In practice, the New York Heart Association (NYHA) classification is often used to assess the severity of heart failure:
I class
— Physical activity is not limited
Class II
— Mild limitation of activity.
The appearance of shortness of breath and weakness after moderate physical activity. Class III
- Marked limitation of activity.
Shortness of breath after minimal physical activity Class IV
- Severe limitation of activity. Symptoms of heart failure at rest
Principles of drug treatment of heart failure
Treatment of heart failure should be aimed at achieving the following goals:
- Identification and treatment of the underlying disease that led to the development of heart failure. For example, in some cases, intensive antihypertensive therapy, valve replacement, or complete cessation of alcohol consumption, etc. may be required.
- Treatment of decompensated heart failure:
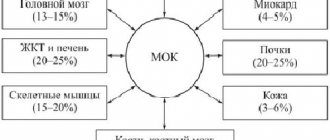
- Reducing blood stagnation: (limiting salt intake, limiting fluid intake, drug therapy (diuretics) aimed at removing excess water and sodium from the body.
- Increased cardiac output and improved blood supply to vital organs. For this purpose, inotropic drugs are used, which increase the contractility of the heart muscle, as well as various vasodilators.
Elimination of factors that provoke the development of decompensation in patients with compensated heart failure (for example, adequate treatment of arrhythmias, limiting fluid intake or salt intake).
Medical Internet conferences
Marfan syndrome (MS) is an autosomal dominant disorder, the prevalence of which in the European population ranges from 1:10,000–1:20,000 to 1:5,000 people [,2]. Diagnosis of the syndrome is based on the patient’s appearance and the results of morphometry. The disease is often associated with arachnodactyly, lens subluxation, and aortic aneurysm []. However, most patients have erased forms that do not have the classic triad of signs. Erased forms of SM are explained by the multiplicity of molecular mechanisms of pathogenesis and heterozygosity [4].
Signs of the disease appear from the moment the child is born. During the newborn period, skeletal abnormalities are detected in the form of elongation of the limbs, a narrow facial skull, and sometimes in the form of deformation of the chest. Manifestations of Marfan syndrome become more obvious with age.
Cardiovascular manifestations in SM are quite common and include: mitral valve (MV) prolapse, aortic root dilatation, aortic regurgitation, cardiac arrhythmias, etc. Other cardiovascular manifestations in young children include aortic coarctation, atrial defect septum (ASD), patent ductus arteriosus (PDA), pulmonary stenosis, etc. The aorta is the main point of attack. In particular, the aortic root is susceptible to dilatation, aneurysm formation, and dissection []. Aortic root enlargement occurs in 60% of patients with SM, while MV prolapse occurs in 91% [].
Cardiovascular changes often determine the prognosis of patients' lives: in 90% of cases, patients die before they reach 40–50 years of age as a result of aortic dissection and rupture, progressive heart failure resulting from aortic valve (AV) and MV insufficiency [].
Disturbances in MV function in SM occur as a result of elongation of the valve chords and dilatation of the ring. Structural disorders are accompanied by prolapse of the MV valves and mitral insufficiency. MV prolapse is diagnosed when late systolic sagging of the leaflet is 2 mm or more during ultrasound examination of the heart in M-mode. In 25% of patients, progression of prolapse of the mitral valves is observed, as a result of which mitral regurgitation develops, accompanied by an increase in the size of the cavity of the left atrium and ventricle. Calcification of the valve ring is often detected in people under 40 years of age. Dilation of the left ventricle due to the formation of mitral regurgitation progresses over time and is accompanied by the development of signs of chronic heart failure (CHF).
In addition to prolapse of the MV valves in SM, there is an expansion of the initial part of the pulmonary trunk. Changes occur in childhood or adolescence, with no basis or signs of stenosis of the pulmonary artery orifice or its subvalvular space.
Changes in the aorta in the form of dilatation at its different levels are formed in utero or in the postnatal period. Dilation of the aortic root is diagnosed based on the results of ultrasound examination: dilation is determined in cases where the size of the aorta at the level of the sinus of Valsalva exceeds normal values for a specific age and body surface area. In addition to ultrasound, methods of contrasting the aorta, computer and magnetic resonance imaging are used.
