Causes
There are two types :
- congenital;
- acquired.
The development of the disease is influenced by a certain number of aspects, among which are:
- Infectious (viral, bacterial, fungal, etc.).
- Helminthic infestations (echinococcosis, trichinosis).
- Factors of a toxic or chemical nature (insect bites, snake bites, exposure to chemicals on the body, drugs or alcohol).
- Aspects of physical health (overwork, overheating).
- The influence of drugs and other means (vaccination, antibiotics).
- Allergic reactions.
From the above reasons, it becomes clear that the disease can mainly manifest itself in children who have had viral or bacterial infections ; in addition, such children are susceptible to allergic reactions. Therefore, it is a good idea for parents to limit the consumption of foods to which the baby is allergic. Otherwise, you can only aggravate the situation and only cause harm.
Read also: Ultrasound of the child’s heart (echocardiography)
Myocarditis is inflammation of the heart muscle. The disease is usually caused by a viral infection, but can be caused by a bacterial or fungal infection, alcohol abuse, certain autoimmune disorders, and medications. Weakening of the body's defenses and autoimmune disorders are important predisposing factors to the disease.
Myocarditis occurs at any age, with equal frequency in men and women. Most often it occurs under the guise of the infection that caused it and may go unnoticed. In severe forms, cardiac failure develops, which reduces blood delivery to organs and tissues. Blood clots may also form, leading to a stroke or heart attack.
For mild forms of myocarditis, no special treatment is required; the underlying disease is treated. In complicated forms, treatment is aimed at restoring normal heart function and correcting immune disorders. In severe forms of heart failure and blockage of blood vessels by blood clots, surgical intervention may be required.
Synonyms Russian
Inflammation of the heart muscle.
English synonyms
Myocarditis.
Symptoms
Symptoms of myocarditis are varied and may vary depending on the cause and severity of the disease. Mild forms may be asymptomatic or disguised as a viral infection. In severe cases, signs of heart failure come to the fore.
Heart symptoms include:
- chest pain, often radiating to the left arm;
- palpitations;
- rapid pulse;
- shortness of breath during exercise, and then at rest;
- swelling in the ankles and feet;
- fatigue.
General manifestations of infection:
- weakness;
- sweating;
- headache;
- pain in joints and muscles;
- fever;
- a sore throat;
- diarrhea.
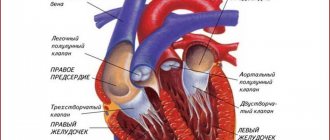
General information about the disease
Inflammation of the heart muscle can occur against the background of any infection, most often viral. Cases of non-infectious myocarditis are also quite common and can be caused by certain medications, harmful chemicals or radiation. In many cases, the exact cause cannot be determined.
The most common causes of infectious myocarditis include:
- viral infections, among which the most important are Coxsackie enterovirus, influenza A and B, measles, rubella, infectious mononucleosis and hepatitis B;
- bacterial infections, primarily staphylococcal, streptococcal and diphtheritic;
- some parasites, primarily trypanosomes and toxoplasma;
- fungi (candida, pathogens of aspergillosis and histoplasmosis).
Non-infectious factors causing myocarditis:
- medications (antibiotics, sulfonamides);
- narcotic substances (cocaine);
- excess thyroid hormones;
- renal dysfunction;
- serums and vaccines;
- connective tissue diseases (nonspecific ulcerative colitis, scleroderma, rheumatoid arthritis, rheumatism, systemic vasculitis, Wegener's granulomatosis, systemic lupus erythematosus);
- injuries and burns;
- factors of unknown origin (idiopathic myocarditis Abramov-Fiedler).
Regardless of the cause of the disease, the changes that occur in the heart muscle are of a similar nature. As a result of inflammation, myocardial edema develops and its blood supply deteriorates. Individual cells can be destroyed with the release of substances into the blood, including protein fragments, which are perceived by the body's defense system as foreign due to their similarity to the proteins of some bacteria and viruses. This leads to activation of the immune system and the development of a reaction to its own tissues. The severity of these reactions largely determines the severity of the disease.
