Not everyone knows what heart failure is. This disease is a condition caused by a decrease in the contractility of the heart muscle. Another reason is stagnation of blood circulation in the small or large circle. Manifestations of the disease can be very diverse. Concern should be caused by shortness of breath, which manifests itself even with minor physical exertion or when a person is at rest. Symptoms include fatigue, a bluish tint to the nails, and the tip of the nose.
What is heart failure
There is an acute and chronic form of the disease. Acute is very dangerous because pulmonary edema and also cardiogenic shock can develop. Chronic causes hypoxia of various organs to develop over time. Heart failure kills many people every year and is considered one of the most common causes of death.
Once the pumping function of the heart is reduced in the case of heart failure, there is a difference between the body's need for blood supply and the fact that the heart cannot provide it. This difference is expressed in the fact that venous inflow increases. The resistance that the heart muscle must overcome in order to direct blood into the vascular bed increases.
Heart failure is not considered an independent disease. It is a consequence of various lesions of the heart and blood vessels. These include ischemia, arterial hypertension, valve defects, etc.
There are diseases, including, in particular, arterial hypertension, in which signs of heart failure in women and men increase gradually. This can happen over several years. In other diseases, for example, acute heart attack, in which some of the working cells die, this happens quite quickly. This period ranges from several days to several hours. If heart failure develops very quickly, its acute form is present; if it develops slowly, it is chronic.
What chronic heart failure is is known to 0.5-2 percent of all people from their own experience. After age 75, the incidence rises to 10 percent. The problem of prevention and treatment of this disease is very important, because the number of patients is constantly increasing. In addition, the disease often leads to disability and death.
About the structure of the cardiovascular system
The heart is a unique organ on which human life depends. It works without rest, has its own control center, which sends electrical impulses that stimulate muscle contractility.
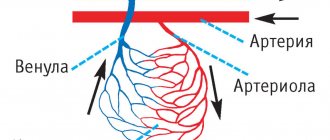
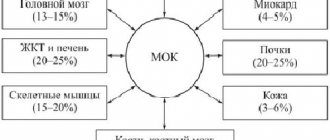
The structure of the heart is widely known: it has two ventricles and two atria. By contracting, they ensure blood circulation through two vascular systems: the small and large blood circles. To more accurately explain the characteristics of different types of heart failure, it is necessary to mention the characteristics of blood flow.
The systemic circulation involves the flow of blood from the left ventricle into the aorta, oxygenation of all important organs and limbs and the return of venous blood to the right atrium. The pulmonary circulation is the flow of blood from the right ventricle to the lungs and the movement of oxygenated blood into the left atrium.
Symptoms of heart failure depend on which part of the heart is affected. This is reflected in disruption of the functioning of blood circulation.
Heart failure, depending on the nature of its course, can be of two types. The chronic form develops over a long period of time and has several stages. Acute heart failure progresses rapidly. The duration of the process is from an hour to two days. This condition requires urgent hospitalization.
The classification of heart failure based on the localization of the pathology distinguishes several types:
- Left ventricular failure;
- Right ventricular failure
- Total form.
As the disease progresses, isolated variants lead to the formation of a general, total form of the lesion. Damage to the left ventricle causes disturbances in the systemic circulation. Pathology of the right ventricle - affects the lungs or pulmonary circulation.
Causes of the disease
In two thirds of all people with heart failure, the cause of the disease is myocardial infarction and ischemia. 14 percent of cases are caused by heart defects, 11 by dilated cardiomyopathy.
Among people over 60 years of age, four percent of cases are caused by hypertension. In elderly patients, a common cause is type 2 diabetes, especially if arterial hypertension is present at the same time. How heart failure is treated depends on the specific cause.
There are several factors that contribute to the formation of the disease. It usually manifests itself if there is a decrease in the compensatory mechanisms of the heart. These factors differ from the causes in their reversibility. If they are eliminated or even reduced, the development of the disease can be stopped. There are cases when this leads to saving the patient’s life.
Such factors include intense physical activity and stressful situations. Among them are pulmonary embolism, arrhythmia, and progressive ischemic disease. Factors include pneumonia, acute respiratory viral infections, and kidney failure. Negative consequences are caused by taking cardiotoxic drugs, as well as medications that retain fluid in the body and increase blood pressure. Addiction to alcohol and sudden weight gain have a negative effect. Predisposing factors are myocarditis, rheumatism, as well as neglect of the recommendations of a treatment specialist.
Causes of the disease
The causes of congestive heart failure are pathologies of the cardiovascular and endocrine systems. They can be congenital or acquired:
- genetic predisposition;
- ischemic disease.
- myocarditis
- diseases resulting in thickening of the walls of the myocardium and pericardium;
- thyroid diseases;
- diabetes.
Factors that provoke the occurrence of pathological processes include:
- bad habits, smoking and alcoholism;
- sedentary lifestyle;
- excessive body weight;
- severe infections (usually viral);
- heavy physical activity;
- frequent stress, improper daily routine, lack of sleep.
Congestive heart failure is more common in old age, occurring in 10% of people after sixty years of age. However, the disease also affects young people. In adolescence, it is necessary to carefully monitor the state of the cardiovascular system. The rapid growth of bone and muscle tissue, hormonal changes increase the load on the heart, which does not have time to grow with such rapid growth of the body as a whole.
Young athletes are at risk. Typically, training for teenagers is more gentle; children undergo annual examinations. If signs of congestive heart failure are detected, not only urgent treatment is necessary, but also a temporary refusal to exercise. Doctors recommend taking a break for about a year.
How does heart failure develop?
The acute form of heart failure is often formed on the basis of a heart attack. Its appearance is caused by acute myocarditis and serious arrhythmias. With these diseases, the minute output is reduced quite sharply, as a result of which much less blood enters the arteries. This form, in its clinical manifestations, resembles acute vascular insufficiency. Therefore, in some cases, such phenomena are referred to as acute cardiac collapse.
In the case of a chronic form of heart failure, the pathological processes that form in the heart are balanced for quite a long time by its increased work. At the same time, adaptive mechanisms of the cardiovascular system operate. The rhythm becomes more frequent, the force of contractions increases. Due to the dilation of blood vessels, the pressure in diastole decreases.
