Rheumatism
Terminology
Rheumatism is one of those diseases that everyone knows about or, at least, has heard of.
However, prevailing ideas about rheumatism vary very widely: from the childhood fear of sneakers (“You can’t always walk in them - you’ll catch a cold and get rheumatism!”) to a more adult discovery: it turns out that rheumatism affects not the legs, but the heart. A careful study of available sources sometimes only confuses the situation. In fact, how can we understand a disease in which it is not a single organ or even a functional system that suffers, but an entire type of tissue in the body? However, this is exactly what happens with rheumatism. Rheumatism is an inflammatory-immune lesion of connective tissue, which is present almost everywhere in the body.
The definition of “inflammatory-immune” should be used in this order: first inflammation, then an immune reaction to it, and then an autoimmune attack on one’s own connective tissue. This is akin to what a brave, fast, but not very accurate bodyguard can do, continuing to shoot in bursts after the invasion has long been repulsed...
As a rule, the connective tissue structures of the heart, joints, blood vessels, and subcutaneous layers are affected. Much less common (1-6 percent of the total volume of registered rheumatism) are rheumatic lesions of the central nervous system, respiratory and visual organs, and gastrointestinal tract.
Rheumatism does not show any endemicity (regional dependence of epidemiological indicators): people get sick everywhere. However, there is a clear dependence of morbidity on age - among primary patients, the category of 5-15 years predominates - as well as an inverse correlation with the standard of living of the population. Considering that the majority of children on the globe (up to 80%) live in the so-called. developing countries, one should not be surprised at the widespread prevalence of rheumatism in the “third world”.
In the last quarter of a century, morbidity and mortality in Russia have decreased by more than three times. However, if we are talking about such a serious disease, and even with a predominantly early manifestation, no epidemiological data can be considered “satisfactory”, except zero. Today, statistics are contradictory and are mainly of an evaluative nature (and this applies not only to the Russian Federation): as a rule, data from the 1960s-90s are extrapolated to the current situation. A more or less reliable estimate of the incidence among Russian children can be considered a frequency of 2-3 cases per 10,000 (and over 1.5% of all heart defects are rheumatic); for comparison, in third world countries this figure varies from 60 to 220 per 10,000.
In conclusion of a brief general overview, it should be noted that the term “rheumatism” itself is currently used mainly by Russian-speaking medicine. In the official international lexicon these are “Acute rheumatic fever”, “Rheumatic heart disease”, “Rheumatoid arthritis”, etc.; however, code M79.0 (heading “Diseases of the musculoskeletal system and connective tissue”) in ICD-10 indicates “Rheumatism, unspecified.”
Symptoms of chronic rheumatic heart disease
Mitral regurgitation (mitral valve insufficiency)
Long-term patients do not complain; the defect can be detected during a random medical examination. As the disease progresses, the following appear:
- shortness of breath during physical exertion, and then at rest, attacks of suffocation at night;
- cyanotic blush in the cheek area;
- acrocyanosis;
- cough with a small amount of sputum;
- pain in the right hypochondrium due to an increase in the size of the liver;
- swelling of the legs and feet;
- general weakness.
The main auscultatory sign of mitral insufficiency: systolic murmur at the apex of the heart.
Mitral stenosis (narrowing of the left atrioventricular opening):
- dyspnea;
- attacks of suffocation at night;
- cough with sputum, sometimes mixed with blood;
- cyanotic flush of the cheeks;
- heartbeat;
- swelling;
- chest pain;
- weight loss;
- children have retarded growth and physical development;
- general weakness, increased fatigue.
Auscultatory signs: mitral valve opening tone, “quail rhythm”, diastolic murmur at the apex of the heart.
Aortic valve insufficiency:
- sensation of pulsation in the area of the vessels of the neck, in the area of the heart;
- heartbeat;
- dizziness, fainting;
- pain in the heart area that occurs during physical activity;
- dyspnea;
- swelling of the legs, feet;
- general weakness, fatigue.
Auscultatory sign: protodiastolic murmur at Botkin's point.
Symptoms
| Occurrence (how often a symptom occurs in a given disease) | |
| Rapid heartbeat - more than 60 beats per minute | 90% |
| Disturbances in the rhythm of the heart of various types (arrhythmia) (irregular heart rhythm, interruptions in the heart) | 80% |
| Constant or periodic shortness of breath without connection with body position or stress | 60% |
| Heart pain during exercise | 50% |
| Cough producing viscous mucous sputum | 50% |
| Edema of the legs (swelling of the legs) | 20% |
| Decreased appetite (loss of appetite, appetite disturbances) | 15% |
| General weakness (fatigue, tiredness, weakness of the body) | 5% |
Treatment of chronic rheumatic heart disease
If symptoms of heart failure develop, surgical treatment is performed - heart valve replacement.
