severe disease with an increase in creatinine> 500 mmol/l or with pulmonary hemorrhages): 7–10 plasmapheresis procedures within 14 days (plasma removal in the amount of 60 ml/kg with its replacement equal volume of 4.5–5% –In human albumin) or pulse - therapy with methylprednisolone (15 mg/kg/day), dexamethasone (2 mg/kg) for 3 days; If the age of patients <60 years, it is possible to prescribe cyclophosphamide at a dose of 2.5 mg/kg/day. Moopherines of mycophenolat • at a dose of 2 g/day. Used to maintain remission in patients with granulomatosis of the vegener [22,23]. Cyclosporin a • in the initial dose of 5 mg/kg/day. followed by a decrease to 2 mg/kg/day. More effective than colchicine regarding the suppression of progression of uveitis in the disease of Bekhceta [24], and at a dose of 2.5 mg/kg/day. More effective than pulse therapy with cyclophosphamide [25]. • Sometimes it is used to maintain remission in granulomatosis of the vegener with the ineffectiveness of other types of therapy, but its use is limited due to the potential nephrotoxicity of the drug. Leflunomide • There are separate observations about a positive clinical effect when using this drug at a dose of 40 mg/day. In combination with 10 mg/day. prenisolone to maintain remission with granulomatosis of the vegener [26]. Sulfametoxazole/trimetrome • There are reports about the use of sulfametoxazole/trimetrim (160/800 mg 2 times a day) to maintain remission in patients with granulomatosis of the vegener [27], primarily with disabilities (lesion of the ENT -organ) and in the early phase of the disease [ 28]; In a dose (160/800 mg 3 times a week) it is used to prevent infectious complications caused by P.Carinii, against the background of immunosuppressive therapy of methotrexate during the period of maintenance of remission of the disease [29]. • The use of the drug as monotherapy or in combination with prednisone is ineffective to maintain remission with a generalized form of granulomatosis of the vegener. Kolchitsin • In case of illness of behchet, the prescription of colchicin (0.5–1.5 mg/day) reduces the frequency and severity of the exacerbations of the disease and its progression [30]. Antiviral drugs • In the presence of markers of the hepatitis B virus, the prescription of interferon preparations [31] (real -denser, recombinant genetically engineer interferon -a), lamivudina [32] at a dose of 100 mg/day are shown. (lasting up to 6 months) in combination with glucocorticoids and plasmapheresis. • Infection of hepatitis C virus (HCV) for cryoglobulimic vasculitis: Interferon -A, ribavirin preparations in combination with glucocorticoids, cytostatics and plasmapheresis (depending on the severity of the condition) [10, 32]. Pentoxifillin: used to treat systemic vasculitis, especially with vasospastic and ischemic syndromes, skin and kidneys. Surgical treatment • It is indicated in the presence of critical, clinically significant (regional ischemia) stenosis or occlusion of the main arteries for ateritis by Tusas [11], obliterating thrombangiate [33], the development of irreversible (peripheral gangrene) changes in tissue changes; Sublot stenosis for granulomatosis of the vegener (mechanical dilatation of the trachea in combination with the local administration of glucocorticoids) [34]. The prognosis of nodule poly arthol: five -year survival in the background of combined therapy with glucocorticoids and cytostatics is up to 60–80%, the largest death of death is recorded in the first