With the subsequent development of manifestations of heart failure, a decrease in cardiac output occurs. There is more blood in the ventricles. When the heart muscles relax, they become overfilled. The myocardium is constantly in a tense state, as it strives to maintain normal blood circulation and direct it into the vascular bed. As a result, compensatory hypertrophy of this cardiac muscle occurs. But time comes and the myocardium weakens, which leads to decompensation. As a result, a process of dystrophy develops in the heart muscle, and it itself begins to experience a lack of blood supply and energy.
At this stage, neurohumoral regulation is involved in this process. This phenomenon leads to narrowing of peripheral blood vessels. As a result, cardiac output becomes smaller, and blood pressure in the systemic circle remains at the same level. In the kidneys, a narrowing of the lumen of blood vessels occurs, which, in turn, causes ischemia of this organ. As a result, fluid is retained inside the tissues.
The pituitary gland produces more antidiuretic hormone. The consequence of this is increased fluid absorption. As a result, the amount of circulating blood becomes greater, and the pressure in the veins and capillaries increases. Transudation increases.
Thus, heart failure causes serious hemodynamic damage to the body:
Disturbance of gas exchange.
When blood circulation slows down, the tissue begins to absorb more air from the capillaries. If usually this figure is 30 percent, then in this case it increases to 70. As a result, acidosis is formed. Due to the fact that the respiratory system begins to function more strongly, the basal metabolism is activated. As a result, movement occurs in a vicious circle. The human body requires more and more oxygen, but the circulatory system cannot provide it.
This phenomenon is called oxygen debt. Its development leads to shortness of breath and cyanosis. The latter comes in two types: central or peripheral. The central one is formed during stagnation in the small circle. Peripheral - a consequence of slowing blood circulation. Due to the fact that the lack of blood circulation is more noticeable in peripheral places, patients develop blueness of the arms and legs, the tip of the nose, and ears.
Edema.
The phenomenon of edema appears due to several circumstances. Among them are an increase in capillary pressure and a slowdown in blood circulation. If there is a disorder of water-salt balance, fluid and sodium are retained. If protein metabolism is incorrect, blood plasma pressure is disrupted. If liver function is reduced, there is a loss of activity of certain hormones, in particular aldosterone.
At first, the swelling occurs secretly. Its presence can be guessed by weight gain, while at the same time less urine is produced. First, it becomes noticeable that the legs swell when a person walks. If it is in a horizontal position, the sacrum swells. The disease progresses, after some time cavitary dropsy appears. Fluid accumulates in the abdominal, pleural, and pericardial cavities.
Stagnation in organs.
This phenomenon in the lungs is caused by a disruption in the movement of blood through the vessels of the small circle. At the same time, muscle tone increases, the difference between the volume of the chest at maximum inspiration and the same exhalation decreases. The mobility of the edges of the lungs becomes lower. Manifestations of the disease in patients are coughing up blood, congestive bronchitis, and pneumosclerosis.
Stagnation in the large circle leads to a strong increase in liver volume. This is expressed in the fact that a person experiences heaviness and pain under the right rib. After this, cardiac fibrosis of this organ occurs, connective tissue is formed in it.
If, during heart failure, the cavities of the heart expand, this may result in damage to the atrioventricular valves. The patient experiences swelling of the neck veins, tachycardia, etc.
If stagnant gastritis is observed, a person suffers from the fact that he begins to feel sick, vomit, loses his appetite, and begins to lose weight. As the deficiency progresses, the patient becomes severely exhausted. This condition is called cardiac cachexia.
Stagnation in the kidneys leads to the fact that they begin to separate very little urine, the density of the latter increases, protein and blood appear in it. Damage to the central nervous system in case of insufficiency is expressed in the fact that the patient quickly gets tired, his activity decreases, both physical and mental, he sleeps poorly, and he develops depression.
Sudden cardiac death and its prevention
Coronary death
Coronary death refers to death that occurs as a result of the cessation of effective heart function. As a rule, in this case, either ventricular fibrillation or primary cardiac arrest develops. In almost 90% of cases, acute coronary death is caused by coronary heart disease. It also happens that before this, IHD did not manifest itself in any way, that is, it was asymptomatic. In some cases, the patient was bothered by angina attacks and arrhythmia. After a heart attack, the risk of sudden death increases several times.
Manifestations and course of coronary death
Autopsies of patients who died suddenly usually reveal damage to the coronary arteries by atherosclerotic plaques. In this case, the lumen of the vessel narrows by 70% or more. Very often, on the damaged surface of the vessel there is a thrombus that has completely stopped blood flow in a fairly large area of the heart muscle. Usually, signs of myocardial infarction cannot be identified, since too little time has passed since the onset of the disease. Histological examination can reveal signs of incipient necrosis and cell restructuring.
Due to electrical instability of the myocardium, life-threatening arrhythmia occurs (asystole or ventricular fibrillation). Blood flow stops, including through the cerebral arteries. In this regard, the person quickly loses consciousness and falls. Noisy wheezing breathing and foam at the mouth may appear. After a few minutes, the muscles will begin to twitch involuntarily. The skin becomes pale, cyanosis of the lips and limbs is observed. The pulse and breathing stop completely, the pupils dilate and stop responding to light.
Help with cardiac death
Sudden coronary death leads to irreversible changes in the cerebral cortex within 5-6 minutes. Therefore, emergency measures to restore blood flow must begin immediately and continue until the arrival of the medical team.
Every person needs to know the basics of cardiopulmonary resuscitation. Her tasks include checking and, if necessary, restoring the patency of the airways, starting artificial ventilation (mouth-to-mouth, mouth-to-nose), and chest compressions. According to the latest recommendations, a person without experience can skip the first two points and immediately begin cardiac massage. Several studies have shown that this approach is more effective and leads to improved survival.
Indirect cardiac massage should be performed as follows:
- Place the person on their back on a hard surface;
- Place your palms on the middle third of the sternum perpendicular to it;
- Start squeezing your chest without bending your elbows;
- In this case, the sternum should bend by 5 cm, and the frequency of movements should be about 100 per minute.
The effectiveness of resuscitation measures can be judged by the color of the skin.
Prevention of sudden coronary death
To prevent cardiac death, it is necessary to influence the main provoking factors, among which the most important are:
- Myocardial ischemia;
- Decrease in left ventricular ejection fraction;
- Various arrhythmias.
To eliminate oxygen starvation of the heart, adequate drug therapy is necessary, including the main classes of drugs to improve coronary blood flow (nitroglycerin, beta blockers, aspirin, statins).
