Pharmacological action, pharmacodynamics and pharmacokinetics
The main therapeutic effects of the drug:
- Decongestant.
- Diuretic.
The drug inhibits the enzyme carbonic anhydrase, which affects water and sodium metabolism in the body. As a result, Diacarb helps eliminate edema of various origins, relieve an attack of acute glaucoma and compensate for the manifestations of a number of other conditions.
By participating in water-salt metabolism, the drug does not affect pH and does not disturb the acid-base balance. The duration of action is no more than 12 hours.
The maximum concentration of Diacarb is achieved in the blood 2 hours after its administration. It has a high ability to bind to protein structures of blood plasma. Able to overcome the placental barrier.
The drug is not metabolized in the body and is excreted in its original form by the kidneys within 24 hours.
Interaction with other drugs
This drug is characterized by interactions with other drugs, which requires caution when prescribing complex treatment. If you are already taking any medication, your doctor should know about it.
- "Diacarb" has the ability to enhance the effect of certain medications. These include Ephedrine, anticoagulants, hypoglycemic drugs, folic acid antagonists.
- The concentration of phenytoin, muscle relaxants, and carbamazepine increases in the blood.
- Diacarb increases the side effects of taking Amphetamine, Atropine and Quinidine.
- The toxic effects of taking cardiac glycosides, Ephedrine, Carbamazepine, and non-depolarizing muscle relaxants increase.
- The simultaneous use of “Diacarb” and “Aminophylline”, “Theophylline” enhances the diuretic effect that the drug of interest to us has.
- A decrease in the diuretic effect is observed with the combination of Diacarb and ammonium chloride.
- A decrease in intraocular pressure is possible with the combination of Diacarb and anticholinergics, beta-blockers.
- The most dangerous is the combination of Diacarb and Aspirin (acetylsalicylic acid), especially with a high dosage of the latter drug. This combination can lead to anorexia, lethargy, tachypnea and even put a person into a coma.
Indications and contraindications
The following is a list of indications for the use of Diacarb:
- Edema of any origin (with mild or moderate severity).
- Acute attack of primary glaucoma.
- Epilepsy (as part of complex treatment of the disease).
- Pathology of the respiratory system, characterized by the accumulation of carbon dioxide and bicarbonate compounds in the blood plasma.
- Mountain sickness.
The drug is strictly prohibited for use in the following conditions:
- Individual intolerance to one or more components of the drug.
- Acidosis.
- Diabetes mellitus type 1 and 2.
- Addison's disease.
- Acute or chronic liver and kidney failure.
- Pregnancy.
- Lactation.
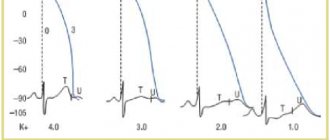
- Decreased potassium concentration in the blood.
How do Diacarb and Asparkam work?
The main thing in this scheme is Diacarb. But this drug, in addition to having a positive effect on the child’s health, also has a negative effect: it flushes potassium from the body. And since this microelement is necessary for the normal functioning of the heart, Diacarb for infants is prescribed exclusively in combination with Asparkam, which compensates for the lack of potassium. Otherwise, treating a newborn for increased intracranial pressure can cause heart failure.
Diacarb improves brain activity, “forces” all its cells to work more actively. Along the way, it helps to reduce the production of cerebrospinal fluid, due to which the pressure on the brain is reduced, and the child’s well-being noticeably improves.
When determining the exact dosage of drugs, the neurologist proceeds from the following data:
- patient's exact weight;
- amount of cerebrospinal fluid;
- general health of the child.
The standard for a child under the age of one year is to prescribe Diacarb once a day, 1/4 tablet, Asparkam - three times a day, but the exact dosage must be prescribed by the attending doctor. In case of acute hypokalemia (significant lack of potassium in the blood), Asparkam is prescribed not as tablets, but in the form of droppers or injections: the drug acts faster intravenously, but it must be administered by a qualified healthcare professional. The medicine is diluted with a 5% glucose solution - this protects against overdose.
Side effects and clinical manifestations of overdose
Short-term use of Diacarb can provoke the development of hypokalemia, paresthesia and limb cramps, muscle weakness, acidosis, visual and auditory disturbances, appetite disorders, itching, and an allergic reaction such as urticaria.
