Hemostatic (antihemorrhagic, hemostatic) drugs are a group of drugs that are used to stop bleeding (hemorrhages) and prevent excessive blood loss.
Normally, blood is a fluid liquid - a suspension of formed elements (erythrocytes, leukocytes, platelets) in plasma. However, during bleeding, blood is able to change its rheological (fluid) properties - it becomes excessively thick and viscous, and then solidifies at the site of damage to the vessel wall (coagulates), forming a clot (thrombus). The thrombus closes the lumen of the wound and thereby prevents further bleeding and loss of blood from the body.
In case of extensive bleeding or in diseases that are accompanied by a violation of the formation of blood clots, the blood does not have time or is not able to clot in time. This leads to excessive blood loss, and then to shock, oxygen starvation of organs (especially the brain and heart) and the development of various kinds of negative consequences, including death. In this case, hemostatic drugs are used.
Indications for use
Hemostatic drugs are used for conditions associated with blood clotting disorders and bleeding.
Fibrinolysis inhibitors are used to stop severe bleeding during operations (especially on the heart, lungs, large vessels), extensive injuries, birth hemorrhages, reduced blood clotting in liver diseases, as well as in case of overdose of fibrinolytic drugs (fibrinolysin, streptokinase, alteplase, urokinase, tenecteplase and etc.).
Aprotinin is additionally used for diseases of the pancreas: acute pancreatitis (including alcoholic), severe injuries and pancreatic cancer.
Vitamin K preparations are used for bleeding associated with vitamin K deficiency in the body: hemorrhagic syndrome of newborns, liver diseases (cholelithiasis and obstructive jaundice) and intestinal diseases (enterocolitis, Crohn's disease). In addition, vitamin K preparations are used for bleeding caused by an overdose of indirect anticoagulants - warfarin, acenocoumarol, phenindione.
Herbal hemostatics are indicated for uterine bleeding (menorrhagia), minor bleeding from small vessels of the stomach and intestines.
Hemostatic drugs for local use are used to stop capillary and parenchymal bleeding (from internal organs) during open abdominal operations.
Etamsylate is used for the prevention and treatment of surgical bleeding, as well as for uterine, nosebleeds, bleeding gums due to periodontal disease, and gingivitis.
Eltrombopag and recombinant thrombopoietin are indicated for the treatment of idiopathic thrombocytopenic purpura - a chronically low level of platelets in the blood, which is dangerous due to frequent bleeding - when the spleen is removed.
Emicizumab is used to treat hemophilia, an inherited disease associated with blood clotting disorders and life-threatening bleeding.
Clotting factor drugs are used for severe, extensive bleeding, as well as for the treatment of hemophilia.
ANTICOAGULANTS AFFECTING THE BLOOD CLOTTING PROCESS
Preferanskaya Nina Germanovna Associate Professor, Department of Pharmacology, Educational Department, Institute of Pharmacy and Translational Medicine, First Moscow State Medical University named after. THEM. Sechenova, Ph.D.
Previously, readers became acquainted with fibrinolytic (thrombolytic) drugs, which are used to dissolve already formed blood clots. This article is devoted to means that prevent the formation of blood clots and prevent the occurrence of thrombosis.
Damage to the vascular wall initiates the process of blood clotting and thus stops bleeding from the damaged vessel. This complex multi-stage process requires the combined activation of plasma, vascular, and platelet factors. Most of them are plasma proteins that circulate in the blood in an inactive state, but are subsequently activated during the blood clotting process. The most important components are involved in this hemocoagulation cascade: fibrinogen (factor I), prothrombin (factor II), tissue thromboplastin (III), calcium ions (IV), proaccelerin (V), antifibrinolysin or proconvertin (VII), antihemophilic globulin A (VIII) , Christmas factor (IX) and Stewart-Prower factor (X), etc. Blood coagulation factors are proenzymes and, as a result of activation, are converted into proteolytic enzymes. At each stage, the inactive enzyme is converted into a more active enzyme.
The first stage in the formation of blood clots is the adhesion of platelets. Platelets do not adhere to intact endothelium or clump together (aggregation) unless the endothelium is damaged and subendothelial structures are present. Platelet adhesion occurs with the participation of a glycoprotein present in blood plasma, platelets and vascular endothelium, called von Willebrand factor . Von Willebrand factor binds to glycoprotein receptors, platelets acquire a spiky-spherical shape, which facilitates their aggregation and adhesion, i.e. their interaction with each other and with the surface of the damaged endothelium.