If necessary, endovascular restoration of artery patency should be performed. A special balloon is inserted into the affected area through a puncture in the femoral artery, inflated, and then a spring (stent) is installed, which prevents further narrowing of the vessel.
If such an operation cannot be performed for any reason, coronary artery bypass grafting is performed with opening of the chest and connection to a heart-lung machine. In this case, additional vessels (the person’s own arteries and veins, taken from an arm or leg) are sewn from the aorta to the coronary arteries. Recovery after this operation is longer, but the prognosis is favorable.
If myocardial contractility decreases, special devices can be installed to increase it. Special medications, such as digoxin, are also prescribed.
To prevent arrhythmia, in particular ventricular fibrillation, a cardioverter-defibrillator is installed. It is a miniature device that is placed under the skin in the chest area. Using special wires, it is connected to the myocardium and, if an arrhythmia occurs, it restarts the heart using a discharge. It should be remembered that with asystole this device will be ineffective.
Unfortunately, coronary death is a rather insidious disease, and it is not always possible to identify potential patients. That is why the most important thing in the fight against this condition is the timely implementation of emergency measures. Nowadays, many public places have defibrillators that can be used for life-threatening arrhythmias. They also often conduct special courses on teaching resuscitation measures to ordinary citizens.
RISK FACTORS FOR SUDDEN DEATH
Sudden cessation of blood circulation (“cardiac arrest”, clinical death) occurs most often as a result of diseases of the cardiovascular system. The cessation of blood circulation leads to the death of cells in the cerebral cortex, which cannot exist without a constant supply of oxygen for more than 5 minutes. The time frame originally used to describe sudden death was 24 hours. Now they have been reduced to 1 hour.
The risk factors for sudden death are essentially the same as for coronary heart disease.
1. Arterial hypertension and left ventricular hypertrophy
First of all, left ventricular hypertrophy. The risk of sudden death increases with increasing myocardial mass.
2. Lipids
The connection between high cholesterol levels and the risk of sudden death is well established and proven, although there is no reliable data on reducing this risk when lipid levels are normalized.
3. Nutritional features
Most epidemiological studies have not found a clear association between the risk of sudden death and any dietary characteristics.
4. Physical activity
The risk of sudden death is higher both in people who do not regularly engage in strenuous exercise and in people with a lack of physical activity.
5. Alcohol addiction
Severe alcohol dependence and especially binge drinking increase the risk of sudden death. However, moderate alcohol consumption reduces the risk of sudden death (30 g of ethanol per day).
6. Heart rate and heart rate variability
An increase in heart rate is an independent risk factor for sudden death. This may be due to a decrease in parasympathetic activity. Heart rate variability is an indicator associated not only with cardiac, but also with non-cardiac causes of death, so its relationship with the risk of sudden death cannot currently be assessed.
7. Smoking
Smoking is an independent risk factor for sudden clinical death and for the development of myocardial infarction. For persons with a history of circulatory arrest, continued smoking after discharge from hospital is also an independent risk factor for repeated sudden circulatory arrest.
8. Diabetes mellitus
To date, there is no convincing evidence that diabetes mellitus is an independent risk factor for sudden death.
9. Changes on the ECG
A large number of studies have noted a clear connection between ECG changes such as ST segment depression and T wave changes with cardiac death in general and sudden death in particular. Prolongation of the QT interval in individuals without heart disease is also an unfavorable prognostic factor for the development of cardiac death. Similar facts have not been proven regarding QT interval dispersion.
10. Genetic basis
Long QT syndrome, hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy, polymorphic ventricular tachycardia, dilated cardiomyopathy are inherited in a monogenic manner and have a clear predisposition to sudden death.
The cause of sudden death is often ventricular fibrillation (VF) 75-80% and ventricular tachycardia (VT), less often electromechanical dissociation (EMD) and asystole. Circulatory arrest usually occurs at home (2/3 of cases), in men over 50 years of age (3/4 of cases) during the day (8-18 hours).
All risk factors for coronary heart disease
Since in most cases sudden cardiac death is caused by ischemic disease, it is clear that almost all risk factors for coronary heart disease are also risk factors for sudden death. The greatest importance belongs to such factors as old age, arterial hypertension, left ventricular hypertrophy, tobacco smoking, high blood cholesterol, excess body weight, nonspecific electrocardiographic changes. The risk of sudden cardiac death increases especially significantly when several risk factors are combined.
Previous myocardial infarction
Myocardial infarction is an important risk factor for sudden cardiac death. The potential risk of sudden cardiac death in the first 72 hours from the onset of a heart attack ranges from 15 to 20% of cases. The highest risk of sudden cardiac death is observed in patients with myocardial infarction between 3 days and 8 weeks if the course of the disease was complicated by ventricular tachycardia or atrial fibrillation, or if paired, salvo, early ventricular extrasystoles, or repeated episodes of salvo ventricular extrasystoles were recorded. When heart rate is normalized and left ventricular dysfunction is eliminated, the risk of sudden death is sharply reduced.
An unfavorable prognostic factor in the post-infarction period is depression of the ST interval (painless or accompanied by pain) during exercise testing. The combination of subtotal stenosis of one or more coronary arteries, areas of left ventricular dyskinesia (detected by echocardiography) and frequent polytopic ventricular extrasystoles has a poor prognostic value. The risk of sudden death is significantly increased by the presence of a left ventricular aneurysm, its pronounced hypertrophy, as well as ventricular fibrillation that occurred in the acute period of myocardial infarction and was successfully stopped.
Left ventricular myocardial dysfunction
A decrease in the contractile function of the left ventricular myocardium is one of the main risk factors for sudden cardiac death in cardiac patients. A reduction in ejection fraction of less than 40% is considered critical. After the onset of congestive heart failure of various origins, the risk of sudden cardiac death is very high, it can be 35-40% within 5 years.
Left ventricular myocardial hypertrophy
Left ventricular myocardial hypertrophy of any origin significantly predisposes to sudden cardiac death, with fatal arrhythmia being the most common mechanism of death. This is explained by the fact that with myocardial hypertrophy, the kinetics of ions in it is disrupted, there is a pronounced heterogeneity in the medium of propagation of depolarization and repolarization waves in the myocardium, which contributes to the development of ventricular fibrillation and flutter.
“Unreasonable” decrease in exercise tolerance
Usually, the basis for an unreasonable decrease in exercise tolerance is myocardial ischemia, which is also often combined with cardiac arrhythmias. These factors significantly increase the risk of sudden cardiac death.