Long-term treatment with the drug causes drowsiness, dyspeptic syndrome, hemolytic anemia, leukopenia and agranulocytosis in some patients.
Overdose symptoms are similar to adverse reactions. Treatment is symptomatic. Immediate discontinuation of the drug and contact a doctor is necessary.
Discussion
Today, hydrocephalus remains the most common pathology encountered by neurosurgeons around the world. The most difficult group among them are patients with various variants of multilevel hydrocephalus, when the ventricular system is separated into multiple isolated chambers. Of course, the solution to this problem is only possible with surgical methods. However, there is still no consensus on which type of surgical intervention for this pathology should be preferred as the most effective and safe [2, 6—14].
The most common method of installing a shunt system may often require the implantation of several shunts and their multiple revisions [14–17]. Moreover, mortality in this pathology due to postoperative complications can reach 54% [4].
Another treatment option is to perform stereotactic aspiration of the cysts and create a communication between the cavities. However, the frequency of cyst recurrence with this technique remains quite high, reaching 80%, which is explained by the inability to perform stereotactic devascularization of the cyst or create a sufficiently wide window in the cyst wall [17, 18].
It is also possible to perform microsurgical dissection of cysts using transcallosal or transcortical access [19, 20]. The advantage of the microsurgical method is the possibility of the most adequate hemostasis during dissection under direct visual control using bipolar coagulation and hemostatic materials. Working under high magnification improves visualization and simplifies the creation of multiple anastomoses over a sufficient length. However, open interventions are not without drawbacks. Performing a transcallosal approach requires extensive experience and appropriate skill and carries the risk of sagittal sinus thrombosis, accidental injury to the pericallosal artery, venous infarction when crossing the transitional veins, and cognitive impairment due to damage to the corpus callosum [21].
The use of transcortical access can lead to the development of epileptic seizures in the postoperative period, to the formation of subdural accumulations of cerebrospinal fluid against the background of pronounced thinning of the brain cloak in hydrocephalus [4]. Retraction of the ventricular walls is also possible due to leakage of cerebrospinal fluid during cyst decompression [22]. In addition, additional craniotomy may be required in the presence of a fourth ventricular cyst or for placement of a shunt.
In our opinion, the most promising in this category of patients are neuroendoscopic interventions that make it possible to establish communication between the cavities by fenestrating their walls from one burr hole [2, 11, 23, 24]. In some cases, endoscopy can save the patient from a previously implanted shunt system or the need for its installation [2, 11, 25]. However, when performing such operations, the search and identification of targets for fenestration in conditions of altered anatomy and the absence of natural landmarks remains a rather difficult task. The use of navigation during such interventions can significantly facilitate the surgeon’s tasks and increase the efficiency of the operation [26–28]. The combined use of endoscopic techniques and frameless navigation virtually eliminates the need to use multiple approaches to create communication between multiple cavities in one patient, thereby stopping the progression of hydrocephalus in one intervention. Thanks to the operation, all patients in our group achieved improvement, which confirms the fairly high effectiveness of this type of intervention. In addition, the presence of intraoperative navigation control allows us to minimize the risk of damage to such important structures as large vessels, functionally significant areas and brain stem regions.
Neuroendoscopic interventions may be accompanied by complications such as intraventricular hemorrhage, ventriculitis, damage to nearby nerve structures and liquorrhea. In a study by N. El-Ghandour [11], among 24 children with multilevel hydrocephalus operated on endoscopically, 2 (8%) patients experienced minor arterial bleeding intraoperatively, which was stopped within a few minutes and did not require interruption of the operation. Subsequently, no additional neurological symptoms were noted in these patients and none of them required craniotomy. In 2 (8%) patients, liquorrhea was noted in the postoperative period, which resolved within 3 days [11]. In another group of 34 patients with complicated hydrocephalus who underwent endoscopic intervention, postoperative liquorrhea was noted in 1 (3%) case and a neuroinfection developed in 1 (3%) patient [23]. The complications we noted in 2 (18.2%) patients did not require additional intervention and, in general, did not affect the favorable outcome of the disease.