year from the onset of the disease. In most cases, the direct cause of death is cardiovascular disasters. Adverse prognostic factors include: the onset of the disease over the age of more than 50 years, damage to the kidneys, the gastrointestinal tract, central nervous system and the development of cardiomyopathy [35]. Microscopic poly arteritis: the prognosis largely depends on the degree of kidney damage; The five -year survival of patients is 65%, in addition, the cause of death is massive pulmonary bleeding, infectious complications associated with therapy. Vegener's granulomatosis: 5 -year survival is more than 75%; The most common causes of deaths are intercurrent infections, respiratory and renal failure, cardiovascular disasters, malignant neoplasms (bladder cancer). Charga -Strass syndrome: the prognosis of the disease depends on the degree of respiratory failure, the generalization of vasculitis (polyneumnia, glomerulonephritis); 5 -year survival is up to 80%. Purpura Shenlein -Genoch: Despite the fairly frequent recurrence of the disease (in 40% of cases), in general, the prognosis for hemorrhagic vasculitis is favorable. Five -year survival of patients is 95%. During the first two years of disease, complete recovery is observed in 93.9% of children and 89.2% of adults [36]. The main factor that determines the unfavorable prognosis of the disease is a persistent kidney damage. Among all the reasons leading to chronic hemodialysis in pediatric practice, glomerulonephritis with hemorrhagic vasculitis accounts for 3-15% [36]. Gigantic cell arteritis: in general, the forecast for the life of patients is favorable. 5 -year survival of almost 100% [37]. However, there is a serious danger of developing various complications of the disease, first of all, damage to the arteries of the eyes, leading to partial or complete loss of vision. The arteritis by Tsuas: 5-10-15 - survival reaches 80–90%. The most common cause of death is a stroke (50%) and myocardial infarction (about 25%), less often - the rupture of aorta aneurysm (5%). In case of damage to the coronary arteries in the first two years from the moment the symptoms of cardiac pathology occurred, mortality reaches 56%. An unfavorable prognosis is observed in patients, the course of the disease in which is complicated by retinopathy, arterial hypertension, aortic deficiency and aortic aneurysm [38]. In patients with two or more of these syndromes, 10 -year survival from the moment of diagnosis is 58.6%, and most of the fatal outcome falls in the first 5 years of the disease. Crylobulinemic vasculitis: the most common cause of death is the damage to the liver and kidneys, diseases of the cardiovascular system and lymphopoliferative diseases. Literature 1. Koldingsnes W., Nossent H. Epidemiology of Wegener's Granulomatossis in North Norway. Arth.rheum. 2000; 43: 2481–2487. 2. Watts Ra, Lane SE, Bentham G., Scott DGI Epidemiology of Systemic Vasculites: A Ten - Year Study in the United. Arth.rheum. 2000; 43: 414–419. 3. Mahr A., Guillevin L., Poissonnet M., Ayme S. Prevalemces of Polyarterity Nodosa, Microscopic Poliangiitis, Wegener's Granulomatosis and Churg - Strauss Syndrome a French Urban Po Palation in 2000: A Capture - Recapture Estimate. Arth.rheum. 2004; 51: 92–99. 4. Jennette JC, Falk RJ, Andrassy K., et al. Nomenclature of Systemic Vasculitides: Proposed of an International Conference. Arthritis Rheum, 1994; 37: 187–192. 