Sudden cardiac arrest during sleep in Russia causes from eight to sixteen deaths per every ten thousand population annually. The majority of people who experienced cardiac arrest suffered from mental disorders (45%), asthma (16%), heart disease (11%), and gastritis (8%). In some patients (22%), sudden death was the first manifestation of the disease.
Patients who suffer from cardiac arrest during sleep for a few seconds are also worried about lack of vigor, headache in the morning, decreased performance, snoring, increased irritability, unbalanced behavior, impotence and decreased libido, memory impairment. Such patients are more likely to have metabolic syndrome or atherosclerosis.
Causes of cardiac arrest
The causes of cardiac arrest at night during sleep are divided into direct cardiac and external. The main cardiac (cardiac) factors are increased blood pressure, atherosclerotic cardiosclerosis, myocardial ischemia and inflammation, acute vascular obstruction due to embolism or thrombosis, rhythm disturbances, and the development of cardiac tamponade.
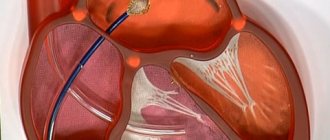
With cardiac tamponade, fluid accumulates between parts of the pericardium. The cavities of the heart are compressed, the muscle cannot contract normally. This condition directly threatens the patient’s life and requires urgent treatment. The pathology is characterized by the presence of complaints that patients usually present with heart failure.
Other causes of cardiac arrest during sleep include:
- loss of a significant volume of fluid due to ongoing diarrhea or vomiting, injury, shock;
- unilateral compression of one lung;
- the appearance of air between the layers of the pleura;
- oxygen deficiency caused by suffocation or anemia;
- severe allergies;
- hypothermia of the body (below 28 degrees);
- metabolic disorders or acute hypercalcemia.
In medical practice, hypercalcemia is a pathological increase in calcium levels in the blood. This occurs due to increased leaching of calcium from bone tissue, decreased absorption of calcium by bones, active absorption of the substance in the intestine, slow excretion from the body, or a combination of several factors. The clinical manifestations of this pathology are varied.
Heart rate in healthy men and women during night sleep
| Age | Men | Women |
| 18-50 years old | max heart rate - 75, min - 45 | max heart rate - 70, min - 40 |
| 51-80 years | max heart rate - 85, min - 50 | max heart rate - 80, min - 45 |
It should be added that the parasympathetic system gains the greatest “power” over the heart around 4 o’clock in the morning - it is at this time, in the deep sleep phase (stage 3), that the maximum slowdown in heart rate is normally observed.
Working at night or not getting enough quality sleep at night leads to an imbalance of the autonomic nervous system - its sympathetic department begins to predominate both day and night. The result is nocturnal tachycardia (an increase in heart rate beyond normal values), rapid depletion of the heart muscle and rhythm disturbances.
What happens during cardiac arrest
After sudden cardiac arrest during sleep, clinical death occurs in the second minute. Afterwards, the pupils dilate and do not react to the light source, and the skin quickly turns pale or acquires a pronounced bluish tint. These are the signs by which you can identify an extremely dangerous condition. In order for a person to survive, it is necessary to “start” the heart (perform an indirect massage) a maximum of five to seven minutes after stopping.
Diagnosis of sudden cardiac arrest
Cardiac arrest during sleep includes the initial symptoms of clinical death. With effective resuscitation, this phase is reversible. Therefore, resuscitation must begin as quickly as possible.
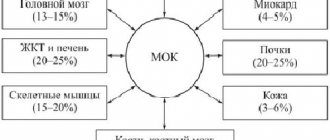
With complete loss of consciousness, the patient does not respond to braking or shouting. After the activity of the heart muscle stops, the brain dies on average within seven minutes, since it is the first to suffer from oxygen deficiency, and the stop of metabolic processes causes cell death.