According to the course, acute and chronic myocarditis are distinguished. The course of the disease largely depends on its cause. Infectious myocarditis is most often acute or subacute, sometimes recurrent, and rarely becomes chronic. Non-infectious myocarditis usually turns into a chronic progressive form with the development of complications such as increasing heart failure, heart rhythm disturbances, blood clots, and heart attack.
Who is at risk?
- Suffering from systemic and autoimmune diseases.
- Patients with rheumatism.
- Having undergone heart surgery.
- Pregnant women.
Diagnostics
Diagnosis of myocarditis is difficult due to the similarity of the clinical picture with many other diseases. One of the warning signs may be the appearance of shortness of breath two weeks after a viral infection. The diagnosis of “myocarditis” is made based on the medical history, laboratory data and special research methods. If an infectious nature of myocarditis is suspected, a blood test should be performed for certain viruses, bacterial or fungal infections. The scope of laboratory tests is determined by the attending physician based on the specific manifestations of the infectious process. In most cases, the decisive factor in making a diagnosis is a myocardial biopsy.
Laboratory research
- Complete blood count (without leukocyte count and ESR) Red blood cells and hemoglobin may be reduced in severe forms of myocarditis.
- Leukocytes. An excessive number of leukocytes with a shift in the leukocyte formula to the left (the appearance of young cellular forms in the blood) is observed in bacterial myocarditis. With myocarditis caused by a viral infection, significant changes in the leukocyte formula, as a rule, do not occur. The number of eosinophils may increase, indicating an allergic reaction.
- Rheumatoid factor is an antibody detected in the blood of people who suffer from certain connective tissue diseases. In myocarditis, a positive rheumatoid factor indicates the presence of an autoimmune component of inflammation.
- Antistreptolysin O - test for the presence of antibodies to streptococcus in the blood. Prescribed for suspected myocarditis of streptococcal origin.
- Total protein and protein fractions in the blood may be reduced in myocarditis. A significant decrease in total protein levels can be observed in severe forms of the disease.
- Alanine aminotransferase (ALT), Aspartate aminotransferase (AST). ALT and AST are enzymes mainly found in the cells of the liver, pancreas, and heart muscle. Their elevated levels in the blood serum may indicate destruction of myocardial cells.
- Fibrinogen. Fibrinogen is one of the main components of the blood coagulation system. Increased fibrinogen levels are typically observed during active inflammation in response to tissue damage. Fibrinogen produces another protein, fibrin, which is involved in the formation of blood clots. In myocarditis, elevated fibrinogen levels may indicate a risk of thrombotic complications.
- Markers of myocardial damage: troponin and creatine kinase-MB may increase during the acute phase of myocarditis. An increase in their level in the absence of clinical myocardial infarction is of diagnostic significance. Troponin I is one of the proteins present in cardiac muscle. When damaged, troponin is released and its concentration in the blood increases. Increases in troponin levels in myocarditis can be observed in the acute phase of the disease. Creatine kinase-MB is an enzyme found in the heart muscle and is released when its cells are destroyed. In myocarditis, just like troponin, it may indicate myocardial damage.
- Antibodies to the myocardium. An allergic or autoimmune component of inflammation is present in the vast majority of cases of the disease, both infectious and non-infectious in origin. The appearance of antibodies to the heart muscle is one of the main indicators confirming the diagnosis.
- A blood test for antibodies to individual pathogens may be prescribed to confirm the infectious nature of the disease. For myocarditis, blood tests for:
- Flu
- Hepatitis B
- Candidiasis
- Streptococcal infection
Additional tests for suspected myocarditis include:
- Ultrasound of the heart (echocardiography). Allows you to evaluate the size and function of the heart. An echocardiogram can detect an enlarged heart, signs of developing heart failure, the manifestation of which on echocardiography is a decrease in ejection fraction. It is estimated as the percentage of blood volume entering the aorta during heart contraction and remaining in it. The lower the ejection fraction, the more severe the degree of cardiac dysfunction. An indicator below 35% indicates a high risk of developing arrhythmias. Echocardiography can also help rule out other diseases that have similar symptoms.
- An ECG allows you to record changes in heart rate, disturbances in cardiac conduction and rhythm, and suspect previous myocarditis. In severe forms of myocarditis, changes on the cardiogram may resemble those during myocardial infarction.