5. Luqmani Ra, Bacon Pa, Moots Rj. et al. Birmingham Vasculites Activity Score (BVAS) In Systemic Necrotising Vasculites.qjmed., 1994; 87: 671–678. 6. Jane D. Evidence - BASED TREATMENT OF SYSTEMIC VASCULITIS. Rheumatology, 2000; 39: 585–595. 7. Ling SM. Polymyalgia Rheumatica and Giant Cell Arteritis. Clinical Guidance from ACP. 2003. 8. Thomas - golbanov C., Sridhan S. Novel Therapies in Vasculites. Expert. Opin. Investig. Drugs. 2001; 10: 1279–1289. 9. Savage Co., Harper L., Ady D. Primary Systemic vasculitis. Lancet, 1997; 349: 553–558. 10. Gross Wl New Concept in Treatment Protocols for Sever Systemic Vasculites. Curr Opin Rheumatol, 1999; 11: 41–46. 11. Sabbadini Mg, Bozzolo E., Baldissera E. Bellone M. Takayasu's Arterites: Therapeutic Strategies. J.Nephrol. 2001; 14: 525–531. 12. Groot KD., ADU D., Savage Co the Value of Pulse Cyclophosphamide in Anca - Sasociated Vasculitis: Meta - Angysis and Critical Review. Nephrol Dial Transplant 2001; 16: 2018–2027. 13. Westman KW, Bygren PG, Olsson H. et al. Relapse Rate, Renal Survival, and Cancer Morbidity in Patience with Wegener's Granulomatosis Or Microscopic Polyangiitis with Renal InvolVeum. J Am Soc Nephrol 1998; 9: 842–852. 14. Jayne Dr, Rasmussen N., Andrassy K. et al. A RANDOMIZED TRIAL of Maintenance Therapy for Vasculites Associated with Antineutrophil Cytoplasmic Autoantibodies New.ingl. J.Med. 2003; 349: 36–44 15. Stone JH, Tun W., Hellman DB Threating of Non - Life Threatening Wegener's Granulomatossis with Methototrexate and Daily Prednisolone as the Initial Therapy of Choice. J.RheumATOL. 1999; 26: 1134–1139. 16. SNELLER MC, Hoffman GS, Talar --williams C. et al. Analysis of 42 Wegener's Granulomatossis Patients Treated with Methotrexate and Prednisone. Arthr.rheum. 1995; 38: 608–613. 17. Langford Ca, Talar --williams C., Barron KS, Sneller MC Use of a Cyclophosphamide - Induction Mithotrexate Regimen for Wegener's Granulomatoissis: Extendence: Extendance D Follow - Up and Rate of Relapse. Am. J. Med. 2003; 114: 463–469. 18. Hoffman GS, Leavitt Ry, Kerr GS et al. Treatment of Glucocorticoid - ReSistant or Relapsing Takayasu Arterity with Methotrexate // Arthr.rheum. - 1994. - Vol. 37. - P.578 - 582. 19. Danieli Mg, Cappelli M., Malcangi G. et al. Long Term Effectivence of Intravenous Immunoglobulin in Churg - Strauss Syndrome. Ann.rheum.dis. 2004; 63: 1649–1654. 20. Cole E., Cattran D., Magil A. et al. A Prospective Randomized Trial of Plasma Exchange as Additive Therapy in Idiopathic Crescentic GlomerulonePhritis. Am J Kidney Dis. 1992; 20: 261–268. 21. Guillevin L., Fain O., Lhote F. et al. Lack of Superiority of Steeroids Plus Plasma Exchange to Steroids Alone in the Treatment of Polyarteritis and Churg - Strauss Syndrome. A proospective, Randomized Trial in 76 Patience // Arthr.rheum. - 1992. - Vol. 35. - P.208 - 215. 22. Nowack R., Gobel U., Klooker P. et al. Mycophenolate Mofetil for Maintenance Therapy of Wegener's Granulomatosis and Microscopic Polyangiitis: A Pilot Study in 11 PATIENTS WITH RENAL INVOLVEMENT. J.AM.SOC. Nephrol. 1999; 10: 1965–1971. 23. Langford Ca, Talar --williams C., Sneller Mc Mycophenolate Mofetil for Remission Maintenance in Therapy of Wegener's Granulomatossis. Athr.rheum. 2004; 51: 278–283. 24. Diaz --llopis M., Cervera M., Menezo Jl Cyclosporin a Treatment of Behcet`s Disease: A Long - Term Study // Curr.eye Res. - 1990. - Vol.9 (SUPPL.). - P.17 - 23. 25. Ozyazgan Y., Yurdakul S., Yazici H. et al. Low Dose Cyclosporin a Versus Pulsed Cyclophosphamide in Behcet's Syndrome: A Single Masked Trial. BR J OPHTHALMOL 1992; 76: 241–247. 