Blood pressure (BP) is an integral indicator of systemic blood flow. It includes two main values: experts call them systolic and diastolic pressure, and common people talk about upper and lower, respectively. The presence of a tonometer in almost every home allows you to monitor blood pressure levels at any time: morning and evening, at night, after meals, physical activity, etc.
Most patients roughly understand what numbers indicate increased or decreased indicators, especially if they change in direct proportion to each other. What to do if non-standard values appear on the tonometer and how to decipher them? This article will focus on just such a case – a pressure of 140 over 70. What this blood pressure level means, whether it is normal and whether correction of values is necessary is discussed below.
What is the danger of blood pressure 140/70, 140/60?
Despite the fact that blood pressure of 140/70 and 140/60 does not go beyond the maximum permissible values, it is often found in older people without any negative clinical symptoms, it is dangerous due to its pulse difference.
Normally, this difference between systolic and diastolic pressure should not exceed 50 units. The optimal pressure is 120/80, while the pulse interval is only 40 units. This is a benchmark indicator that should be strived for, even if systolic and diastolic blood pressure are above the optimum, but do not cause complaints or negative symptoms in a particular person.
The interval of blood pressure between the maximum permissible values in this case (120/80 and 140/90) refers to prehypertension: that is, blood pressure of 140/70 and 140/60 is not yet a disease, but it is no longer the norm, since the risk of developing cardiovascular complications.
It should be remembered that after 40, every additional millimeter of systolic pressure that exceeds the optimal value of 120 units increases the risk of death by almost 2%, and diastolic pressure by almost 1%.
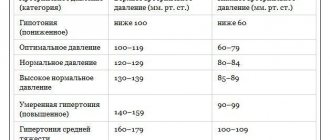
About pressure and its norm
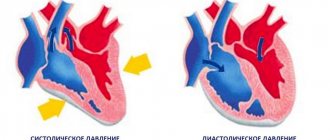
The first number of blood pressure is called the systolic indicator. This is the maximum value of blood pressure in the chambers of the heart and arteries at the height of contraction of the heart muscle. The figure has a direct relationship with the systolic volume of the heart, the contractile function of the myocardium, the pulse rate, the elasticity of the vascular walls and the volume of circulating blood, as well as the viscosity of the latter. The norm is not lower than 100 mm Hg. Art., not higher than 139 mm Hg. Art. The average optimal value is 120 mmHg. Art.
Diastolic indicator is the minimum value of blood pressure in the arteries and chambers of the heart at the end of the period of myocardial relaxation. Depends on heart rate and the degree of resistance to blood flow in the periphery. The norm is not lower than 60 mm Hg. Art., not higher than 90 mm Hg. Art. Optimal – 70–80 mmHg. Art.
There is another important indicator that not all patients know about: pulse pressure. Its significance also deserves detailed consideration. Pulse blood pressure is the result of the direct interaction of factors of the arterial system and stroke volume of the heart. The indicator is the functional equivalent of the pulse volume of blood, which enters the vessel during myocardial contraction and leaves it during the period of relaxation of the heart muscle.
The level of pulse pressure depends on the contractility of the heart, the magnitude of the reflection wave, the degree of distensibility and elasticity of the arteries. Calculation of the indicator = systolic blood pressure – diastolic blood pressure. Normal values are considered to be between 35 and 50 mmHg. Art. Pulse pressure control should occur dynamically. Why is that?
When measuring pressure, the upper and lower numbers on the tonometer correspond to different cardiac cycles, which means that one systolic (or diastolic) indicator may correspond to different values of pulse blood pressure. To characterize the patient’s hemodynamic state, it is necessary to obtain the relationship between all three indicators over a certain period of time. Only qualified specialists do this.
Pressure analysis 140 to 70:
- 140 is the upper limit, which can be a symptom of mild hypertension or be a normal “working” indicator for an elderly person;
- 70 is the absolute norm, but in the case of high “working” blood pressure in combination with poor health, it may be a manifestation of hypotension;
- 140-70=70 – high pulse pressure, which indicates the presence of pulse hypertension.