Essential drugs
There are contraindications. Specialist consultation is required.
- Hydrochlorothiazide (diuretic). Dosage regimen: orally, at a dose of 25-100 mg per day once or once every 2 days. Depending on the clinical response, the dose may be reduced to 25-50 mg per day once or once every 2 days.
- Bisoprolol (antiarrhythmic drug). Dosage regimen: orally, without chewing, with a small amount of liquid, in the morning on an empty stomach or during breakfast 1.2510 mg 1 time per day.
- Amlodipine (antianginal, antihypertensive drug). Dosage regimen: orally, after meals, with a small amount of water at an initial dose of 2.5-5 mg 1 time / day. If necessary, the dose can be gradually increased to a maximum of 10 mg 1 time / day.
- Digoxin (antiarrhythmic drug). Dosage regimen: orally, at a saturation dose for adults of 0.5-1.0 mg, then take 0.25 mg every 6 hours until the desired therapeutic effect is achieved. Maintenance dose 0.125-0.25 mg/day.
- Warfarin (indirect anticoagulant). Dosage regimen: orally in a dose of 2.5-10 mg 1 time per day at the same time. The initial dose for patients who have not previously used warfarin is 5 mg per day (2 tablets) for the first 4 days. On the 5th day of treatment, MHO is determined. The maintenance dose of the drug should keep the INR at 2.0-3.0.
Acquired heart defects
Acquired heart defects are a group of diseases accompanied by disruption of the structure and function of the heart valve apparatus and leading to changes in intracardiac circulation.
Acquired heart defects develop as a result of acute or chronic (long-term) diseases and injuries that impair the function of the valves and cause changes in intracardiac hemodynamics (blood movement through the vessels).
More than half of all acquired heart defects are due to lesions of the mitral (located between the left atrium and the left ventricle) valve, about a third are lesions of the aortic (separates the left ventricle and aorta) valve, the rest are represented by combined (changes affecting several valves) defects.
Symptoms of acquired heart disease
- Dyspnea.
- Marked weakness.
- Changes in skin color - constant pallor or, conversely, pinkishness.
- Feeling of heartbeat.
- Possible pain in the heart area during physical activity.
- Headaches, dizziness, fainting (loss of consciousness).
Forms
Acquired heart defects are classified into several categories.
According to etiology (cause of occurrence) there are:
- rheumatic (occurs as a result of rheumatism - a systemic inflammatory disease of connective tissue with predominant damage to the heart);
- endocardial (due to endocarditis - inflammation of the inner lining of the heart);
- syphilitic (due to syphilis - a systemic disease that is predominantly sexually transmitted and affects many organs and systems) and so on.
Based on the type of valve affected, the following are distinguished:
- aortic;
- mitral;
- tricuspid valve defect;
- valve defect of the pulmonary artery trunk.
By the number of affected valves:
- isolated, or local (damage to 1 valve),
- combined defect - insufficiency and stenosis (narrowing of the lumen) simultaneously occur on one valve;
- combined defect - changes affect several valves.
Functionally:
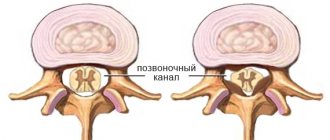
- stenosis - narrowing of the lumen of the opening as a result of post-inflammatory (occurs after the inflammatory process) cicatricial adhesions of the valve leaflets;
- insufficiency - incomplete closure of the heart valve leaflets;
- prolapse - protrusion, protrusion or eversion of the valves into the cavity of the heart.
According to the severity of the defect and the degree of hemodynamic disturbance (blood movement through the vessels) of the heart:
- does not have a significant effect on intracardiac circulation;
- moderately expressed;
- pronounced.
According to the state of general hemodynamics:
- compensated heart defects - without circulatory failure (a condition in which the heart is not able to adequately supply blood to all organs and tissues);
- subcompensated - with transient (temporary) decompensation (inability to compensate for impaired blood flow) caused by excessive physical exertion, elevated body temperature, pregnancy, and so on;
- decompensated - with developed circulatory failure.
Reasons for purchasing
The most common causes of acquired heart defects are:
- rheumatism is a systemic inflammatory disease of connective tissue primarily affecting the heart;
- infective endocarditis (inflammation of the inner wall of the heart);
- atherosclerosis is a chronic disease characterized by hardening and loss of elasticity of the walls of the arteries, narrowing of their lumen due to the so-called atherosclerotic plaques (formations consisting of a mixture of fats (primarily cholesterol (a fat-like substance that is a “building material” for the body’s cells) and calcium ));
- heart injuries (bruises and wounds of the heart muscle);
- syphilis is a systemic disease, transmitted primarily through sexual contact and affecting many organs and systems;
- sepsis (blood poisoning) and others.