26. Metzler C., Low - Friedrich I., Reinold - Keller E. et al. Leflunomide a New Promising Agent in Maintenance of Remission in Wagener's Granulomatosis. Clin.exp.immunol. 1998; 112: 56. 3 Dutch Co - Trimoxazole Wegener Study Group. N.engl.j. Med. 1996; 335: 16–20. 28. Reinhold - Keller E., de Groot K., Rudert H. et al. Response to trimethoprim/Sulfamethoxazole in Wegener's Granulomatossis Depends on the Phase of Disease. QJM 1996; 89: 15–23. 29. Chung JB, Armstrong K., Schwartz JS, Albert D. Cost - Effectivence of Prophylaxis AGainStis Carini Pneumonia in Patents with Wegner's Granulomatosis Undergo Immunosuppressive Therapy. Arthr. Rheum. 2000; 43: 1841–1847. 30. Masuda K., nakajima A., urayama A. et al. Double - Massked Trial of Cyclosporin Versus Colchicne and Long - Term Open Study of Cyclosporin in Behcet`s Disease.lancet. 1989; 1: 1093 - 1096. 31. Guillevin L., Cohen P. Management of Virus --induced Systemic vasculitides. Cur.rheumATOL.Rep. 2002; 4: 60–66. 32. Guillevin L., Mahr A., Cohen P. et al. Short -Term Corticosteroids then lamivudine and Plasma Exchanges to Treat Hepatis b Virus --rerteritis nodosa. Arthr.rheum. 2004; 51: 482–487. 33. TADA Y. Surgical Treatment of Intractable Vasculitis Syndromes with Special Reference to Buerger Disease, Takayasu Arteritis, and So - Called Abdominal Aortic aneurasm. Nippon.rinsho.1994; 52: 2191 - 2202. 34. Hoffman GS, Thomas - Golbanov CK, Chan J. et al. Treatment of Subglottic Stenosis, Due To Wegener's Granulomatosis, With Intraletional Corticosteroids and Dilation. J Rheumatol. 2003; 30: 1017–1025. 35. Guillevin L., Lhote F., Cohen P. et al. CorticoSteroids Plus Cyclophosphamide and Plasma Exchange Versus Corticosteroids Plus Cyclophosphamide Alone in the Treatment of Polyarteritis Nodosa and Churg - Strauss Syndrome iEnts with factors Predicting Poor Prognosis. Arthr.rheum. - 1995. - Vol.38. - P.1638 - 1645. 36. Blanco R., Martinez - Taboada VM, Rodriguez - Valverde V. et al. Henoch - Schonlein Purpura in Adulthood and Childhood. Two Different Expression of the Same Syndrome. Arthr.rheum. 1997; 40: 859 - 864. 37. Salvarani C., Crowson CS, O'Fallon WM et al. Reappraisal of the Epidemiology of Giant Cell Arterites in Olmsted Country, Minnesota, Over a Fifty - Year Period. Arth.rheum. 2004; 51: 264–268. 38. ISHIKAWA K., Maetani S. Long - Term Outcome for 120 Japanese Patients with Takayasu's Disease. Clinical and Statistical Analyses of Related Prognostic Factors // Circulation. - 1994. - Vol.90. - R.855 - 860.
Causes
Inflammation of the walls of blood vessels begins due to autoimmune disorders, in which antibodies are produced against the cells of one’s own body. The exact causes of primary vasculitis have not been established. Secondary vasculitis develops against the background of infectious or oncological diseases, as a rare complication of vaccination, after overheating or hypothermia, or sunburn.
Other possible causes include allergies to medications. More than 150 drugs have been identified that can provoke the disease. These include some antibiotics, analgesics, radiopaque agents, serums, vaccines, as well as iodine preparations, B vitamins and other drugs. Allergies, autoimmune failure and the development of vasculitis do not always occur after taking them. The risk of such complications is determined by the individual reaction to the components of the drug. Therefore, it is important that all medications are selected by a doctor. You do not need to choose your own antibiotics or antihistamines.