- Cardiac magnetic resonance imaging (MRI). Allows you to see the position and size of the heart, its shape and structure. MRI can show signs of myocardial inflammation.
- Myocardial biopsy. Using a special instrument, you can take fragments of the heart muscle for examination under a microscope. In this case, characteristic signs of inflammation and edema in muscle tissue are visible, as well as destroyed myocardial cells in severe cases of the disease. The method has high diagnostic accuracy and allows you to confirm or refute the diagnosis of myocarditis in cases where other research methods are insufficiently informative.
- Coronarocardiography. A method in which a radiopaque substance is injected into the vessels of the heart using special catheters. The method is important for excluding coronary heart disease, which in many cases should be differentiated from myocarditis.
Treatment
Treatment of myocarditis depends on the cause that caused it and the stage of the disease. In mild cases, restriction of physical activity is indicated; in more severe cases, bed rest is indicated. Salt restriction is recommended. Drug treatment may include:
- Antibiotics - prescribed when the bacterial nature of myocarditis is confirmed
- Steroid hormones - to suppress the autoimmune reaction and the allergic component
- Drugs that lower blood pressure and affect heart rate may be prescribed to reduce the workload on the heart.
- Diuretics to reduce swelling
In severe cases with the development of chronic heart failure, a pacemaker may be required or a heart transplant may be considered.
Prevention
There is no specific prevention of myocarditis. Basic measures to prevent myocarditis include:
- Scheduled preventive vaccinations
- Limiting contact with persons suffering from acute viral infection
- Timely treatment of viral diseases
- Maintaining personal hygiene rules
- A healthy lifestyle that eliminates the risk of HIV infection, avoiding drugs, limiting alcohol.
Recommended tests
- Erythrocyte sedimentation rate (ESR)
- Leukocyte formula
- General blood analysis
- General urine analysis with microscopy
- Total protein in urine
- Fibrinogen
- Serum albumin
- Total protein in whey
- Protein fractions in whey
- Serum creatinine
- Urea in serum
- Rheumatoid factor
- C-reactive protein, quantitative
- Total immunoglobulin A (IgA) in serum
- Total immunoglobulin G (IgG) in serum
- Antibodies to myocardium
- Troponin I (quantitative)
- Creatine kinase MB
- Influenza virus A/B (influenza viruses A/B), RNA [real-time PCR]
- HBV, DNA quantitative [real-time PCR]
- Candida albicans, IgG, titer
- Mumps Virus, IgG
- Varicella Zoster Virus, DNA [real-time PCR]
- Epstein Barr Virus, DNA [real-time PCR]
- HIV 1.2 Ag/Ab Combo (determination of antibodies to HIV types 1 and 2 and p24 antigen)
- Streptococcus pyogenes, DNA [real-time PCR]
Myocarditis - symptoms
The distinctive characteristics and features of the manifestation of inflammation alone are not known; the disease can manifest itself against the background of others, so it is often not possible to determine it in a timely manner. But there are characteristic symptoms of myocarditis that doctors highlight:
- severe or aching pain in the heart area;
- irregular rhythm or pulse, it seems as if the heart is “turning over”;
- shortness of breath that occurs regardless of the intensity of physical activity;
- cough;
- blue nose, legs, arms;
- circulatory disorders;
- swelling in the legs;
- rapid patient fatigue;
- Increased body temperature is less common;
- general weakness.
Particular attention should be paid to newborn children ; if you notice signs of illness in them, then immediately seek the advice of your attending physician , who will help identify the illness that has appeared in time.
Publications in the media
Almost any term in Latin with the ending “it” means inflammation: bronchitis is inflammation of the bronchi, tonsillitis is inflammation of the tonsils, etc. Myocarditis is inflammation of the muscle tissue of the heart. Similar to inflammation of any skeletal muscle after a sprain or hypothermia, which is manifested by pain, impaired muscle function, local swelling and redness, pain and decreased contractility also occur in the heart muscle. Due to inflammation, the current of impulses through the conduction system of the heart slows down - blockade and heart rhythm disturbances develop.