Dilatation of the aortic root causes the most serious complications. Aortic insufficiency appears, an aneurysm of the ascending aorta is formed, complicated by its rupture. The risk of rupture of the ascending aorta increases if its internal diameter at the level of the sinus of Valsalva is more than 5.5 cm. An aneurysm of the ascending aorta is represented by a dissecting vessel wall or a saccular form. A saccular aneurysm involving the ascending aorta and sinuses of Valsalva ruptures more often than a dissecting aneurysm. At the same time, a dissecting aortic root is also accompanied by severe complications: occlusion of the coronary arteries and myocardial infarction occurs [8].
Organic and functional changes in the heart that occur in Marfan syndrome are often accompanied by cardiac arrhythmias (supraventricular and ventricular tachycardia, atrial fibrillation, QT prolongation), the development of infective endocarditis, and sudden cardiac death (SCD) [9, 10].
If SM is diagnosed, patients are advised to limit physical activity to a moderate or low level. Patients should be observed by various specialists, including a cardiologist, ophthalmologist, orthopedic traumatologist, clinical geneticist, etc., since multidisciplinary problems arise.
Changes in the cardiovascular system are an indication for medical and surgical treatment of these patients. Pharmacological treatment includes the use of beta-blockers to reduce the speed of propagation of the pulse wave with progressive dilatation of the aorta and regurgitation of the mitral or aortic valve of the heart. The use of Ca++ channel blockers is possible in cases where the use of β-blockers is limited.
Surgical treatment is used for heart valve insufficiency, prolapse of the mitral valve leaflets, significant (more than 55 mm) expansion of the ascending aorta and its dissection. Prophylactic aortic root replacement is recommended if:
- aortic root diameter ≥ 55 mm;
- positive family history of aortic dissection and aortic root diameter ≥ 50 mm;
- aortic root growth ≥ 2 mm/year.
Clinical case
Patient S., 29 years old, was admitted with complaints of: shortness of breath with minimal physical and emotional stress, sometimes at rest; swelling of the lower extremities; episodes of rapid, irregular heartbeat; to increased fatigue, severe general weakness.
Since childhood, Marfan syndrome and MV prolapse have been diagnosed. I was seen regularly by a cardiologist. The condition worsened at the end of 2001, when severe shortness of breath, swelling of the legs, and ascites appeared. The examination revealed cardiomegaly (CTI=71%) with a decrease in myocardial contractility (LVEF up to 45%). In February 2002, at the Scientific Center for Agricultural Sciences named after. A. N. Bakulev of the Russian Academy of Medical Sciences performed an operation: replacement of the mitral valve with the Medinge prosthesis No. 31 with preservation of the subvalvular structures of the posterior and partially anterior mitral leaflet, creation of neochordas, plastic repair of the valve according to de Vega under infrared conditions. He was discharged on the 20th day after surgery. He took the prescribed therapy regularly and underwent outpatient examinations as planned. LVEF remained at the level of 49-51%. During the next examination at the end of 2007, an aneurysm of the ascending aorta was detected. In October 2007, the Bentall-De Bono operation was performed using a synthetic valve-containing Meding conduit No. 25. He was discharged on the 15th day in satisfactory condition. He underwent regular outpatient examinations and took prescribed therapy regularly. The deterioration of health occurred in 2011, when signs of decompensation appeared in the systemic circulation. Since the summer of 2012, he has noticed a gradual significant deterioration: shortness of breath has become constant, severe swelling of the legs, cardiac arrhythmias, in the form of atrial fibrillation, have appeared.