Symptoms of vasculitis
The manifestations of vasculitis are determined by the type of disease, location and size of the affected vessels. The most common symptoms that appear are:
- increased body temperature;
- weakness, malaise, fatigue;
- decreased appetite, nausea and vomiting;
- rapid weight loss;
- pain: headaches, muscles, joints;
- dizziness, loss of consciousness;
- pallor of the skin, the appearance of rashes on it (ulcers, purpura, petechiae);
- if there are cardiovascular diseases, they worsen;
- Possible decreased vision;
- change in skin sensitivity (from weak, almost absent to too strong);
- symptoms associated with organs whose functioning is impaired due to insufficient blood circulation (this may be decreased vision, symptoms of kidney failure, problems with the digestive system).
Figure 2. Skin rash due to vasculitis.
Source: CC0 Public Domain Symptoms of inflammation are the first to appear, regardless of the size of the affected vessels. Fever occurs, general malaise occurs, weight begins to decrease, joint pain appears, and sweating increases at night. If the walls of small and medium-sized vessels become inflamed, skin lesions appear almost immediately: rash (palpable purpura, urticaria, and others), the formation of ulcers, nodules, livedo reticularis.
Figure 3. Reticular erythema pattern typical of livedo reticularis in cutaneous vasculitis. Source: Springer Science/Business Media
Some of the symptoms of vasculitis can be life-threatening and require immediate treatment. These are alveolar hemorrhage, mesenteric ischemia, a sharp decrease in vision, glomerulonephritis (kidney damage).
The exact symptoms of vasculitis depend on its form:
- cutaneous - an itchy rash appears on the skin as a result of pinpoint hemorrhages. At first, its color is red, but then the rashes darken, disappear, and pigmented areas remain in their place. More often, such rashes form on the skin of the buttocks and legs;
- articular - manifested by swelling, impaired mobility of large joints, pain;
- abdominal - abdominal pain, nausea, vomiting, loss of appetite;
- renal - change in the color of urine and a decrease in its volume. The urine turns red or pink. Clinical analysis reveals protein levels indicating glomerulonephritis. Without treatment, kidney failure develops.
Vasculitis in children
Vasculitis rarely appears in children. Almost always this is either hemorrhagic vasculitis or Kawasaki syndrome.
Kawasaki syndrome. Yonsei medical journal / Open-i (Attribution-NonCommercial 3.0 Unported)
Kawasaki syndrome is dangerous due to damage to the lymph nodes, heart vessels, and respiratory mucosa. The disease develops in an acute form with the sequential appearance of the following symptoms:
- severe fever with a rapid increase in temperature to 38-41 degrees;
- the appearance of a rash, erythematous spots on the skin;
- damage to the mucous membranes of the eyes, upper respiratory tract, nose;
- redness and then thickening of the skin on the palms and soles of the feet;
- inflammation, enlargement of lymph nodes in the neck;
- redness of the tongue;
- dryness and flaking of the skin on the phalanges of the fingers and toes, around the nails.
Kawasaki syndrome is dangerous due to damage to the cardiovascular system and the risk of aneurysm formation, but with timely diagnosis and treatment, the prognosis is favorable.
Hemorrhagic vasculitis in children can occur in several forms, including cutaneous, abdominal, skin-articular, and renal. Symptoms for each form vary:
- skin - the appearance of rash, swelling;
- abdominal - abdominal pain, nausea and vomiting, loss of appetite, weight loss;
- renal - decrease in urine volume, change in its color, appearance of protein in the analysis;
- articular - the appearance of joint pain, limited mobility of large joints.
Vasculitis in adults
Vasculitis in adults develops as a result of disturbances in the functioning of the immune system. The main risk factors are severe infections, untimely or improper treatment of infectious diseases, taking medications without a doctor’s prescription, allergies to food or medications, and the use of certain medications.
Vasculitis occurs as a chronic, progressive disease, and in this case, its treatment requires complex and long-term therapy. The earlier the diagnosis is made and treatment started, the better the prognosis. In adults, inflammation of the walls of blood vessels can provoke life-threatening conditions, so it is important to consult a doctor promptly. Inflammation of the walls of blood vessels may be indicated by ongoing fever, symptoms associated with poor circulation, muscle, headaches, and joint pain.