Previous sudden cardiac death and previous resuscitation
In patients who have survived sudden cardiac death, the risk of recurrence of ventricular fibrillation is very high: up to 25% during the first year and approximately 5% during the second year (N. M. Shevchenko, 1992).
Violation of autonomic regulation of the heart
In case of coronary artery disease, inflammatory myocardial diseases, diabetes mellitus and other diseases, damage to the autonomic nervous system is observed, which causes its dysfunction and leads, in particular, to a decrease in the effects on the heart and an increase in sympathetic activity. Signs of a violation of the autonomic regulation of the heart are an increase in heart rate and a decrease in heart rate variability.
An increase in sympathetic activity significantly increases the risk of sudden cardiac death, especially in the morning, after the patient awakens. Sympathetic stimulation is also promoted by various toxic effects on the myocardium (smoking, alcohol).
REMINDER FOR THE POPULATION
Prevention of Sudden Cardiac Death
The problem of sudden cardiac death (SCD) has remained one of the pressing health problems for many years due to its medical and social significance, as well as its drama. Sudden cardiac death is understood as circulatory arrest that develops suddenly, within an hour from the onset of clinical symptoms. This outcome is unexpected both for doctors and relatives, since the patient is in a stable condition on the eve of the attack. In some people, sudden cardiac death is the first and last manifestation of the disease. What is the reason for such transience of events? Sudden cardiac death in most cases is an arrhythmic death, in which medical care should be provided within the first 5-6 minutes, and in 90% of cases, circulatory arrest during sudden cardiac death occurs outside of a hospital setting.
According to WHO, the incidence of sudden cardiac death is 30 cases per week per 1 million population. To make it easier to imagine the scale of the problem, here are the following figures: in Europe and the USA, about 350,000 people die suddenly every year (this is an entire city of regional significance!), and every 5 minutes in the world one person dies suddenly! Unfortunately, there are no accurate statistics on sudden cardiac death in our country, since such a diagnosis is not included in post-mortem reports. However, given the high morbidity and mortality from cardiovascular diseases in our country, one of the highest in Europe, there is no doubt that we are “leaders” in this matter.
Since, as indicated, resuscitation measures in case of circulatory arrest must be carried out immediately, and in real life are not always feasible, the main approach to solving the problem of sudden cardiac death is its prevention. It should primarily be carried out in individuals at high risk of sudden cardiac death. Among heart diseases, the main cause of sudden cardiac death is coronary heart disease, which accounts for up to 80% of all cases of sudden cardiac death, and especially in patients who have had a myocardial infarction.
The examination program for patients with coronary artery disease should include:
- Consultation with a cardiologist;
- ECG;
- Test with physical activity - treadmill test;
- Echocardiography;
- Daily ECG monitoring with additional options (assessment of heart rate variability, sinus rhythm turbulence, T wave alternans);
- High-resolution ECG with registration of late ventricular potentials.
Recently, the issue of the risk of sudden death in athletes has become relevant. In an analysis of 185 cases of death of athletes in the United States (1985-1995), the main cause was identified as cardiovascular pathology, with hypertrophic cardiomyopathy leading in it (36%). When analyzing medical documentation, more than a third of athletes noted fainting or pre-fainting conditions, or cardiac complaints several months before death.
It is customary to distinguish three main categories of sudden death in athletes:
- 1st: “commotio cordis” syndrome - develops in the event of a strong blow to the heart, followed by a life-threatening arrhythmia;
- 2nd: sudden death in athletes under 30 years of age is usually associated with congenital cardiac pathology (hypertrophic cardiomyopathies, WPW syndrome, Brugada syndrome, etc.);
- 3rd: sudden death in athletes after 30 years of age, when the death is caused by an already acquired pathology, for example, ischemic heart disease.
The examination program for athletes should include:
- Consultation with a cardiologist;
- ECG;
- Echocardiography;
- Test with physical activity - treadmill test;
- Daily ECG monitoring.
In recent years, the development of sudden cardiac death has been identified as a cause such as respiratory arrest during sleep (obstructive apnea syndrome). This syndrome is manifested by snoring, pauses in breathing during sleep, and daytime sleepiness. In contrast to the generally accepted fact that the peak of cardiovascular mortality in the general population occurs in the early morning hours (from 6.00 to 12.00), in patients with obstructive apnea syndrome, the highest incidence of sudden cardiovascular mortality occurs during the night period (from 00.00 to 6.00). Sleep apnea leads to the development of sinus node arrest, AV blockade of various degrees, up to complete transverse block, and also contributes to the development of arterial hypertension, diabetes mellitus, and maintains obesity (obesity is typical for persons with obstructive apnea).
The examination program for patients with obstructive apnea syndrome should include:
- Consultation with a cardiologist;
- Consultation with an otolaryngologist;
- Polysomnography;
- Consultation with an endocrinologist.
To combat this disease, special breathing devices are selected that eliminate sleep apnea and normalize sleep.
I would like to emphasize that persons with so-called risk factors for cardiovascular diseases are also at risk of premature death. These include: smoking, hypertension, high cholesterol, family history of cardiovascular pathology, obesity, diabetes, physical inactivity. These individuals are recommended to undergo examination using scales developed by European cardiologists (see figure), as well as additional tests (homocysteine, myeloperoxidase, C-reactive protein, comprehensive lipid profile, etc.) and calculate the risk of fatal complications in the next 10 years.
About holding Health Day on the topic
“Let’s prevent the risks of sudden death!”
On October 8, 2021, the State Budgetary Institution “Center for Medical Prevention” of the Ministry of Health of the Krasnodar Territory will organize the next Health Day, which is held as part of the Day for the Prevention of Sudden Death and Life-Threatening Aries. Health Day is held with the aim of preventing cardiovascular diseases and promoting the principles of a healthy lifestyle. An indicative Health Day with the participation of regional specialists will be held in the city of Krasnodar. During the Health Day, organized jointly with the city administration and with the participation of the press, diagnostic tests, consultations, lectures, propaganda and festive events will be carried out.
Cardiovascular diseases, mainly sudden cardiac death (SCD), are the leading cause of death in most countries of the world. SCD is the most pressing problem of our time. The mechanisms underlying the development of sudden cardiac death in the vast majority of cases are ventricular tachycardia (VT) and ventricular fibrillation (VF) - 95%, and the remaining 5% are due to bradyarrhythmias and asystole. The main cause of SCD is coronary heart disease.