Myocarditis can occur with any acute or chronic indolent infectious disease. Most often, myocarditis develops due to viral infections. Non-infectious factors that cause myocarditis include some medications, including antibiotics, sulfonamides, etc., as well as vaccines and inoculations. In addition, myocarditis often accompanies systemic connective tissue diseases, for example, systemic lupus erythematosus, rheumatoid arthritis, and vasculitis. Among the causes of myocardial inflammation, a special place is given to rheumatism, in which myocarditis is one of the main and leading manifestations of the disease along with endocarditis and pericarditis - inflammation of the inner and outer lining of the heart, respectively.
There is also idiopathic (that is, without an obvious known cause) myocarditis, which is called Abramov-Fiedler. Moreover, in the classic course of the disease, examination and blood tests do not reveal the infection that provoked myocardial inflammation.
According to the course, acute, subacute and chronic myocarditis are distinguished. In a chronic course, depending on the frequency of relapses, cardiac function can significantly decrease and chronic heart failure develops.
Quite often, myocarditis is not accompanied by significant symptoms of the disease and is recognized only during an instrumental examination, sometimes performed for another reason. Complaints may be limited to general weakness, chest discomfort, palpitations, a slight increase in body temperature - nonspecific complaints, for which not everyone goes to the doctor, and almost no one comes to the cardiologist.
In typical, clinically pronounced cases, there are complaints of prolonged pain in the heart area not associated with physical activity, weakness, increased fatigue, shortness of breath and palpitations even at rest, and interruptions in cardiac function. Body temperature is often subfibrile: 37-37.90C.
Myocarditis begins against the background of an acute infectious disease or shortly after it. The malaise intensifies and the above complaints appear. Sometimes the pain in the heart is persistent and long-lasting. Body temperature is normal or slightly elevated. The severity of symptoms is determined by the prevalence of the inflammatory process in the myocardium - how much of the heart muscle is involved in inflammation and begins to work worse - to contract. Due to a decrease in myocardial tone, the size of the heart increases, the normal functioning of the valves is disrupted, and cardiac output decreases. Myocarditis can be complicated by the development of acute heart failure - a reason for emergency hospitalization and intensive care.
Myocarditis can occur in two clinical forms: infectious-toxic (heart lesions appear during a period of severe intoxication against the background of infection) and infectious-allergic (the infectious agent triggers an excessive immune response of the body and the body’s own immune cells begin to fight and destroy their own cells in different organs , including hearts, which in a number of ways are a little similar to bacteria and viruses. Therefore, the immune system cannot distinguish body cells from harmful microbes. That is why infectious-allergic myocarditis can occur and continue after the end of the infectious process that caused it.
Idiopathic myocarditis
Idiopathic myocarditis, in which there is no clearly established cause for the development of inflammation in the myocardium, is characterized by a more severe, sometimes fulminant course with the rapid development of a large “flabby” heart and heart failure. Without timely help, most often, such myocarditis is fatal or requires an urgent heart transplant, which in our country, unfortunately, is not always possible. In a large heart, blood flow slows down significantly, valve function is disrupted, and cardiac output decreases. The walls of the heart are stretched so much that even after successful treatment, changes in the myocardium can be irreversible. In idiopathic myocarditis, both rhythm disturbances and the formation of blood clots inside the heart due to its expansion and turbulent blood flow, which can enter the brain and lungs, leading to fatal thromboembolic complications - pulmonary infarctions, strokes, etc., are deadly in idiopathic myocarditis.
Myocarditis in children
Myocarditis in a child, as well as in an adult, occurs as a result of an infectious factor. In children, due to the failure of the immune response to a number of bacteria and viruses that adults are more “familiar” with, even a mild infection can lead to generalization - complications in other organs, most often the heart and kidneys. Children are characterized by the presence of two types of myocarditis:
1. Congenital - in this case, from the day of birth, the child exhibits lethargy, pallor, shortness of breath, changes in the ECG, low blood pressure, weak sucking reflex, etc. The child does not gain weight. Jaundice prolongs due to insufficient blood supply to the liver. The situation requires immediate treatment. Most often, this condition is associated with an intrapartum infection - then antibiotics are quite effective and the process is reversible. If congenital myocarditis is associated with impaired immunity and occurs as part of an autoimmune process, treatment is more complex, the prognosis is worse, and death is possible.