During diagnosis, it becomes impossible to determine the pulse in the carotid artery, but this sign depends on the experience of others. If there is no pulsation in the carotid artery, then you can try to listen to the heartbeat by placing your ear to the victim’s chest. After making sure that the heart is not beating, you need to immediately begin resuscitation measures.
Other symptoms of cardiac arrest during sleep include dilation of the pupils, lack of reaction of the pupils to light, the appearance of individual seizures, and a change in skin color to pale or bluish. If an ambulance manages to arrive at the scene of the incident, then an electrocardiogram can confirm the simultaneous breathing disorder (in some cases, breathing does not stop completely, but is disrupted, which is accompanied by noisy breaths, the interval between which can be up to two minutes).
Can sleep apnea in adults be harmless?
Rare (less than 5 per hour) and short apneas (lasting less than 10 seconds) do not pose a threat to health.
If you notice any signs of sleep apnea, it is highly recommended that you consult a doctor. You (or your loved ones who notice the symptom) may think that apneas are rare and do not last long. But observations of the sleeping person are biased. Polysomnography will help identify the true number of pauses in breathing, determine an accurate diagnosis, and establish the causes and severity of the disorder. Perhaps this will help you avoid dangerous complications.
To make an appointment, call: 8 (495) 77-33-195 or leave your contacts in the form below.
If you have sleep apnea, make an appointment with a sleep specialist. Fill out the contact form and the administrator will call you back before the end of the working day to find a convenient time.
Signs of imminent cardiac arrest
Cardiac arrest during sleep is a sudden condition, but many patients noted the appearance of signs of the imminent onset of such a dangerous condition. 35% of patients had at least one sign indicating the presence of heart disease, Danish scientists say. In 17% of cases, a few hours before cardiac arrest, the person lost consciousness or felt chest pain (34%) - this is the most common symptom. Some patients experienced shortness of breath (29%).
According to the results of American studies, every second person who suffered sudden cardiac arrest during sleep experienced problems with the functioning of the heart muscle several weeks before the attack. Half of the men and more than half of the women reported chest pain or difficulty breathing four weeks before the attack. Almost all (93%) had the same symptom the day before cardiac arrest.
Treatment
To restart a stopped heart muscle in a medical facility, doctors use:
- Adrenalin;
- Norepinephrine;
- Atropine.
The listed drugs stimulate the activity of the heart. After the injection is administered, an electrocardiogram is taken. If necessary, the heart is started using a defibrillator, a device that creates an electrical shock. The device is already used in the intensive care unit to deliver the victim alive to the clinic .
Medicines for cardiac therapy
Patients are treated using the following medications:
- Ventricular extrasystole. What is it, treatment, what is dangerous, causes, ECG, drugs
- Adrenaline allows you to strengthen and accelerate the contraction of the heart muscle.
- Atropine is administered if asystole develops.
- Lidocaine suppresses arrhythmia.
- Sodium bicarbonate is infused if the heart has stopped for a long time, the activity of the organ has stopped due to acidosis or hyperkalemia.
- Magnesia helps stabilize and activate the heart muscle.
- Calcium eliminates hyperkalemia.
Proper use of medications allows for effective therapy. The chances of survival for a person whose heart has stopped in his sleep increase many times over.
Some patients require surgery. Patients have a pacemaker implanted into their heart muscle.
Rehabilitation period
When returning home, the patient must follow all medical recommendations:
- forget about bad habits;
- take medications prescribed by the doctor;
- undergo regular preventive examinations.
If the patient takes glycosides and leads a healthy lifestyle, relapse does not occur . A person has a chance to become a long-liver.
Consequences of cardiac arrest
The severity of the consequences depends on the speed and correctness of medical care. According to statistics, only one out of twenty people can be saved from death when the heart stops during sleep. Prolonged oxygen deficiency leads to the appearance of irreversible foci of ischemia in the brain, damage to the kidneys and liver. When carrying out resuscitation measures, fractures of the ribs, sternum, and accumulation of air or gases in the pleural cavity are possible.