Sudden cardiac death is one of the pressing problems of our time. Currently, many different studies are being conducted to study this problem. When treating patients with cardiovascular diseases, the main efforts of doctors should be aimed at actively preventing sudden cardiac death with the help of drugs that have maximum effectiveness and safety.
The issue of preventing sudden cardiac arrest is very important, since the correct attitude to one’s own feelings and the complaints of a loved one will in many cases prevent a fatal outcome. As a number of research works show, many people ignore the warning signals sent by their own body. Thus, very often, patients resuscitated after a sudden stop of blood circulation report previous chest pain, attacks of severe weakness, shortness of breath, palpitations and some other symptoms that appeared hours, days or even weeks before the development of the episode. Many patients with diagnosed heart disease report deterioration of their condition prior to cardiac arrest, but the appearance of these symptoms for some reason does not prompt many of them to seek medical help. And this is due, first of all, to the lack of awareness of patients about the symptoms of heart disease and its potential complications and outcomes.
Sudden cardiac death is a rather insidious disease, and it is not always possible to identify potential patients. That is why the most important thing in the fight against this condition is the timely implementation of emergency measures. Nowadays, many public places have defibrillators that can be used for life-threatening arrhythmias. They also often conduct special courses on teaching resuscitation measures to ordinary citizens.
GBUZ "Center for Medical Prevention" of the Ministry of Health of the Krasnodar Territory.
Classification of the disease
According to the duration of development of symptoms of damage, heart failure is divided into acute and chronic. The first of them can develop in one of two types:
- To the left - left ventricular or left atrial.
- To the right - right ventricular.
Cardiovascular failure is classified, according to Vasilenko-Strazhesko, into three stages:
- First. This is the initial stage, characterized by the fact that hidden symptoms become noticeable only if the person is physically active. He experiences shortness of breath and rapid heartbeat. The patient gets tired quickly. In the absence of physical activity, these signs are absent.
- Second. Symptoms of long-term circulatory failure and stagnation of the entire cardiovascular system also appear when a person is at rest. The patient is considered disabled. This stage has two periods. 2nd A is characterized by moderate hemodynamic lesions in one of the sections of the organ. This is the left or right ventricle. Manifestations of shortness of breath are observed even with normal physical activity. The patient's performance decreases. Other manifestations are cyanotic skin color, swelling of the legs, heavy breathing. 2nd B A is characterized by serious violations. The entire cardiovascular system is involved in this process. External manifestations - a person feels shortness of breath even when at rest. Edema and cyanosis appear. The patient is completely disabled.
- Third. This final stage is characterized by a significant deterioration in blood circulation and metabolism. The structure of many organs, in particular the liver and lungs, is irreversibly damaged. The patient is exhausted.
What are the signs of heart failure?
Heart failure itself is a syndrome, not a disease. Therefore, painful sensations are unusual for her. Early signs of the development of this condition are shortness of breath, weakness, and swelling in the legs by the end of the day. “If a person has healthy veins, but at the end of the day there are marks on the legs from the elastic bands of socks, you need to check the heart. The syndrome can also be recognized by the appearance of shortness of breath during normal exertion. You should be wary if a person normally climbed to the fourth floor, but now he needs to stop and rest on the second. As the syndrome develops, these signs get worse,” says Belenkov.
Article on the topic
The disease of the dissatisfied. What symptoms indicate the onset of heart problems?
The domestic Strazhesko-Vasilenko classification identifies three stages of development of chronic heart failure. At the initial, first stage, shortness of breath and rapid heartbeat appear with significant physical stress. At the second stage, clinical manifestations begin at rest: prolonged circulatory failure, congestive changes in the lungs, stagnation first in the pulmonary circulation, and then in both circles. At the final, third stage of the disease, irreversible changes in vital organs occur (liver cirrhosis, “stagnant” kidney, etc.), metabolism is disrupted, and treatment becomes ineffective.
Signs indicating the presence of heart failure
If a patient has acute heart failure, the activity of any part of the heart is weakened. This could be the left atrium, one of the ventricles. Left ventricular failure occurs when there is a disease that puts stress on this department. It could be hypertension, heart attack.
In this case, there is an increase in pressure in some blood vessels and an increase in their permeability. The consequence of this is interstitial edema, which turns into alveolar edema. A similar type of failure manifests itself in the form of cardiac asthma. Alveolar pulmonary edema is also observed.
Exacerbation of asthma is usually caused by excessive physical activity or great emotional stress. Most often, a person experiences severe and sudden suffocation at night, during sleep. As a result, the patient wakes up in horror.
This type of asthma manifests itself as a feeling of lack of oxygen, increased heart rate, wet cough, and severe weakness. During an attack, the patient becomes covered in cold sweat, and when lying down he experiences severe shortness of breath. The specialist conducting the examination notes that the surface of the skin has turned gray and cyanotic, the person has shortness of breath and cold sweat. The pulse becomes weak and arrhythmic. The borders of the heart expand to the left. Blood pressure decreases. When listening to the lungs, harsh breathing is observed.
There is an increase in stagnation in the pulmonary circulation. As a result, pulmonary edema develops. The patient experiences a state of suffocation, and sputum is released. It is foamy, has a pinkish tint, and is very abundant. This is due to the presence of blood in it. Even strangers hear heavy, hoarse breathing with bubbling sounds. The patient is forced to be in a vertical position, since in a horizontal position his shortness of breath increases.
The face becomes bluish, the veins in the neck swell, and the patient breaks out in a cold sweat. The pulse is rapid, thread-like, the pressure is low, and wheezing is heard when breathing. If pulmonary edema occurs that requires urgent intervention, intensive care measures must be taken. Otherwise, everything could end very sadly.
Acute heart failure of the left atrium is observed in the case of mitral stenosis. The manifestations of the disease are similar to those found in left ventricular disease.
Damage to the right ventricle is usually a consequence of pulmonary embolism. Congestion appears in the systemic circulation. As a result, the legs begin to swell, the veins of the neck swell, shortness of breath appears, the skin becomes bluish, and there is pressure and pain in the area of the heart. There is a sharp decrease in blood pressure and expansion of the heart to the right.