2. Purchased. This type of myocarditis, as in adults, is divided into acute, subacute and chronic, and is most often a consequence of ARVI. The child's appetite decreases, anxiety occurs during the day and sleep disturbances at night, episodes of cyanosis (blue face) and shortness of breath, increased body temperature. In this case, examination and observation by a cardiologist is mandatory.
Instrumental examination methods
In a blood test, the level of inflammation indicators increases - leukocytes, ESR, C-reactive protein, etc., but, unlike a banal infection, with myocarditis the level of enzymes in the blood increases - MB-CPK and troponin. These enzymes are normally found inside the muscle cells of the heart. During inflammation, which leads, among other things, to disruption of the integrity of cell membranes, enzymes enter the blood and their level is proportional to the number of damaged cells. This happens when the myocardium becomes inflamed or damaged during a heart attack.
The ECG records certain changes that are characteristic specifically of myocarditis, although often difficult to distinguish from ischemic ones. Almost always, with myocarditis, ECG reveals disturbances in heart rhythm and conduction.
Ultrasound of the heart - decreased myocardial contractility, expansion of the cavities of the heart, accumulation of fluid around the heart and other specific changes.
Forecast
With Abramov-Fiedler myocarditis, myocarditis against the background of sepsis (severe generalized infection and damage to almost all organs), the prognosis for life is unfavorable - mortality up to 50-60%.
With infectious myocarditis, with timely and adequate treatment, in most cases, myocarditis is asymptomatic and ends with complete recovery. Occasionally, changes in ECG or cardiac ultrasound data will persist for a long time. Most often, there are no signs of previous myocarditis 2-3 months after the end of the disease. Other forms of myocarditis with an acute and subacute course in at least 1/3 of cases result in complete recovery, and mortality in Russia reaches 5-10%.
Prevention
Prevention is the prevention and timely effective treatment of infectious diseases. If signs of infection appear, you should consult your doctor. Of course, a runny nose can be treated at home, but without a doctor and a basic examination you will not be able to distinguish between a “lingering” runny nose and the onset of an inflammatory process in the heart. It is also important to treat infectious diseases. Do not stop therapy prematurely, including antibiotics, even if nothing bothers you anymore.
If you have had myocarditis, you need to be examined and treated with greater care and attention for any, even “harmless” infection. If you are planning to undergo any surgical intervention, including tooth extraction, warts or skin papillomas, etc., be sure to undergo antibiotic prophylaxis under the supervision of a doctor.
Indications for hospitalization
In this matter everything is extremely simple. Suspicion of acute myocarditis or exacerbation of chronic myocarditis is an undeniable indication for hospitalization. Myocarditis is not treated at home, no matter how severe it is. Severe arrhythmias and acute heart failure can develop suddenly, and you will miss the moment to begin adequate treatment.
Treatment of myocarditis is carried out exclusively in a hospital under the dynamic supervision of a doctor. Antibiotics and anti-inflammatory drugs, including hormonal ones, are prescribed, the pulse rate is reduced and, if necessary, drugs are prescribed against disturbances in heart rhythm and conduction.
Cardiologist, Ph.D. Zaikina Alexandra
Myocarditis - how is diagnosis done?
At the first signs, immediately contact a clinic where competent doctors work. They will conduct a targeted examination and give directions for further, detailed examination. But, there are stages of diagnostics:
- External examination of the baby . An experienced cardiologist immediately diagnoses that the heart muscle is inflamed. A blue tint to the face, swollen legs, swollen veins, hard breathing, all this makes it clear to the specialist that it is necessary to check the functioning of the heart as a whole.
- Percussion . At this moment, the doctor “tapping” and accurately determines the boundaries of the expansion of the heart muscle.
- Using a phonendoscope, the doctor listens to the frequency and rhythm of the heartbeat;
But, unfortunately, not every pediatrician is able to make a correct and clear diagnosis, so most likely you will be referred for a thorough examination using special devices that will give a complete picture of the child’s condition. Myocarditis and its diagnosis require increased attention from parents ; some notice manifestations quite late, which significantly aggravates the situation.
