Minute blood volume
To determine the IOC, the amount of blood passing through one of the atria in 1 minute is calculated. The characteristic is measured in liters or milliliters. Taking into account the individuality of the human body, as well as the difference in physical data, experts introduced the concept of cardiac index (CI). This value is calculated by the ratio of the IOC to the total surface area of the body, which is measured in square meters. The SI unit is l/min. m².
When transporting oxygen through a closed system, blood circulation plays the role of a kind of limiter. The highest indicator of minute volume of blood circulation obtained during maximum muscle tension, when compared with the indicator recorded under normal conditions, allows us to determine the functional reserve of the cardiovascular system and specifically the heart in terms of hemodynamics.
If a person is healthy, the hemodynamic reserve varies from 300 to 400%. The figures inform that without any danger to the body’s condition, a three- to four-fold increase in IOC, which is observed at rest, is possible. In people who regularly engage in sports and are physically well developed, this figure can exceed 700%.
When the body is in a horizontal position and any physical activity is excluded, the IOC is in the range from 4 to 5.5 (6) l/min. Normal SI under the same conditions does not leave the range of 2–4 l/min. m².
Relationship between the IOC and organs at rest
The amount of blood filling the circulatory system of a normal person is 5–6 liters. One minute is enough to complete a full circuit. With heavy physical work and increased sports loads, the IOC of an ordinary person increases to 30 l/min, and for professional athletes even more - up to 40.
In addition to physical condition, IOC indicators largely depend on:
- systolic blood volume;
- heart rate;
- the functionality and condition of the venous system, through which blood returns to the heart.
Systolic blood volume
Systolic blood volume refers to the amount of blood pushed by the ventricles into the great vessels during one heartbeat. Based on this indicator, a conclusion is made about the strength and efficiency of the heart muscle. In addition to systolic, this characteristic is often called stroke volume or VT.
Systolic volume of blood circulation is calculated by the amount of blood pushed by the heart into the vessels during one contraction
At rest and in the absence of physical activity, during one contraction of the heart, 0.3–0.5 volumes of blood are pushed out to diastole, filling its chamber. The remaining blood is a reserve, which can be used in case of a sharp increase in physical, emotional or other activity.
The blood remaining in the chamber becomes the main determinant that determines the functional reserve of the heart. The larger the reserve volume, the more blood can be supplied to the circulatory system as needed.
When the circulatory system begins to adapt to certain conditions, the systolic volume undergoes a change. Extracardiac nervous mechanisms take an active part in the process of self-regulation. In this case, the main effect is on the myocardium, or more precisely, on the force of its contraction. A decrease in the power of myocardial contractions leads to a decrease in systolic volume.
For the average person, whose body is in a horizontal position and does not experience physical stress, it is normal if the OC varies between 70–100 ml.
Factors influencing IOC
Cardiac output is a variable value, and there are quite a few factors that change it. One of them is pulse, expressed as heart rate. At rest and in a horizontal position of the body, its average is 60–80 beats per minute. Changes in pulse occur under the influence of chronotropic influences, and inotropic influences affect strength.
An increase in heart rate leads to an increase in minute blood volume. These changes play an important role in the process of accelerating the adaptation of the IOC to the relevant situation. When the body is exposed to extreme stress, there is an increase in heart rate by 3 or more times compared to normal. Heart rhythm changes under the chronotropic influence exerted by the sympathetic and vagus nerves on the sinoatrial node of the heart. In parallel with chronotropic changes in cardiac activity, inotropic effects may be exerted on the myocardium.
Systemic hemodynamics is also determined by the work of the heart. To calculate this indicator, it is necessary to multiply the data on the average pressure and the mass of blood that is pumped into the aorta over a certain time interval. The result informs how the left ventricle is functioning. To establish the work of the right ventricle, it is enough to reduce the resulting value by 4 times.
If cardiac output indicators do not correspond to the norm and there are no external influences observed, then this fact indicates abnormal functioning of the heart, therefore, the presence of pathology.
What is sudden cardiac arrest?
When the heart suddenly stops, it stops pumping blood.
Sudden cardiac arrest is not the same as a heart attack. A heart attack occurs when one or more of the arteries supplying blood to your heart becomes clogged or blocked. As a result, the heart muscle may suffer. This can be thought of as a problem with the “heart piping”. Sudden cardiac arrest can occur when the heart begins to beat at a dangerously fast rate. This can be thought of as an "electrical" heart problem. Even if the problem with the cardiac pipeline is corrected by angioplasty, bypass surgery, or some other method, the risk of sudden cardiac arrest still remains.