If a patient has a disease that causes the right ventricle to malfunction, heart failure will appear sooner than if the same happens to the left ventricle. After all, this part of the heart is considered the most powerful. But, if there is a decrease in its functions, the development of heart failure occurs very quickly.
Chronic heart failure is characterized by the fact that at the very beginning its development can be of any type - right and left atrial, right and left ventricular. If there is an aortic defect, arterial hypertension, or some other ailments, congestion is observed in the vessels of the pulmonary circulation, leading to left ventricular failure. At the same time, vascular changes occur in the lungs. A person experiences shortness of breath, suffocation (usually at night), and bluish skin color. There is an increased heart rate, dry cough, and the patient gets tired very quickly.
If there are problems with the left atrium, severe congestion of the small circle appears. This happens in people who have mitral valve stenosis. The patient experiences shortness of breath, constantly coughs, and begins to spit up blood. If stagnation in the veins continues for a long time, sclerosis is observed in the vessels and lungs. Blood circulation in the pulmonary circle worsens, as an additional obstacle appears. The load on the right ventricle increases, and it is this circumstance that explains the occurrence of failure.
If the right ventricle is mainly affected, stagnation covers a large circle. A disease of this type can be a consequence of mitral heart defects, pneumosclerosis, and other ailments. The patient begins to complain that he has pain under his right rib and feels heaviness. He develops swelling, his abdomen becomes enlarged, and shortness of breath occurs with even slight physical activity. Diuresis decreases, the skin becomes cyanotic. Swelling of the veins of the neck and enlargement of the liver are observed.
A lesion that affects only one part of the heart spreads to others after some time. This is how total chronic heart failure occurs, the symptoms and treatment of which should be carried out by a cardiologist. Congestion in the veins is observed in both the small and large circles. A similar problem arises in the following cases: with damage to the heart muscle, myocarditis, coronary artery disease, and some others.
Sudden cardiac death (SCD) is defined as natural death
resulting from the cessation of effective heart function. As a rule, in this case, either ventricular fibrillation or primary cardiac arrest develops. The key concepts guiding the definition of sudden death are that the cause is non-traumatic and that the onset of death is immediate and unpredictable.
In almost 90% of cases, acute coronary death is caused by coronary heart disease. It also happens that before this, IHD did not manifest itself in any way, that is, it was asymptomatic. In some cases, the patient was bothered by angina attacks and arrhythmia. After a heart attack, the risk of sudden death increases several times.
Groups of people at high risk of SCD:
- Patients undergoing resuscitation due to cardiac arrest or ventricular fibrillation;
- Patients with chronic heart failure and ischemia;
- Persons with electrical instability in the conductive system;
- Those diagnosed with significant cardiac hypertrophy.
In a quarter of all cases of sudden death of adults, there were no previous symptoms; it occurred without obvious reasons. Other patients noted, one to two weeks before the attack, a deterioration in their health in the form of: b more frequent pain attacks in the heart area; increasing shortness of breath; a noticeable decrease in performance, feelings of fatigue and fatigue; more frequent episodes of arrhythmia and interruptions in cardiac activity. These signs can be considered harbingers of an impending threat; they indicate an exacerbation of existing heart problems, so it is advisable to consult a cardiologist when they appear.
Before cardiovascular death, pain in the heart area increases sharply, many patients manage to complain about it and experience severe fear, as happens with myocardial infarction. Psychomotor agitation is possible, the patient grabs the heart area, breathes noisily and frequently, gasps for air, sweating and redness of the face are possible. Nine out of ten cases of sudden coronary death occur outside the home, often against the background of strong emotional distress or physical overload, but it happens that the patient dies from acute coronary pathology in his sleep.
When ventricular fibrillation and cardiac arrest occur during an attack, severe weakness appears, dizziness begins, the patient loses consciousness and falls, breathing becomes noisy, and convulsions are possible due to deep hypoxia of the brain tissue.
Upon examination, pale skin is noted, the pupils dilate and stop responding to light, heart sounds cannot be heard due to their absence, and the pulse in large vessels is also not detected. In a matter of minutes, clinical death occurs with all its characteristic signs. Since the heart does not contract, the blood supply to all internal organs is disrupted, so within a few minutes after loss of consciousness and asystole, breathing disappears.
Since sudden cardiac death syndrome causes cardiac arrest and respiratory failure, the first step is to restore the functioning of life support organs. Emergency care should be started as early as possible and includes cardiopulmonary resuscitation and immediate transport of the patient to the hospital.
At the prehospital stage, the possibilities of resuscitation are limited; it is usually carried out by emergency specialists who find the patient in a variety of conditions - on the street, at home, at the workplace. It’s good if at the time of the attack there is a person nearby who knows her techniques - artificial respiration and chest compressions.
Sudden coronary death leads to irreversible changes in the cerebral cortex within 5-6 minutes. Therefore, emergency measures to restore blood flow must begin immediately and continue until the arrival of the medical team.
Every person needs to know the basics of cardiopulmonary resuscitation. Her tasks include checking and, if necessary, restoring the patency of the airways, starting artificial ventilation (mouth-to-mouth, mouth-to-nose), and chest compressions. According to the latest recommendations, a person without experience can skip the first two points and immediately begin cardiac massage. Several studies have shown that this approach is more effective and leads to improved survival.
Indirect cardiac massage should be performed as follows:
- Place the person on their back on a hard surface;
- Place your palms on the middle third of the sternum perpendicular to it;
- Start squeezing your chest without bending your elbows;
- In this case, the sternum should bend by 5 cm, and the frequency of movements should be about 100 per minute.
The effectiveness of resuscitation measures can be judged by the color of the skin.
Prevention of sudden coronary death is needed for people with chronic diseases of the cardiovascular system, which can cause an attack, as well as for those who have already survived it and were successfully resuscitated. To prevent a heart attack, a cardioverter defibrillator may be implanted, which is especially effective for serious arrhythmias. At the right moment, the device generates the impulse the heart needs and does not allow it to stop. Heart rhythm disturbances require medication support. Beta blockers, calcium channel blockers, and products containing omega-3 fatty acids are prescribed. Surgical prevention consists of operations aimed at eliminating arrhythmias. Nonspecific measures to prevent cardiac death are the same as for any other cardiac or vascular pathology - a healthy lifestyle, physical activity, giving up bad habits, proper nutrition.