DIAGNOSIS AND TREATMENT of myocarditis
Myocarditis is a clinical syndrome characterized by many possible causes and manifestations. It is believed that viral infection is the most common cause of myocarditis, but similar changes can be caused by other infectious and non-infectious factors, the impact of which leads to inflammatory infiltration between cardiomyocytes.
Not only the causative factors of this pathological condition, but also its manifestations are very diverse. The diagnosis is clear in the presence of clear and characteristic signs of acute cardiac dysfunction that has arisen in connection with a viral disease, but with an erased clinical picture, diagnosing myocarditis is a very difficult task.
Definition. Myocarditis is a pathological condition in which an active inflammatory process occurs in the myocardium with necrosis and degenerative changes in cardiomyocytes; the pathomorphological picture differs from the changes observed during infarction. Cell death and fibrosis are observed. Inflammatory infiltration can be represented by any type of immune cells, and the histological nature of the inflammatory reaction often indicates the etiological factor.
Morbidity. It is difficult to give exact figures regarding myocarditis, since this pathological condition is very heterogeneous: in some cases it occurs hidden and therefore does not come to the attention of doctors; its chronic form can lead to dilated cardiomyopathy with manifestation many years after the onset of the disease.
Myocarditis is found in 1-4% of routine autopsies. In Europe and North America, viral infections are considered the most common cause of myocarditis. Cardiac pathology, according to some estimates, develops in 5% of all cases of viral diseases; however, clinically significant cardiac damage, according to large studies, is observed in 0.5-5.0% of cases.
The incidence is influenced by extreme factors, including age, as well as pregnancy and time of year. The incidence of myocarditis is high in infants, with a second peak in adolescence.
Etiology. The inflammatory response in the myocardium can arise from a number of different influences that damage cardiomyocytes (see table). Viral infections are considered the most common cause of myocarditis.
The mechanisms of damage to cardiomyocytes during viral infections are being actively studied: it is currently believed that viruses change the antigens expressed by cardiomyocytes, therefore, in addition to the direct replication of the pathogen, these cells are damaged by a constantly ongoing cellular immune reaction.
If this is so, then the immune response in a given patient determines the clinical manifestations of the infection.
Coxsackie viruses A and B, enteroviruses and influenza viruses are the most common etiological factors of myocarditis. Approximately 25-40% of patients infected with HIV (human immunodeficiency virus) show signs of cardiac dysfunction, which manifests itself clinically in 10% of cases.
Recently, there has been increasing recognition of the fact that cardiac pathology can also develop as a long-term complication of radiation therapy, with damage to the myocardium, valves or arteries - sometimes many years after irradiation. More advanced radiation therapy techniques are designed to protect against such complications.
Pathomorphology. Direct exposure to ionizing radiation, exposure to a toxin (such as in diphtheria), or an autoimmune reaction (such as in Mycoplasma pneumoniae infection) can damage cardiomyocytes and cause heart failure and arrhythmias, with the clinical picture depending on the extent of the damage.
Inflammation gives the myocardium a pale tint with rare small hemorrhages. Microscopy reveals a disturbance in the structure of muscle fibers due to interstitial edema and isolated foci of necrosis. The inflammatory infiltrate is usually represented by lymphocytes.
Depending on the etiological factor, more specific histological features may be found, such as non-caseating granuloma in sarcoidosis (see Fig. 1). Subsequently, complete resolution of the process often occurs without residual fibrosis, but in some cases focal healing with interstitial fibrosis is observed.
| Figure 1. Myocardial biopsy specimen for sarcoidosis (hematoxylin and eosin staining): inflammatory lymphocytic infiltration and non-caseating granuloma are visible |
Clinical signs. Clinical manifestations are very diverse and depend on the degree of cardiac dysfunction and the nature of the etiological factor.
Viral myocarditis may be preceded by a prodromal phase with flu-like symptoms, fever, muscle and joint pain, and rash. The time between the appearance of these signs and the onset of symptoms of cardiac pathology can range from several weeks to several years. Coxsackievirus appears to be the most cardiotoxic, especially in children.