Tests and diagnostics
Vasculitis can occur in several forms, and the symptoms for each of them will be different. Often they are “masked” as other diseases, and therefore a detailed diagnosis is needed. It starts with contacting a rheumatologist. He can refer you to a dermatologist, cardiologist, immunologist, nephrologist and other specialists.
Diagnosis begins with the following studies:
- clinical blood test. Allows you to identify inflammation, signs of allergies, immune reactions;
- general urine analysis. Evaluates the condition and function of the kidneys. With a high protein content, it indicates glomerulonephritis associated with kidney damage;
- coagulogram. Evaluates blood clotting. With vasculitis, it decreases, which increases the risk of hemorrhage.
Additionally, tests can be performed for antibodies to hepatitis B and C (often detected with vasculitis), a biopsy of the affected tissue, followed by histology (the study of cells). Some laboratory tests are used to determine the type of vasculitis, its etiology, and the degree of organ damage.
During diagnosis, an ECG is also prescribed to assess the condition of the heart, identify circulatory disorders, radiography, CT or MRI of affected organs or large blood vessels.
Diagnostics
It is necessary to try to diagnose vasculitis even in the presence of the very first signs. The disease is serious and dangerous and requires immediate treatment.
If you suspect an illness, you must perform a series of examinations and tests. Appointed:
- angiography;
- general blood and urine tests;
- ECHO-cardiography;
- blood biochemistry;
- Ultrasound of the heart, abdominal organs and kidneys;
- X-rays of light.
The problem is that it is very difficult to diagnose vasculitis in the early stages. But more striking signs of the disease and a reason to sound the alarm appear even when several organs are affected at once.
In severe and rapid progression of the disease, an additional biopsy is performed, followed by a detailed study of tissue samples.
Treatment
The approach to treating vasculitis is determined by the location of the affected vessels, the presence of concomitant diseases, the severity of the condition, and a number of other factors. Most often, complex therapy is used, which involves taking medications, physiotherapy, diet, and preventing exacerbations. In severe forms of the disease, if thrombosis of large arteries or stenosis of the great arteries develops, surgical treatment is indicated.
Drug treatment of vasculitis
Approaches to treating vasculitis vary in each case. The rheumatologist will prescribe medications to reduce the production of antibodies and reduce tissue sensitivity. In some cases, antibiotics are needed, in others, antiallergic drugs.
Photo: lucky7trader / freepik.com
The attending rheumatologist should draw up a drug treatment program. Additionally, he can attract other doctors of a more narrow specialization. You cannot try to cure the disease on your own. It is dangerous due to severe complications and requires systemic and complex therapy.
Medicines for vasculitis
Prescribed in order to achieve stable remission and reduce the risk of complications. With secondary vasculitis, therapy is aimed at treating the underlying disease that caused vascular inflammation.
The following drugs are used for treatment:
- glucocorticosteroids or steroid hormones. Prescribed in almost all cases, they have anti-inflammatory and immunosuppressive effects. Doses of drugs are selected individually, creating a dosage schedule. Typically the dosage is high at first and then gradually reduced;
- cytostatics. They suppress the activity of the immune system, which allows for the correction of autoimmune mechanisms. Cytostatics are used in combination with glucocorticosteroids for severe forms of vasculitis. The drugs are prescribed as part of pulse therapy. It involves taking medications in short courses to avoid side effects;
- antitumor drugs, in particular Rituximab. These are monoclonal antibodies that are produced by immune cells, have immunosuppressive properties and are used in the treatment of systemic vasculitis if the use of cytostatics is undesirable. They are not prescribed for hepatitis B virus, neutropenia, low IgC levels in the blood and a positive tuberculin test.