State Budgetary Institution "Center for Medical Prevention" of the Ministry of Health of the Republic of Kazakhstan
Diagnosis of the disease
Since such an ailment is considered secondary and its development occurs in the presence of other diseases that are already known to specialists, the goal of diagnosis is to identify it at an early stage, even if there are no obvious symptoms.
The first symptoms of heart failure in women and men are fatigue and shortness of breath. Therefore, first of all you should pay attention to them. It is necessary to monitor patients with hypertension and coronary artery disease. People who have suffered a heart attack or rheumatic attacks are at risk. Specific symptoms of the disease include swelling of the legs and accumulation of fluid in the abdominal cavity. You need to be wary when the 3rd heart sound appears and its boundaries shift.
If there are concerns that the patient is developing heart failure, the gas and electrolyte composition of the blood is analyzed. Acid-base balance studies are carried out and other tests are taken.
The presence of coronary heart disease, arrhythmia, and myocardium can be determined by an electrocardiogram. In addition, a variety of load tests are often used. To do this, they resort to the help of treadmills and exercise bikes. Such testing, in which the load gradually increases, indicates the reserves of the heart.
The use of ultrasound echocardiography helps determine the cause of heart failure. In addition, in this way the pumping activity of the myocardium is assessed. MRI performed on this organ helps to identify ischemia, various heart defects, etc.
Using X-ray examination of the lungs and other organs, it is possible to determine the presence of blood stagnation in the pulmonary circulation. Radioisotope ventriculography, performed in patients with signs of heart failure, makes it possible to accurately determine the contractility of the myocardium. In addition, using this method you can install out of capacity.
If a serious form of the disease is present, an ultrasound examination of the liver, pancreas, and other important organs is performed to assess the condition of the internal organs.
Diagnostics
Symptoms of congestive heart failure are observed by the therapist when examining the patient and listening to heart sounds. He refers the patient to a cardiologist. A number of studies are being carried out:
- ECG;
- ECHOCG
- HMEKG
- Radiography
- Coronary angiography
- MRI, MSCT
Research is being conducted on the characteristics of the heartbeat during physical activity. To do this, the patient is asked to perform a series of simple exercises, such as squats. After this, monitor the change and restoration of the pulse. More in-depth examinations of this kind are performed using a treadmill or exercise bike.
Methods of treating the disease
The main goal of treating patients is to eliminate the factors that cause heart failure. Among them are rheumatism, ischemia, hypertension, etc. In some cases, surgery is required, this happens with heart defects, aneurysm, and other problems that cause a mechanical barrier to the functioning of the organ.
If the patient has severe or acute cardiovascular failure, the specialist prescribes him to adhere to bed rest. In addition, complete rest is recommended for him. If the condition is not so serious, the load may be moderate and will not affect your well-being.
It is not advisable for the patient to consume more than 600 ml of liquid per day; salt should be either completely excluded from the diet or limited to 1-2 grams. Food should be easily digestible, with plenty of vitamins.
Pharmacotherapy brings good results; it makes it possible to significantly improve the condition of patients and improve their quality of life. Treatment of heart failure involves taking several groups of medications:
- Cardiac glycosides. They are needed to improve myocardial contractility. As a result, its pumping function and diuresis increase. The products help to tolerate physical activity normally. Among the drugs are strophanthin, digoxin, etc.
- ACE inhibitors, vasodilators. Their effect is a decrease in vascular tone. The drugs cause the blood vessels to dilate. Thus, as the heart contracts, its resistance decreases, therefore, cardiac output becomes greater.
- Nitrates. The purpose of the funds is to improve the filling of blood in the ventricles. Their use allows you to increase cardiac output and make the coronary arteries wider. Among them are sustak, nitroglycerin, etc.
- Diuretics. Prevents the retention of excess water in the body. This is furosemide, etc.
- Beta blockers. Their use leads to a decrease in heartbeats, improvement in its filling with blood, and an increase in cardiac output.
- Anticoagulants. Prevents the formation of blood clots in blood vessels. This is, in particular, aspirin.
- Means leading to improvement of myocardial metabolism. These are vitamins B, C, riboxin.
If a patient develops pulmonary edema, he should be admitted to a hospital where he will receive emergency treatment. He will need to take diuretics and nitrates. The patient is given drugs that increase cardiac output. In addition, he is prescribed oxygen inhalations.
When water accumulates in the abdominal cavity, it is removed using punctures. If pneumothorax occurs, pleural puncture is necessary. If a patient has a low oxygen content in the tissues, oxygen therapy is recommended. That is, if there is heart failure with symptoms, treatment - tablets, other drugs - should be prescribed by a specialist.
What causes heart failure?
Heart failure is a syndrome that develops against the background of various heart diseases. “In our country this is caused by inadequate treatment of arterial hypertension; in all European countries it is mainly coronary heart disease and myocardial infarction. This could be cardiomyopathy, myocarditis, heart disease, etc. There are many reasons,” notes Belenkov.
There are factors that increase the likelihood of developing or worsening heart failure. “The first and main thing is irregular treatment. The second is a cold. Any severe cold can cause an exacerbation, so such patients must be vaccinated. This is also a violation of the diet, alcohol intake, excessive physical activity, which is not recommended for the patient,” says the cardiologist.
What awaits patients
Half of all patients diagnosed with heart failure live more than five years. It is difficult to talk about maximum life expectancy; this indicator is determined by many factors. These include the severity of the disease, concomitant background, and the effectiveness of the prescribed treatment. The kind of life the patient leads and much more is of great importance.
If the disease is detected in the initial stage, with the help of therapy the patient’s condition can be completely compensated. At stage 3 of the disease, experts talk about a worse prognosis.
What treatment is prescribed for heart failure?
Self-medication in this case is unacceptable. A qualified doctor will select the necessary medications in accordance with the patient’s condition and the stage of the disease.
It is mandatory to prescribe medications that stimulate the work of the heart muscle. In addition, diuretics are indicated. If necessary, oxygen therapy is provided.
Treatment of the disease that caused heart failure syndrome is of great importance.
It should be noted that in most cases, medication must be continued throughout life.
Preventive measures
For preventive purposes, to prevent the occurrence of such a disease, it is necessary to prevent the development of diseases that lead to it. Among them is ischemia, hypertension, heart defects. In addition, it is necessary to prevent as much as possible the emergence of factors that favor the appearance.