Myocardial damage first manifests itself in the form of fatigue, shortness of breath, chest pain and palpitations, sometimes in the form of fainting. These symptoms are explained by insufficiency of systole and damage to the conduction system.
Chest pain may be associated with body position and movement, suggesting the possibility of pericarditis. In severe cases, acute left or right ventricular failure and cardiogenic shock occur. Sudden death may occur due to abnormal heart rhythms.
Physical examination reveals signs of heart failure: tachycardia (in classic cases, it is more pronounced than could be explained by fever), gallop rhythm, and in more severe cases, pulmonary edema or peripheral edema. The heart size is usually normal, and a murmur of mitral regurgitation may be heard. Sometimes atrial fibrillation develops. In some cases, a pericardial friction rub may be heard.
Diagnostics. There are no specific clinical signs on the basis of which this diagnosis could be made. The combination of an acute infectious disease and symptoms of myocardial pathology gives reason to suspect myocarditis.
Myocardial pathology can be judged on the basis of ECG data (see Fig. 2), chest x-ray, echocardiography and determination of the level of cardiac enzymes. Pathological signs on the ECG are often observed in the form of nonspecific changes in the ST segment and T wave.
An X-ray of the chest organs reveals signs of pulmonary edema, and the heart may be enlarged. Echocardiography often reveals left ventricular dysfunction, and this change may be regional rather than diffuse. Nonspecific indicators of inflammation: leukocytosis, erythrocyte sedimentation rate, and C-reactive protein also help make the diagnosis.
The presence of an acute viral infection is confirmed by analyzing swabs from the throat, stool, and also on the basis of serological tests (which can reveal a fourfold increase in antibody titer). Sometimes it is possible to isolate the pathogen from fluid taken from the pericardial cavity.
Among the more complex research methods, gallium-67 scanning can be noted, which can detect an active inflammatory process.
Some tertiary centers advocate myocardial biopsy.
Treatment of myocarditis is carried out with the aim of:
- maintaining the pumping function of the heart and reducing the risk of progression of heart failure,
- fight against arrhythmia,
- identifying and eliminating sources of toxicity.
Ideally, all patients with suspected myocardial damage should be admitted to hospital and monitored to see how effective the treatment is.
General supportive measures include bed rest and restriction of physical activity. Animal experiments have clearly shown that exercise during acute myocarditis is harmful; During the recovery period, patients should be advised to limit sports activities. This is important given that many patients suffering from this disease are young.
In the acute phase of myocarditis, the condition of patients must be carefully monitored. For congestive heart failure, conventional treatment with diuretics and angiotensin-converting enzyme inhibitors is effective, as well as anticoagulant therapy when there are signs of peripheral or pulmonary embolism, severe ventricular failure, or atrial fibrillation.
In some cases, a clinical picture of cardiogenic shock and low ventricular output is observed, and adequate intensive care is necessary.
Arrhythmia may occur, requiring specific therapy. Occasionally, there is a need for temporary or permanent implantation of artificial pacemakers. It is generally accepted that the risk of sudden cardiac death is increased following myocarditis, especially in younger patients.
Specific therapy directed at the causative factor is limited. Since in most cases myocarditis develops against the background of viral infections and is based on immunological reactions, some studies have examined the role of antiviral and immunosuppressive therapy. Many of these studies were poorly controlled and their results were inconclusive. Currently, there are no clear data on the basis of which immunomodulatory therapy can be recommended.
It is best not to prescribe non-steroidal anti-inflammatory drugs, as some animal studies have shown that their use increases heart damage.
Most patients recover completely without evidence of residual cardiac dysfunction. Echocardiography allows accurate and noninvasive assessment of cardiac function, and, at least until cardiac function returns to normal, all patients should receive angiotensin-converting enzyme inhibitors.
With residual myocardial dysfunction, continuous treatment and specialist supervision is required, since in a small percentage of cases the disease recurs. Often the causative factor cannot be identified, but when it is known, it must be adequately addressed.
Rajesh K. Kharbanda , Fellow, British Heart Research Foundation Howerd Swanton , MD, Fellow, Middlesex Hospital