Von Willebrand factor and proaccelerin, after activation, act as cofactors that increase proteolytic activity. Proconvertin initially has low proteolytic activity, but as a result of interaction with tissue factor, its proteolytic activity rapidly increases. Activated proconvertin (corvertin), together with tissue factor and Ca2+ ions, forms a complex that causes partial proteolysis of Christmas factor and Stewart-Prower factor, they are activated. Active Christmas factor (IXa), in turn, additionally activates factor X. Active Stewart-Prower factor (Xa) acts on prothrombin (factor II) and converts it into active thrombin (IIa). Subsequently, platelets are activated by collagen and the first portions of thrombin formed in the vascular wall. Thrombin causes partial proteolysis of fibrinogen to form fibrin.
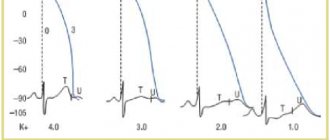
Proteolytic activation of blood coagulation factors is greatly accelerated when these factors bind through Ca2 + to negatively charged phospholipids of cell membranes. These phospholipids act as a kind of matrix on which coagulation factors are assembled into complexes with the participation of Ca2 + . At the same time, the rate of activation of factors in these complexes increases 50 times or more. A necessary condition for the formation of such complexes is the ability of factors II, VII, IX, X to bind to Ca2 + . The factors contain negatively charged γ-carboxyglutamic acid residues, which ensure their binding to Ca2+. The formation of γ-carboxyglutamic acids occurs in the liver with the participation of vitamin K. With a deficiency of vitamin K, defective blood clotting factors appear in the blood and the formation of fibrin threads is disrupted.
For the human body, it is optimal to have a balance between these processes (hemostasis system). The function of this system is to maintain the liquid state of the blood, stop bleeding, in case of damage to the walls of blood vessels and dissolve blood clots.
Depending on the nature, mechanism of action, speed and duration of influence on the process of thrombus formation, drugs are divided into the following subgroups:
- Direct anticoagulants acting on blood clotting factors.
- Indirect anticoagulants that interfere with the formation of prothrombin in the liver.
- Agents that affect platelet aggregation, lower the level of cytoplasmic Ca2+ and prevent platelet aggregation.
- Fibrinolytics (thrombolytics), stimulating the conversion of profibrinolysin into fibrinolysin and destroying fibrin threads (MA No. 11 - 12/16).
Anticoagulants are drugs that inhibit active coagulation factors directly in the vascular bed or disrupt the formation of coagulation factors in the liver and, thus, prevent the formation of blood clots. Violations of the blood coagulation process in one direction or another cause serious illnesses.
Indications for the use of anticoagulants are:
- prevention and treatment of thromboembolic diseases;
- prevention of thrombosis of coronary and peripheral arteries;
- unstable angina, myocardial infarction;
- prevention and treatment of deep vein thrombosis;
- pulmonary embolism;
- prevention of thrombus formation in atrial fibrillation;
- angioplasty of coronary vessels;
- prevention and limitation of thrombus formation during surgical interventions;
- maintaining the liquid state of blood in artificial circulation machines and flushing venous catheters;
- carrying out hemodialysis, hemosorption, peritoneal dialysis.
Direct anticoagulants prevent the formation of fibrin and promote the action of fibrinolytic factors on them. These drugs prevent the formation of blood clots or stop the growth of already formed blood clots.