Immunosuppressants (suppress the activity of the immune system), normal human immunoglobulin (used for infectious complications, severe kidney damage, development of hemorrhagic alveolitis), antibacterial, non-steroidal anti-inflammatory drugs, anticoagulants (prevent the formation of blood clots in blood vessels), antiallergic drugs can also be prescribed.
Physiotherapeutic methods for treating vasculitis
To treat vasculitis, plasmapheresis is used, in which blood is taken, purified and returned to the bloodstream. The technique is used as part of combination therapy if the disease is severe or acute and progresses rapidly. Plasmapheresis is prescribed in courses for severe kidney damage, as well as in cases where the use of cytostatics is contraindicated.
Treatment with folk remedies
Folk remedies are ineffective in treating vasculitis, and their use can be dangerous. If the disease progresses rapidly or becomes severe, you should immediately consult a doctor. Attempts to be treated with traditional methods will lead to a loss of time and can provoke complications.
Valeria Korol – general practitioner, rheumatologist, Member of the Expert Council of MedPortal
“Who is admitted to the hospital for vasculitis?
— All patients with newly diagnosed signs of systemic vasculitis. Special indications for hospitalization of patients with an established diagnosis of SV:
- Rapidly progressive deterioration of kidney function
- The appearance of protein in the urine - more than 3 g/day
- Recurring abdominal pain
- Damage to the organ of vision
- Signs of central nervous system damage"
Prevention
The causes of primary vasculitis are unknown, so special prevention is not carried out. Prevention of secondary vasculitis is carried out in several directions and involves restoration and maintenance of normal health:
- reducing the risk of contracting hepatitis B virus, hepatitis C virus, and other infections;
- timely and correct treatment of any diseases and especially infectious ones;
- taking medications only as prescribed by a doctor;
- maintaining a healthy lifestyle: maintaining a normal weight, giving up bad habits, proper nutrition and sufficient physical activity;
- allergy control. If they exist, it is important to exclude allergic reactions to food and medicines.
Angiitis of the skin: Etiology and pathogenesis.
In recent years, the theory of the immune complex genesis of angiitis has become increasingly widespread, linking its occurrence with the damaging effect on the vascular wall of immune complexes deposited from the blood. Among the etiological factors leading to inflammation of the vascular wall, focal (less often general) infection caused by staphylococcus or streptococcus, mycobacterium tuberculosis, enterococci, yeast and other fungi, and influenza virus is most often called. Among exogenous sensitizing factors for angiitis, a special place is currently given to drugs, primarily antibiotics and sulfonamides. Chronic intoxication, endocrinopathies, various types of metabolic disorders, as well as repeated cooling, mental and physical stress, photosensitivity, arterial hypertension, and venous congestion can play a significant role in the pathogenesis of angiitis
Diet for vasculitis
The diet for vasculitis is designed to eliminate food allergies, normalize weight, and provide the daily requirement for calories, vitamins, minerals, etc. When forming a diet, they take into account the causes that provoked vasculitis and which organs were affected due to inflammation of the walls of blood vessels and poor circulation. For example, if the stomach or intestines are damaged, a special nutrition plan is needed.
General recommendations involve organizing a healthy diet: excluding foods that cause an allergic reaction, eating enough fresh vegetables and fruits, dairy products, cereals, excluding fatty, spicy, fried foods. In each individual case, you can contact a nutritionist for help in creating a diet.
Frequently asked questions about vasculitis
How does vasculitis manifest?
This disease has many symptoms. Common symptoms include malaise, fever, changes in blood pressure and disturbances in the circulatory system.
Why is vasculitis dangerous?
Vasculitis is an insidious disease that leads to tissue destruction and dysfunction of vital organs.
What happens if vasculitis is not treated?
Without proper treatment, the disease will progress and become more complicated, often resulting in disability or death.
Consequences and complications
Without treatment, vasculitis becomes a life-threatening disease. It can cause pulmonary, intestinal and intracranial bleeding, thrombosis, renal or liver failure, myocardial infarction, and aneurysms. Possible complications include:
- intestinal obstruction;
- peritonitis;
- pancreatitis;
- heart attacks, thrombosis, ischemia of tissues and organs;
- perforation of intestinal and stomach ulcers;
- neuritis, cerebral disorders.