Objectively
The general condition is moderate. The severity of the condition is due to heart failure in the compensation stage. Consciousness is clear, behavior is adequate, emotionally stable. Activity is limited by the functional class of CHF. Constitutional features of asthenics. Height 197 (cm), weight 82 (kg), BSA = 2.14, BMI = 584.23. Body mass index = 21.13. The head is dolichocephalic in shape, the face is narrow, elongated, micro- and retrognathia, high arched palate, skin hyperextensibility, decreased tissue turgor. Positive wrist and thumb tests, scoliosis, kyphosis, pectus excavatum, arachnodactyly, pes planovalgus. The skin is pale, there are multiple small nevi and hemangiomas on the skin of the face, trunk, upper and lower extremities. The subcutaneous fat layer is thinned. The chest is of the correct shape. Respiratory rate 14/min. Breathing is harsh, carried out in all departments. No wheezing. Percussion data: pulmonary sound in all fields. Auscultation data: hard breathing in all fields. Heart sounds are muffled and arrhythmic. The boundaries of relative cardiac dullness are shifted to the left due to chest deformation and cardiomegaly. The abdomen is soft and painless on palpation. The liver is 1.5 cm below the right edge of the costal arch. Heart rate = 80 beats/min. Blood pressure: on the left arm - 90/60 mm Hg. The liver is not enlarged. The spleen is not palpable. The abdomen is soft, painless in all parts on superficial palpation. The stool is regular and formed. Urination is free and painless. Diuresis is sufficient despite the constant intake of saluretics. Pasternatsky's symptom is negative on both sides.
Laboratory research methods
ECG: Rhythm atrial fibrillation with a ventricular rate of 82 beats per minute. Left bundle branch block. QRS = 190ms. Chest X-ray: in direct projection, no fresh focal and infiltrative changes are noted. The lungs are emphysematous. The pulmonary pattern is enhanced. The roots of the lungs are displaced and compacted. The sinuses are differentiated. The right dome of the diaphragm is partially relaxed. The mediastinum is displaced. The heart shadow is expanded in diameter. Two artificial valves are identified.
EchoCG: Left atrium: parasternal access - 5.7 cm; apical - 9.0x8.5. V-370ml. Left ventricle: according to Simpson: KDO-684ml; KSO-558ml; UO-127ml; FV-18-19%; according to Teincholz: KSR-8.8 cm; KDR-9.7cm; KDO-526ml; UO-97ml; FV-18%. Mitral valve: prosthesis, movement of the elements, preserved subvalvular structures of the PVJ. Peak gradient = 9 mm. Hg Art. Mid-diastolic gradient = 3.8 mm. Hg Art. Aorta: ascending-36mm. Aortic valve: prosthesis, movement of disc electric valves. Peak gradient = 12mmHg, mean = 5mm. Hg Art. RA and RV: the electrodes are pushed aside by the dilated left ones, echo signal from the pacemaker. Pulmonary artery: trunk-29mm. Peak gradient - 0.8 mmHg Regurgitation - 1.5 degrees. Tricuspid valve: cusps are movable. Peak hail is 1.5 mm. Hg Art. The degree of regurgitation is 1.5. Akinesis of the IVS with thinning, pronounced diffuse hypokinesis. There is no liquid in the p/n. In the left chambers there is a pronounced effect of spontaneous contrast.
EchoCG for dyssynchrony (09.11.12) APE - 148 (163), PPE - 163 (162), IVMD inter (>40mc) - 20 - 40, IVRT - 89, IVMD intra (>130mc) - 170 - 210, LLA - 55, EDV - 520 ml, ESR - 429 ml, PV - 16 -18%. Conclusion: signs of intraventricular dyssynchrony (transverse in all segments). No signs of interventricular dyssynchrony were detected.
Based on the medical history and the results of instrumental studies, a clinical diagnosis was made: Marfan syndrome. Condition after mitral valve replacement (Meding prosthesis No. 31), with preservation of the subvalvular structures of the posterior and partially anterior mitral leaflet, creation of neochordas, de Vega repair of the ventral valve under infrared conditions from 02/14/2002. Condition after the Bentall - De Bono operation with a synthetic valve-containing conduit Medinge No. 25 under IR conditions from 10/16/2007. Secondary cardiomyopathy. Low cardiac output syndrome. Heart rhythm disturbance: permanent form of atrial fibrillation. Complete block of the left bundle branch. CHF IIB, FC III-IV
Considering the presence of dyssynchrony, low LVEF, as well as in order to prevent possible fatal cardiac arrhythmias, the patient was decided to undergo cardiac resynchronization therapy [11-14].