CLASSIFICATION OF DIRECT ACTION ANTICOAGULANTS
1. Heparin preparations: Heparin standard (unfractionated), Heparin sodium (Lioton 1000, Trombless); 1a. Combined preparations containing heparin: Venolife, Venabos, Venitan forte, Gepatrombin, Gepatrombin G, Hepatrombin S, Heparin ointment, Dolobene, Contractubex, Nigepan, Trombless Plus, Troxevasin Neo; 2. Low molecular weight (fractionated) heparins: Nadroparin-calcium (Fraxiparin), Dalteparin sodium (Fragmin), Parnaparin sodium (Fluxum), Enoxaparin sodium (Antifibra, Clexane); 3. Dehydrogenated low molecular weight heparin - Bemiparin sodium (Tsibor 2500, Tsibor 3500); 4. Heparinoids mucopolysaccharides: Heparinoid Zentiva, Heparinoid Lechiva Sulodexide (Angioflux, Wessel Due F); 5. Direct inhibitors of blood coagulation factor Xa (activated Stewart-Prower factor): Apixaban (Eliquis), Rivaroxaban (Xarelto), Fondaparinux sodium (Arixtra); 6. Selective direct thrombin inhibitors: Bivalirudin (Angiox), Dabigatran etexilate mesylate (Pradaxa); 7. Antithrombin III drug - Antithrombin III human (glycoprotein); 8. Hirudin preparations: Lepirudin; 9. Medical leech, Piyavit (leech powder); 10. Sodium citrate, for blood preservation.
Direct anticoagulants act directly in the blood and are used parenterally and orally. When using these drugs, side effects may occur: hemorrhages, allergic reactions (urticaria, angioedema, etc.), thrombocytopenia, hyperkalemia, and with long-term use - osteoporosis, etc.
Heparin, a sulfated glycosaminoglycan (mucopolysaccharide), consisting of D-glucosamine and D-uronic acid residues. Produced by mast cells in many tissues; found in large quantities in the liver, lungs, and intestinal mucosa. For medical purposes, heparin is isolated from the mucous membrane of the pig intestine and from bovine lungs. The isolation process produces a mixture of fractions with different lengths of the polysaccharide chain and different molecular weights (from 3000 to 40,000 D). Fractions with different molecular weights differ somewhat from each other in biological activity and pharmacokinetic properties.
Heparin preparations obtained by different methods and from different sources may have different anticoagulant activity, as a result of which it is necessary to carry out their biological standardization. The activity of heparin is determined by its ability to prolong blood clotting time (1 mg of standard heparin contains 130 units).
The mechanism of action of heparin is complex. Heparin itself does not have an anticoagulant effect; it exerts its effect on blood coagulation factors only after the formation of a complex with the endogenous anticoagulant antithrombin III. Antithrombin III is a blood plasma glycoprotein synthesized in the liver. It is an inhibitor of serine proteases, which include blood coagulation factors IIa (thrombin), IXa and Xa (as well as XIa and XIIa). However, the process of inactivation of factors under the influence of antithrombin III alone proceeds very slowly. Heparin causes conformational changes in the antithrombin III molecule and potentiates its effects, which leads to an acceleration of this process by approximately 1000 times. The main action of the heparin-antithrombin III complex is directed against thrombin and factor Xa, but the mechanisms of inhibition of these factors have some differences. To inactivate thrombin, heparin must bind to both the antithrombin III molecule and the thrombin molecule. At the same time, rapid inactivation of factor Xa by the heparin–antithrombin III complex does not require binding of this factor to heparin. Fractions of heparin with a relatively short polymer chain cannot simultaneously bind antithrombin III and thrombin and therefore do not have antithrombin activity. Their action is mainly associated with the inactivation of factor Xa and, therefore, with the disruption of the conversion of prothrombin to thrombin.
Heparin is poorly absorbed when administered orally. Depending on the indications, heparin is administered intravenously (sometimes the first portions are drips), intramuscularly and subcutaneously. Heparin is dosed in action units, prescribed from 2000 IU to 5000 IU per day. For therapeutic purposes, it is administered intravenously; the dose and frequency of administration are determined individually, depending on the analysis of prothrombin time. When administered intravenously, the effect occurs immediately and lasts 4–6 hours. When administered subcutaneously, heparin begins to act in 30–60 minutes, the duration of action is 8–12 hours. For prophylactic purposes, it is used subcutaneously, administered every 8–12 hours. to the abdominal area, where there are fewer blood vessels and less danger of developing hematomas.
Heparin in the blood binds to many proteins, incl. with those that neutralize it (platelet factor). High levels of these proteins in the blood can cause relative resistance to the drug. In addition, heparin binds to macrophages and endothelial cells, and its degradation (depolymerization) occurs. Heparin is biotransformed by the liver, mainly by cells of the reticuloendothelial system, and is excreted by the kidneys in the form of metabolites.