Consequences from the brain can be partial or complete memory impairment, paroxysmal convulsions in the limbs, involuntary chewing movements, visual or auditory hallucinations, blindness accompanying irreversible changes in the optic nerves (while vision is restored in rare cases).
Stopping the activity of the heart muscle is not only provoked by cardiac diseases, but can also become a significant risk factor for the development of other pathologies.
The most common diseases of the cardiovascular system:
- Hypertension
(high blood pressure): Places additional stress on the heart and damages blood vessels.
During sleep, your blood pressure usually drops by about 10-20%. When you stop breathing, your oxygen levels drop. The brain's response to lack of oxygen is to release adrenaline as well as constrict blood vessels to increase the flow of oxygen to vital organs such as the heart and brain, leading to increased blood pressure. That is, sleep apnea causes a constant jump in high blood pressure, increasing it by 10-20% above normal. A constant surge of high blood pressure can continue during waking hours, leading to the development of hypertension.
That is, when the force of blood flowing through the vessels is constantly too high, the circulatory system can become damaged, which can lead to a heart attack, stroke….
- Arrhythmia
(heart rhythm disorder) – the heart beats irregularly or differently than normal:
Obstructive sleep apnea can contribute to arrhythmias due to:
- repeated episodes of oxygen starvation (hypoxia);
- increased levels of carbon dioxide in the blood (hypercapnia);
- direct effects on the heart due to changes in chest pressure.
- Stroke
– vascular diseases of the brain:
It is the second leading cause of death worldwide. It is also a leading cause of long-term disability. Insufficient sleep caused by obstructive sleep apnea is significantly associated with stroke risk, even in the absence of other risk factors, including age, gender, race, smoking status, alcohol use, diabetes, or hypertension.
The more severe the symptoms of OSA, the higher the risk of stroke, particularly in middle-aged and older people, and especially in men. Scientists speculate that the difference in risk between men and women may be due to the fact that men are more likely to develop sleep apnea at a younger age and therefore go untreated for OSA for a longer period of time than women.
Prevention of the syndrome
You can prevent cardiac arrest during sleep by avoiding negative provoking factors that affect blood circulation. For people with heart disease, no less important than regularly taking cardiac pills are regular walks in the fresh air, drinking enough clean water, giving up alcohol and smoking, and a balanced diet.
The use of drugs to normalize heart rhythm is possible only under pulse control. We must also remember about a possible overdose. The patient should learn to independently determine and count the pulse; it is important to follow the doctor’s recommendations regarding the dosage and duration of taking medications.
Unfortunately, the decisive factor in sudden cardiac arrest during sleep is the speed of first aid. But it has not yet been possible to achieve complete and effective resuscitation measures at home.
Signs of cardiac apnea
With this disease, patients experience various symptoms. The frequently recurring signs of chronic insufficiency (weakness, swelling, palpitations, chronic dry cough, shortness of breath) are accompanied by other problems.
How to treat cardiac apnea? Monitoring, CPAP therapy
All of the listed negative additions to heart disease, which manifest themselves in breathing disorder at night, require diagnosis and special help. Without special therapy, returning to normal sleep is almost impossible.
A healthy heart requires a diet, establishing the patient’s normal weight, and feasible exercise. One of the important conditions for effective heart treatment is adequate and complete sleep.
It is equally important to monitor patients with HF to identify the type of apnea. If patients with OSA are most often overweight, then with central apnea patients are usually thin. In addition, they may not suffer from snoring.
An effective diagnostic test among modern technologies is polysomnography. After its results, the doctor selects an appropriate treatment method taking into account heart failure.
Today, many people are prescribed CPAP therapy, the benefits of which have been proven by several serious studies and practice. Patients' functional capabilities improved significantly, their quality of life increased, and heart failure was much more easily controlled.
Remember that timely treatment of sleep disorders will improve heart function. Therefore, at the slightest suspicion of cardiac apnea, do not put off visiting a doctor and do not self-medicate!
Source