Operation
Under local anesthesia Sol.Novocaini - 0.5% - 60 ml, a 5cm incision was made in the left subclavian region. The left subclavian vein was punctured twice. Using an introducer, a 10-pole BW Webster electrode was inserted into the heart cavity. Next, the Biotronic ScoutPro 7F introducer was passed along the electrode into the CS. Contrast of the CS was performed using BRAUN Corodyn P2 7F, then using the Coronary Guide Wire Galeo Hydro ES 014, a left ventricular electrode Guidant EASYTRAK 2 was passed and installed in the lateral vein of the LV. The right ventricular defibrillation electrode Biotronic Linox SD 6516 is installed in the apex of the pancreas.
The electrode parameters were:
| RV electrode | LV electrode | |
| Sensitivity, mV | >25 | 12,5 |
| Stimulation threshold, V | 0,4 | 1,8 |
| Pulse duration, ms | 0,5 | 0,5 |
| Resistance, Ohm. | 645 | 925. |
Shock 51 Ohm.
Fixation of electrodes. Re-measurement of parameters. Creation of a subcutaneous bed for BVS-KVDF. Implantation into the created BVS-KVDF bed from GUIDANT CONTAK RENEWAL 4 REF: H190 SNo. 318346. Suturing of the BVS-KVDF bed. Layer-by-layer suturing of the wound. Interrupted sutures on the skin. Alcohol. Aseptic dressing.
Stimulation parameters: Stimulation mode – VVIR, Lower stimulation limit – 80, Upper stimulation limit 120, VV delay – 0ms.
| pancreas | LV | |
| Sensitivity, mV | Std. | Std. |
| Amplitude, V | 3,0 | 3,0 |
| Pulse duration, ms | 0,5 | 0,5 |
| Polarity (stim./feelings) | bi/bi | LVtip-RVcoil/- |
VF 300ms/200 beats - 31J shock.
The postoperative period was without complications. Due to the persistent tachysystolic form of atrial fibrillation, after 1.5 months the patient underwent radiofrequency ablation of the AV nodal conduction. With further observation of the patient, an improvement in the condition is noted.
Rice. 1. A. Contrast of the coronary sinus. A right ventricular defibrillation electrode Biotronic Linox SD 6516 was implanted into the apex of the pancreas. Left ventricular electrode Guidant EASYTRAK 2.
Hypoxemic crisis (dyspnea-cyanotic attack)
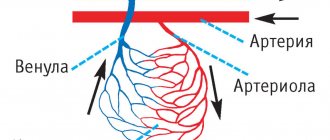
A shortness of breath-cyanotic attack is an attack of hypoxia (paroxysmal shortness of breath with severe cyanosis) in a child with blue-type congenital heart disease, most often with tetralogy of Fallot. It occurs as a result of a sudden decrease in pulmonary blood flow associated with spasm of the outflow tract of the right ventricle of the heart, an increase in blood discharge from right to left and hypoxemia in the systemic circulation.
Attacks of hypoxia develop mainly in young children - from 4–6 months to 3 years. Provoking factors for a dyspnea-cyanotic attack can be psycho-emotional stress, increased physical activity, intercurrent diseases accompanied by dehydration (fever, diarrhea), iron deficiency anemia, neuro-reflex excitability syndrome with perinatal damage to the central nervous system, etc.
A dyspnea-cyanotic attack is characterized by a sudden onset. The child becomes restless, moans, cries, and cyanosis and shortness of breath increase. Takes a forced position - lies on its side with its legs brought to the stomach or squats. On auscultation of the heart there is tachycardia, a decrease in intensity or disappearance of systolic murmur over the pulmonary artery. The duration of a hypoxic attack ranges from several minutes to several hours. In severe cases, hypoxemia, acidosis, convulsions, loss of consciousness, even coma, and death are possible.