Even with timely treatment of vasculitis and persistent remission of the disease, consequences are possible, including chronic diseases of the kidneys, liver, digestive organs, breathing, hearing loss, vision loss and others. In order to most effectively restore normal health and quality of life, long-term systemic therapy is carried out.
List of sources
- Dunaeva N.V., Nikitina O.E., Stukov B.V., Karev V.E., Mazing A.V., Lerner M.Yu., Lapin S.V., Totolyan A. Cryoglobulinemic vasculitis associated with chronic hepatitis B: clinical observations and literature review.
- Nasonov E.L., Baranov A.A., Shilkina N.P. Hemorrhagic vasculitis (Henoch-Schönlein disease) // Vasculitis and vasculopathies. - Yaroslavl: Upper Volga, 1999. - 616 p.
- Handbook of a practicing physician. Under. ed. Vorobyova A.I. “Medicine”, 1981.
- Shostak N.A., Klimenko A.A. Systemic vasculitis: new in classification, diagnosis and treatment. Clinician. 2015;9(2):8-12
- Shilkina N.P., Dryazhenkova I.V. Systemic vasculitis and atherosclerosis. Ter. Arch. 2007; 3: 84-92.
Forecast
Depends on the form, localization of vasculitis, severity of the disease. In some cases, primary vasculitis goes away without treatment and leaves no consequences at all. In others, the disease develops rapidly and is life-threatening. It is important to consult a general practitioner or rheumatologist in time, immediately after the first symptoms appear. The main danger with most forms of vasculitis is possible complications:
- severe cardiovascular diseases, heart attacks with polyarteritis nodosa;
- development of infections and pulmonary hemorrhages with microscopic polyarteritis;
- infections, renal, respiratory failure, cardiovascular accidents with Wegener's granulomatosis;
- partial or complete loss of vision with giant cell arteritis (but overall the prognosis is favorable);
- strokes, heart attacks with Takayasu arteritis.
To improve the prognosis, it is important to strictly follow the recommendations of the attending physician, try to prolong the remission of the disease, and eliminate factors that provoke relapses.
Valeria Korol – general practitioner, rheumatologist, Member of the expert council of MedPortal “How to avoid recurrent vasculitis?
— Avoid factors that can provoke an exacerbation of the disease:
- Infections
- Stress
- Exposure to direct sunlight
- Unmotivated medication use
- To give up smoking
- Normalization of body weight
- Valeria Korol
- general practitioner, rheumatologist"
Make an appointment.
The Medical Center of the Central Clinical Hospital of the Russian Academy of Sciences offers to make an appointment with the necessary specialists and undergo an examination in Moscow.
Prices for services
| Primary appointment (examination, consultation) with an allergist-immunologist | 2500 rub. | ||
| Appointment (examination, consultation) with an allergist-immunologist with an academic degree of K.M.N. (academic title “Assistant Professor”), primary | 2800 rub. | ||
| Repeated appointment (examination, consultation) with an allergist-immunologist | 1700 rub. | ||
| Primary appointment (examination, consultation) with a general practitioner | 2000 rub. | ||
| Appointment (examination, consultation) with a general practitioner with an academic degree of K.M.N. (academic title "Assistant Professor"), primary | 2300 rub. | ||
| Appointment (examination, consultation) with a general practitioner with an academic degree of D.M.N. (academic title "professor"), primary | 3000 rub. | ||
| Repeated appointment (examination, consultation) with a general practitioner | 1500 rub. | ||
| Immunocytochemical examination of urine | 1200 rub. | ||
| Detailed general (clinical) blood test | 850 rub. | ||
| Registration, interpretation, description and interpretation of electrocardiographic data (ECG) | 1000 rub. | ||
| Show all ↓ | |||