If you have heart failure, the symptoms of which have already appeared, you must first of all try to prevent its progression. To do this, you should not exceed the recommended physical activity, take all medications prescribed by your doctor, and be regularly examined by a cardiologist. The doctors of the Clinical Hospital “RZD-Medicine” in Nizhny Novgorod will help you monitor your health.
Is it possible to have heart failure at a young age?
According to Belenkov, heart failure is possible at any age. “This is a condition that accompanies many diseases, including heart defects. And heart defects can be congenital. Therefore, heart failure can also occur in a newborn,” the doctor notes.
Meanwhile, the prevalence of chronic heart failure increases significantly with age. Among patients 20-29 years old, it occurs in 0.3% of cases, and in people over 90 years old - in almost 70% of cases. According to statistics, more than 65% of people with this syndrome belong to the age group 60+. According to Belenkov, this is due to the fact that among this age category there are more patients with myocardial infarction and those who suffer from arterial hypertension.
Treatment
Given the severity of the disease, treatment for congestive heart failure should begin as early as possible. First of all, the doctor prescribes non-drug therapy, which includes:
- Constant control of body weight
- Load limitation
- Special training complex
- Review of the daily diet with mandatory limitation of salt intake
- Limiting fluid intake
Additionally, drug treatment is provided, including:
- Use of cardiac glycosides
- Fluid removal medications
- Use of drugs to prevent arrhythmic manifestations
In this list, the main drugs are glycosides necessary to maintain the pumping function of the heart. Given the importance of these drugs, they are prescribed on an ongoing basis. No less important in the fight against the manifestations of congestive heart failure are diuretics. They help remove excess fluid from all organs, preventing swelling from developing. Since minerals and other beneficial substances are inevitably washed out of the body with the removal of fluid, the use of drugs with a high potassium content is recommended.
Along with the treatment of congestive manifestations in the heart, therapy is carried out for the disease that led to the development of this disease. It is mandatory to use drugs whose action is aimed at maintaining heart function. Medicines that help relieve blockages in blood vessels should also be used.
If drug therapy does not produce positive results, the only option may be an organ transplant. Although, in some cases, chronic congestive heart failure can be eliminated by surgical correction of the main disease.
In conclusion, we note that for the treatment of heart failure it is important to identify the causes that led to the development of such a serious illness. Then a list of non-drug measures aimed at stabilizing the general condition is compiled. Among such measures, it is mandatory to limit the consumption of salt and water. Under no circumstances should you stop physical activity completely. A minimum set of special exercises should be performed daily. The final stage of therapy is taking medications that are determined by the cardiologist.
You can make an appointment with a cardiologist at the ProfMedPomoshch clinic by phone or through online forms on the website.
Acute cardiovascular failure
Acute cardiovascular failure is the inability of the heart and blood vessels to provide blood supply to body tissues adequate to metabolic needs, which leads to dysfunction of cells and their death.
The causes of the pathology can be mechanical trauma, bleeding, burns, excessive loss of water and salts by the body, intoxication with exogenous and endogenous poisons, the action of microorganisms and their toxins, immediate hypersensitive reaction to allergens, coronary heart disease, arrhythmias, disorders of neurohumoral regulation of vascular tone, etc. .d.
Acute heart failure is a violation of the pumping function of the heart. It can develop as a result of both cardiac disorders (heart disease) and secondary, under the influence of extracardiac factors (infection, intoxication). Acute heart failure occurs in the left and right ventricular types.
Acute left ventricular failure is the inability of the left ventricle to pump blood from the pulmonary circulation to the large circulation. Most often it occurs with myocardial infarction, mitral heart disease, stenosis of the left atrioventricular orifice, stenosis and insufficiency of the aortic valve, hypertension, coronary vascular sclerosis, acute pneumonia.
Patients experience impaired blood circulation in the coronary vessels (which occurs only during diastole and is intermittent) and cardiac output decreases. During systole, not all the blood is pushed into the aorta, but some remains in the left ventricle. Therefore, during diastole, the pressure in it increases, which leads to stagnation of blood in the left atrium. The right ventricle, which retains its function, continues to pump blood into the pulmonary vessels, which are not able to accommodate such a volume. Hydrostatic pressure in the vessels of the pulmonary circulation increases; The liquid part of the blood passes into the lung tissue.
Patients experience suffocation (first during physical exertion, and then at rest). Subsequent attacks of suffocation are accompanied by a cough producing pink sputum. This condition is called cardiac asthma. With a further increase in hydrostatic pressure in the capillaries of the pulmonary circulation (over 150-200 mm Hg), the liquid part of the blood penetrates into the lumen of the alveoli. Pulmonary edema occurs. There are interstitial and alveolar pulmonary edema.
With interstitial edema, serous fluid is released from the congestive vessels of the small circle and infiltrates all lung tissues, including the peribronchial and perivascular spaces.
With alveolar edema, not only plasma penetrates into the lumen of the alveoli, but also erythrocytes, leukocytes, and platelets. When breathing, liquid mixes with air; A large amount of foam is formed, which disrupts the flow of oxygen into the blood. Circulatory hypoxia (due to heart failure) is accompanied by hypoxic hypoxia (due to impaired oxygen supply).
The patient's condition deteriorates sharply. He takes a forced (sitting) position. Shortness of breath increases (30-35 breaths per minute), which often turns into suffocation. Acrocyanosis occurs. Consciousness is clouded, psychomotor agitation is observed (due to hypoxia of the central nervous system). The breath is squeaky, with the release of pink foam. Multiple moist rales of different sizes are heard in the lungs, which can be heard at a distance (the “boiling samovar” symptom).
There are two forms of pulmonary edema: with high blood pressure (hypertension, aortic valve insufficiency, with damage to the structures and vessels of the brain) and with normal or low blood pressure (with extensive myocardial infarction, acute myocarditis, severe mitral or aortic heart disease, severe pneumonia).
Stages of the disease
Congestive heart failure manifests itself in three stages, each of which is characterized by a specific list of symptoms:
- Initial first stage. During this period of disease development, patients note increased fatigue, tachycardia, and restless sleep. With little physical activity, a person feels shortness of breath and increased heart rate.
- The second stage of the disease is characterized by a constant feeling of fatigue and increased heart rate. During this period, right- or left-sided insufficiency is clearly diagnosed.
- The third and final stage entails serious changes in the body. At this stage, pulmonary insufficiency manifests itself, the development of cirrhosis of the liver, and disturbances in intestinal function are possible. If by this time the treatment has not yielded positive results, the patient will die.