No ads 1
Causes
Triggers for an increase in the pulse difference at blood pressure 140/70 (140/60) in different age periods are different factors. For older people, isolated systolic hypertension is considered normal: upper pressure ≥ 140, lower pressure < 90, but a large pulse difference is most often a variant of the norm, although everything is individual and depends on the person’s well-being.
In this age category, an incorrect pulse interval can be caused by physiological reasons, which include one-time physical or psycho-emotional stress, fluctuations in atmospheric pressure, overeating, drinking alcohol or cigarettes, and sudden temperature changes. But more often it occurs in pathological conditions:
- changes in the distensibility or elasticity of the main main vessel of the heart - the aorta, this is age-related degeneration with the replacement of elastin with collagen, which is almost impossible to restore;
- atherosclerosis of blood vessels due to inflammation of the vascular wall, violation of its integrity and sedimentation of LDL in deformed areas;
- calcification of the arteries (the same process, but with the deposition of calcium on the vascular endothelium);
- hypothyroidism - the decline of thyroid function leads to disruption of the usual renewal of collagen and muscles, they lose elasticity, acquire increased strength (rigidity), in parallel, in the intercellular substance the connective tissue gel, which plays the role of a buffer, becomes denser, which also impairs the distensibility of blood vessels;
- diabetes mellitus, when high levels of insulin stimulate vasospasm, increasing the risk of the formation of atherosclerotic plaques;
- age-related impairment of kidney function - the accumulation of sodium ions in the arterial wall increases vascular spasm and disrupts glomerular filtration.
In young people, there are significantly more reasons for blood pressure 140/70 (140/60), but the most likely are:
- physical inactivity;
- obesity of varying degrees of genesis;
- stress, psycho-emotional exhaustion;
- atherogenic nutritional profile with a predominance of fats;
- abuse of alcohol, nicotine, other drugs, energy drinks;
- passion for salty foods (daily consumption of salt in excess of 7 g);
- low iron levels in the blood;
- physical stress;
- endocrine diseases (DM, hypothyroidism, menopause);
- heart defects: congenital or acquired;
- hereditary predisposition;
- tumors of the pituitary-hypothalamic system;
- kidney failure;
- varicose veins and other vascular pathologies;
- anemia;
- heart failure of varying degrees and forms.
Blood pressure of 140/70 (140/60) in children and adolescents, provided there are no physiological reasons: stress, overload, bad habits, clearly indicates the development of hypertension.
In pregnant women, a persistent change in blood pressure to 140/70 (140/60) leads to pathology of the placenta, fetal hypoxia and the formation of intrauterine diseases.
Prevention
To avoid the risk of hypertension, the following measures must be observed:
- sleep schedule should be 8 hours a day;
- saturate the menu with foods high in iron;
- avoid stress;
- be in the fresh air;
- do not smoke or drink alcohol;
- perform breathing exercises;
- normalize weight;
- monitor blood pressure readings.
If the first signs of pathology appear, contact the clinic in a timely manner.
Does it need to be adjusted?
In elderly patients, in the absence of complaints about general health and pathological symptoms, nothing should be done; this is an age-related physiological norm. In children and adolescents, blood pressure 140/70 (140/60) on an ongoing basis is always a reason to consult a doctor to identify the root cause of the symptom and appropriate treatment. In young people, everything is decided by concomitant symptoms and general well-being. If there are no negative symptoms, dynamic observation is needed with the development of an individual nutrition program and exercise therapy.
In pregnant women, the determining factor when blood pressure is 140/70 (140/60) is the condition of the fetus. Any minimal deviation from normal development is a reason for medical correction of the condition in a hospital setting.
Manifestations
Symptoms of a dangerous condition are observed in the following situations:
- sleep disturbance;
- knocking in the temples;
- tremor;
- weakness;
- may feel dizzy;
- memory deteriorates;
- pulse increases;
- heavy sweating;
- loss of consciousness;
- anxiety;
- meteorological sensitivity;
- heaviness in the eye sockets;
- swelling, chills;
- your leg may go numb;
- blurred vision;
- decreased hearing function;
- pain in internal organs;
- drowsiness develops;
- blood from the nose.
Normal blood pressure values are individual for each person, so if there are minor deviations from the standard and the severity of symptoms, you must seek qualified help to avoid serious complications.