Heparin is used for the prevention and treatment of deep vein thrombosis and pulmonary embolism, for unstable angina and myocardial infarction, for the prevention of thrombosis of peripheral arteries, for heart valve replacement and extracorporeal circulation. Heparin reduces blood lipid levels due to the activation of lipoprotein lipase, which hydrolyzes triglycerides to release free fatty acids.
With the simultaneous use of heparin with antiplatelet agents (especially aspirin), other anticoagulants, fibrinolytics and non-steroidal anti-inflammatory drugs, its anticoagulant activity increases and the risk of bleeding increases. Drugs that cause hypoprothrombinemia (cefamandole, cefoperazone, valproic acid) also increase the risk of bleeding. When used with nicotine, ergot alkaloids, thyroxine, tetracycline and antihistamines, the effect of heparin is reduced.
The most common complication of heparin therapy is bleeding, which may be caused by inhibition of platelet function or a decrease in their number (thrombocytopenia). The binding of heparin to von Willebrand factor appears to explain its inhibitory effect on platelet adhesion and aggregation. In such cases, heparin is discontinued, and in case of serious bleeding, it is necessary to administer intravenously a hemostatic agent (heparin antidote) - protamine sulfate, which neutralizes heparin, forming an insoluble complex with it. 1 mg per 100 units of heparin is administered.
In 1–5% of patients receiving heparin, thrombocytopenia is observed on days 7–14, which is caused by the appearance of antibodies against the heparin-platelet factor 4 complex. This complex is formed on the platelet membrane when heparin is neutralized by factor 4 (platelet-derived glycoprotein), which is released during platelet aggregation. Less than 1% of patients with thrombocytopenia experience thrombosis due to activation of platelets by antibodies to the heparin-factor 4 complex, which causes their aggregation. This condition requires discontinuation of heparin and administration of anticoagulants that do not cause thrombocytopenia, such as danaparoid and lepirudin.
With prolonged administration of heparin (more than 3 months), osteoporosis may develop. This is especially important to consider when prescribing heparin during the postmenopausal period. A fairly rare complication of heparin therapy is hyperkalemia associated with inhibition of aldosterone synthesis in the adrenal glands.
Heparin is contraindicated in patients with bleeding, hemorrhagic strokes and diathesis, hemophilia, thrombocytopenia, severe hypertension, patients with active tuberculosis and peptic ulcer disease, and pregnant women only for health reasons.
For thrombophlebitis of the superficial veins of the legs, trophic ulcers of the extremities and other thromboembolic diseases, heparin is used topically, in the form of ointments, gels, and suppositories. For this purpose, sodium heparin and combination preparations containing heparin are used.
Sodium heparin ( Lioton 1000, Trombless ) belongs to the group of medium molecular heparins, providing anti-inflammatory, antiproliferative, decongestant and analgesic effects. Reduces platelet aggregation, binds to antithrombin III, preventing the transition of prothrombin to thrombin. Inhibits the activity of thrombin, reduces the activity of hyaluronidase, and increases the fibrinolytic properties of blood. Improves microcirculation and activates tissue metabolism, thereby accelerating the processes of resorption of hematoma and blood clots, ultimately restoring the patency of the veins, which is accompanied by a pronounced analgesic and anti-inflammatory effect.
When Lyoton 1000 is used externally, its components have a local antithrombotic, antiexudative, and moderate anti-inflammatory effect. The drug is used for the prevention and treatment of deep vein thrombosis, peripheral venous diseases, thrombophlebitis, in the prevention and treatment of microthrombosis and microcirculation disorders. Lyoton 1000 in the form of a gel or ointment for external use is applied to the affected area (3–5 cm in diameter) 1–3 times a day.
In case of thrombosis of hemorrhoidal veins, rectal tampons or calico pads with ointment are applied directly to the strangulated nodes and fixed with a bandage. For the same purpose, you can use a tampon soaked in ointment, which is inserted into the anus.
The course of treatment with Lyoton 1000 is 3–4 days. In the case of a leg ulcer, carefully lubricate the inflamed skin around the ulcer, applying 2-3 times a day, daily, until the inflammation disappears, on average from 3 to 7 days, the possibility of a longer course of treatment is determined by the doctor.