Diagnostics
- Analysis of the medical history and complaints - when (how long ago) and what kind of complaints appeared, whether the patient consulted a doctor, underwent examination and treatment, with what results, and so on.
- Analysis of life history - past infectious diseases and chest injuries are clarified.
- Analysis of family history - it is found out whether any of the close relatives have heart diseases, what kind of diseases they are, and whether there have been cases of heart defects in the family.
- Medical examination. Wheezing in the lungs, murmurs in the heart are determined, the level of blood pressure is measured, the boundaries of the heart are determined by percussion (by tapping) (to determine hypertrophy (increase in size)), heart sounds and sounds are listened to to determine the type of defect, the lungs are auscultated and the size of the liver is determined ( to diagnose heart failure, a condition in which the heart cannot provide adequate blood flow to all organs).
- General blood test - allows you to detect signs of inflammation in the body (increased levels of leukocytes (white blood cells), increased levels of ESR (erythrocyte sedimentation rate (red blood cells), a nonspecific sign of inflammation)) and identify complications and possible causes of heart disease.
- A general urine test can detect complications of heart defects.
- Biochemical blood test - determination of the level of total cholesterol (a fat-like substance that is a “building material” for the body’s cells), “bad” (promotes the formation of atherosclerotic “plaques” (cell clots)) and “good” (prevents the formation of “plaques”) cholesterol, level of triglycerides (fats, the source of cell energy), blood sugar.
- Electrocardiography (ECG) is a method of recording the electrical activity of the heart on paper. Allows you to diagnose changes in heart rhythm, determine the type of arrhythmia and signs of ischemia (insufficient blood supply to the heart muscle).
- Phonocardiography is the recording of sound signals of the beating heart: murmurs and tones. The method allows you to assess the duration, intensity, nature, origin of heart murmurs and tones, and record the third and fourth heart sounds, which are indistinguishable by ear, which ultimately allows you to determine the type and nature of the heart defect.
- Echocardiography (EchoCG) is an ultrasound examination of the heart. Allows you to diagnose the defect itself, the area of the atrioventricular orifice (connecting the atrium and ventricle of the heart), the severity of regurgitation (backflow of blood), the condition and size of the valves, and determine the pressure in the vessels.
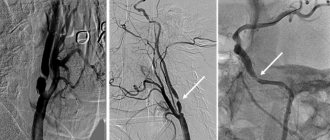
- Chest X-ray with intravenous contrast agent (angiocardiography) - assesses the condition of the lungs, the size of the heart and its chambers. The method helps to identify specific changes in the vascular bed in such patients.
- Multislice computed tomography - cardiography (MSCT of the heart) is a method of layer-by-layer scanning of heart structures, based on recording an X-ray beam passing through tissue using several rows of ultra-sensitive detectors. Cardiac MSCT enables 3-dimensional reconstruction of the heart and is used to identify valve defects.
- Cardiac magnetic resonance imaging (MRI) is a method of obtaining diagnostic images based on the physical phenomenon of nuclear magnetic resonance, thus it is safe for the body.
- It is also possible to consult a therapist or cardiac surgeon.
Treatment of acquired heart disease
Conservative (drug) treatment of acquired heart disease is prescribed only with the goal of stabilizing the heart rhythm, preventing heart failure (a condition in which the heart is unable to provide normal blood flow to all organs), complications and relapses (recurrences) of the underlying disease that caused the heart disease.
The main treatment method for acquired heart defects is surgery.
Valve defect correction:
- valvotomy (dissection of fused heart valves);
- valvuloplasty (restoration of valve function by cutting the valve walls and subsequent suturing of new leaflets).
- Prosthetic valve replacement (replacement with an artificial one).
Complications and consequences
- The development of heart failure (a condition in which the heart is unable to adequately supply blood to all organs and tissues).
- Heart rhythm disturbance (any heart rhythm other than normal).
- Thromboembolic complications (complications in which blood clots (blood clots in a vessel) can enter any vessel in the body through the bloodstream, block its lumen and cause organ dysfunction).
- Disability of patients.
- Lethal outcome (death).
Prevention of acquired heart disease
Prevention of all acquired heart defects consists in preventing the underlying disease that causes the defect (for example, timely treatment of tonsillitis (an infectious disease primarily affecting the palatine tonsils) prevents the development of rheumatism (a systemic inflammatory disease of connective tissue primarily affecting the heart)).