First aid at home
At home, first aid before the arrival of doctors may be required only against the background of a sharp deterioration in health, which is associated with heart rhythm disturbances. By itself, blood pressure 140/70 (140/60) does not require any intervention. For tachycardia, in addition to rest, loosening tight clothing and allowing fresh air into the room, you can give sedative drops: Corvalol. If substernal discomfort occurs, use Nitroglycerin under the tongue.
In case of bradycardia, absolute rest is recommended; the patient should be placed in bed with a support for the back (a bolster, a blanket), a heating pad for the legs or a mustard plaster for the calves. No medications are given unless previously prescribed by a doctor.
Nutrition
If you have hypertension, the patient should adhere to a special diet. The menu for the week should consist of products that have antihypertensive properties. These include:
- oranges;
- apples;
- tangerines;
- lemon;
- vegetable and dairy soups;
- potato;
- fish;
- dried fruits;
- green tea;
- walnuts;
- raisin.
The patient needs to adhere to a diet without salt. Eliminate fatty foods, fried foods, and smoked foods from your diet. This food negatively affects the circulatory system of the entire body. A prerequisite for successful diet therapy is compliance with the drinking regime. You need to drink up to 2.5 liters of liquid per day.
When is emergency medical care needed?
Calling an ambulance is necessary when the blood pressure is 140/70 (140/60) and the pulse is critically slow, which is an indication for urgent surgery and installation of a pacemaker. The condition is dangerous due to disruption of the blood supply to vital organs.
In addition, calling an ambulance may be necessary if there are sudden complaints of chest pain, shortness of breath, cold profuse sweat and a feeling of fear of sudden death - this is a sign of developing ischemia, life-threatening.
Complications
With hypertension, serious forms of development of this disease can manifest themselves, and the initial pathology can behave extremely aggressively. With a sharp jump in blood pressure, a hypertensive crisis develops, provoking an active neurovascular reaction. A fatal complication of the disease is cerebral hemorrhage.
Another complication of hypertension is damage to the blood vessels of the brain. Vascular spasm occurs, giving impetus to the development of pathology. As a result, cerebral edema is possible, the consequence of which is the necrosis of small capillaries and neighboring tissue areas.
Among the complications of the pathology are heart failure and myocardial infarction. A very dangerous development of the disease is damage to the brain and kidneys. As the disease progresses, sclerotic tissue changes begin, caused by chronic ischemia. The organ is no longer able to function properly, which causes kidney failure.
Features of treatment
If necessary, blood pressure can be adjusted to 140/70 (140/60) using medications or traditional medicine. Massage and exercise therapy will also help.
Medications
Medicines are prescribed by a doctor; if blood pressure is 140/70 (140/60), special care is needed in selecting medications so as not to lower the diastolic reading. Use:
- ACE inhibitors for lowering blood pressure against the background of expanding the diameter of the lumen of blood vessels: Lisinopril, Captopril, Enalapril.
- Calcium antagonists to block the penetration of element ions into the cell: Norvasc, Amlodipine.
- Antispasmodics that relax smooth muscles: Spazmalgon, Drotaverine, No-shpa.
- Diuretics: Triampur, Veroshpiron, Spironolactone.
- Antioxidants and drugs that improve metabolism: vitamin C, E, Mildronate, Actovegin.
Folk recipes
Traditional medicine must be previously agreed upon with the doctor. The most popular: rosehip decoction, motherwort, oregano, hawthorn, St. John's wort. Beet and carrot juices. Apple cider vinegar lotions.
Nordic walking is the most effective exercise therapy; massage of the collar area gives good results.
Diagnostics
In order to establish the cause of the pathology, the doctor prescribes daily blood pressure monitoring and other clarifying studies for such patients. The most common:
- general blood and urine analysis;
- lipid profile;
- blood chemistry;
- blood sugar test;
- coagulogram;
- electrocardiogram;
- Ultrasound of the heart;
- Ultrasound of the kidneys and renal vessels.
If necessary, the patient is prescribed to undergo consultation with other specialists:
- vascular surgeon;
- endocrinologist;
- neurologist.