Important! The gel/ointment should not be applied to open wounds, mucous membranes, or in the presence of purulent processes. The use of ointment is not recommended for deep venous thrombosis.
Trombless is a gel whose action is aimed at reducing the inflammatory process, blood clotting, reducing swelling of soft tissues and pain. The drug acts by reducing platelet aggregation by binding to antithrombin III, which does not allow prothrombin to transform into thrombin. Under the influence of the gel, blood flow in small vessels (capillaries) of tissues and tissue metabolism improves, which leads to the resorption of blood clots and hematomas, a decrease in inflammation and pain intensity .
Trombless Plus is a combination drug whose active ingredients are sodium heparin, troxerutin, dexpathenol and benzocaine.
Dexpanthenol provitamin B5 in the skin is converted into pantothenic acid, which is part of coenzyme A, which is involved in the processes of acetylation, carbohydrate and fat metabolism; stimulates skin regeneration, normalizes cellular metabolism, increases the strength of collagen fibers. The drug has a regenerating, vitamin, metabolic and anti-inflammatory effect.
Troxerutin is a derivative of rutin, has P-vitamin activity, has venotonic, angioprotective, decongestant, antioxidant and anti-inflammatory effects. Participates in redox processes, blocks hyaluronidase, stabilizes hyaluronic acid in cell membranes and reduces the permeability and fragility of capillaries, increases their tone. Increases the density of the vascular wall, reduces exudation of the liquid part of the plasma and diapedesis of blood cells. Reduces inflammation in the vascular wall, limiting the adhesion of platelets to its surface.
Benzocaine is a local anesthetic for superficial anesthesia. Reduces the permeability of the cell membrane to sodium ions, displaces calcium ions from receptors located on the inner surface of the membrane, and blocks the conduction of nerve impulses. Prevents the occurrence of pain impulses at the endings of sensory nerves and their conduction along nerve fibers. The drug dilates superficial vessels, promoting the absorption of heparin.
Agents with antithrombic and local anesthetic effects containing benzocaine include Heparin ointment and Nigepan , rectal suppositories. Gepazolon rectal suppositories contain lidocaine hydrochloride.
Hepatrombin (gel, ointment) is a drug that contains sodium heparin, allantoin and dexpanthenol, has antithrombotic, keratolytic and anti-inflammatory effects, improves tissue regeneration.
For hemorrhoids with complications in the form of thrombosis, for fissures and fistulas of the anus, for anogenital itching, Hepatrombin G - a drug with antithrombic, local anesthetic, venosclerosing, antiedematous, antipruritic and anti-inflammatory effects, which includes sodium heparin, lauromacrogol and prednisolone. Available in the form of rectal suppositories, ointments for rectal and external use.
Hepatrombin C and Dolobene (gel), which contain sodium heparin, dexpanthenol and dimethyl sulfoxide, are used for hematomas, inflammation of soft tissues, muscles, tendons, tendon sheaths, ligaments after bruises, compression, injuries (including sports); for bursitis, neuralgia, periarthritis, in the presence of damage to periarticular tissues. They have antithrombotic, anti-inflammatory effects, improve tissue regeneration.
For varicose veins of the lower extremities and thrombophlebitis, combination drugs with heparin containing troxerutin are used - Venolife, Troxevasin Neo, Venitan Forte . The drugs have an antithrombotic, venotonic, angioprotective effect, have P-vitamin activity, reduce vascular tissue permeability and capillary fragility, normalize microcirculation and tissue trophism, reduce congestion in the veins and paravenous tissues, causing an anti-edematous and anti-inflammatory effect.
Classification of hemostatic drugs
Hemostatic drugs are classified into:
- fibrinolysis inhibitors: amino acids (tranexamic acid, aminocaproic acid), protease inhibitors (aprotinin);
- vitamin K preparations: menadione, phytomenadione;
- herbal preparations: liquid extract of water pepper, nettle leaves, yarrow herb;
- hemostatic agents for local use: thrombin, fibrinogen, Ambien, calcium chloride;
- other hemostatic drugs for systemic use: etamsylate, eltrombopag, emicizumab, recombinant thrombopoietin.
In addition, preparations of proteins that regulate blood coagulation - coagulation factors II, VII, VIIa, VIII, IX, X and their combinations, von Willebrand factor, nonacog alpha - have a hemostatic effect.