Instructions for use Diacarb
The daily dosage and treatment regimen may vary. Features of admission depend on the presence of concomitant diseases, the age of the patient, as well as the type and severity of the underlying pathology.
For mild and moderate swelling, you should take 250 to 400 mg of the drug per day once.
For the treatment of an acute attack of glaucoma, adult patients are prescribed 250 milligrams of Diacarb every 4 hours. For pediatric patients, the dosage is calculated at 10-15 mg per kilogram of weight.
To prevent mountain sickness, it is recommended to take 500 mg of the drug 1-2 days before and during the ascent.
For patients with epilepsy, Diacarb is prescribed in a dosage of 250 to 500 mg per day for three days.
Use in childhood
In pediatric practice, Diacarb is prescribed for the treatment of neurological diseases:
- hydrocephalus – accumulation of fluid due to increased synthesis of cerebrospinal fluid or impaired outflow;
- epilepsy with “small” seizures: partial (Jacksonian), myoclonus and absence seizures.
The most sensitive to the drug are disorders of liquor dynamics, which are accompanied by interstitial edema of the brain. This type of intracranial hypertension is caused by an increased content of Na+ ions and water in the periventricular (periventricular) white matter.
Clinical signs of pathology:
- Headache. Children complain of a feeling of “expansion”, “squeezing of the eyes.” Intensifies when tilting the head and coughing. The pain is most pronounced in the morning, immediately after waking up.
- Vomiting, after which the intensity of the symptom decreases.
- Congestion in the fundus is a pathognomonic (most specific) sign.
Conservative treatment of pathology involves:
- diet with limited salt intake;
- drinking regime (reducing the amount of fluid consumed);
- taking diuretics (Diacarba), glucocorticoids (in severe cases).
Surgical treatment is indicated if drug therapy is ineffective for 2 months. "Diacarb" for epilepsy in children is an auxiliary element for basic anticonvulsants.
Neurologists prescribe a combination of Diacarb and Asparkam once before routine vaccination (DPT, CPC, Imovax-Polio) in order to prevent complications in children at risk. Taking medications does not reduce the likelihood of developing seizures.
Parental complaints about prolonged crying, sleep disturbances, and increased excitability are not indications for taking the drug. To reduce nervous excitement in pediatric practice, Cinnarizine or Glycine is used.
How to take Asparkam and Diacarb correctly for children?
Prescription of medications in pediatric practice is carried out taking into account the child’s body weight. Doses and recommendations for taking Asparkam with Diacarb are presented in the table.
| Pathologies | Dosage calculation | special instructions |
| Hydrocephalus |
| Take in the morning, once |
| Epileptic seizures |
|
|
Correction of the dose and regimen of anticonvulsants is carried out 2 times a year.
Long-term diuretic therapy requires periodic monitoring of blood pH and water and electrolyte balance. Taking Asparkam with Diacarb is recommended for laboratory-confirmed hypokalemia and hypomagnesemia.
Reviews about the medication
Reviews from patients and doctors about the drug Diacarb are very different, both positive and negative.
Most patients note the high effectiveness of the drug, as well as its affordable cost.
Some patients speak negatively about Diakarb. For some it did not help at all, but for others it caused undesirable reactions, due to which they had to stop taking the drug. Most often, patients experience severe muscle weakness and cramps as a result of hypokalemia.
On thematic forums, the question often arises about the possibility of treatment with Diacarb during pregnancy and lactation. Currently, medical professionals do not prescribe it to expectant and nursing mothers, since there is no reliable data on the safety of its use in this category of patients.
Why do infants develop increased intracranial pressure?
Most often, this problem worries babies whose pregnancy had complications: severe toxicosis, entanglement in the umbilical cord, difficult childbirth can cause the development of this disease, namely ICP. These complications could be the reason that the child did not receive the necessary portion of oxygen while still in the womb; as a result, some brain cells cease to function properly, and cerebrospinal fluid is produced in excess and puts pressure on the brain with its volume. This is what causes frequent headaches, tears and poor sleep. Only the child cannot yet report this - therefore, parents, together with a doctor, need to conduct a series of studies to identify the exact cause.
A doctor can make an accurate diagnosis only after an ultrasound of the brain (this procedure can be performed on a child until the baby’s sac, the hole in the skull located at the top of the head, has become overgrown).