Causes of sudden cardiac arrest.
If you have heart failure or have had a heart attack, there is a chance that your heart muscles are damaged. In this case, the conduction (electrical) system of the heart may also suffer, creating a risk of sudden cardiac arrest. If this situation applies to you, consult with your doctor about the advisability of using an implantable defibrillator for safety reasons.
Sudden cardiac arrest has no warning signs.
Some people may experience palpitations or dizziness, which is a warning sign that a dangerous rhythm disorder may be occurring. But in the vast majority of cases, sudden cardiac arrest occurs without warning. There is no drug that is 100% effective in preventing sudden cardiac arrest. The most effective treatment for sudden cardiac arrest is defibrillation. Defibrillation is the application of a high-energy electrical shock to the heart to restore normal heart rhythm. To prevent death, defibrillation must be performed within a few minutes.
An implantable defibrillator is always ready.
Ambulance crews use external defibrillators. A small device implanted under your skin, an implantable cardioverter defibrillator, can also restore your heart's rhythm and save your life. An implantable defibrillator is always ready to help, monitoring your heart function around the clock. If your implantable defibrillator detects an abnormal rhythm, it automatically provides therapy. An implantable defibrillator is always ready to help you. You can consider it an ambulance that is always with you.
Decreased cardiac output
The most common causes of low cardiac output are disturbances in basic cardiac functions. These include:
- damaged myocardium;
- blocked coronary vessels;
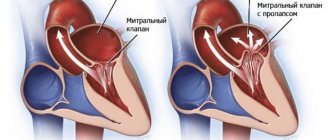
- abnormally functioning heart valves;
- cardiac tamponade;
- disrupted metabolic processes occurring in the heart muscle.
When cardiac output decreases and tissues are no longer supplied with nutrients, cardiogenic shock can occur.
The main reason leading to a decrease in cardiac output lies in the insufficient supply of venous blood to the heart. This factor has a negative impact on the IOC. The process is determined by:
- a decrease in the amount of blood involved in circulation;
- decrease in tissue mass;
- blockage of large veins and expansion of ordinary ones.
A decrease in the amount of circulating blood helps to reduce the IOC to a critical threshold. A shortage of blood begins to be felt in the vascular system, which affects the amount of blood returned to the heart.
When fainting occurs due to disorders in the nervous system, small arteries become dilated and veins become enlarged. The result is a decrease in blood pressure and, as a consequence, insufficient blood volume entering the heart.
If the vessels supplying blood to the heart undergo changes, they may partially block. This immediately affects peripheral vessels that are not involved in the supply of blood to the heart. The resulting reduced amount of blood sent to the heart causes low cardiac output syndrome. Its main symptoms are expressed:
- drop in blood pressure;
- low heart rate;
- tachycardia.
This process is accompanied by external factors: cold sweat, low volume of urination and changes in skin color (pallor, blueness).
The final diagnosis is made by an experienced cardiologist after carefully studying the test results.
Increased cardiac output
The level of cardiac output depends not only on physical activity, but also on the psycho-emotional state of a person. The functioning of the nervous system can reduce and increase the IOC index.
Sports activities are accompanied by an increase in blood pressure. Accelerating metabolism contracts skeletal muscles and dilates arterioles. This factor allows oxygen to be supplied to the muscles to the required extent. Loads lead to a narrowing of large veins, an increase in heart rate and an increase in the strength of contractions of the heart muscle. High blood pressure causes increased blood flow to the skeletal muscles.
Increased cardiac output is most often observed in the following cases:
- arteriovenous fistula;
- thyrotoxicosis;
- anemia;
- vitamin B deficiency.
In an arteriovenous fistula, the artery is directly connected to the vein. This phenomenon is called a fistula and comes in two types. A congenital arteriovenous fistula is accompanied by benign formations on the skin and can be located on any organ. In this variant, it is expressed by embryonic fistulas that have not reached the stages of veins or arteries.
Arteriovenous fistula
An acquired arteriovenous fistula is formed under the influence of external influence. It is created if there is a need for hemodialysis. Often a fistula becomes the result of catheterization, as well as a consequence of surgical intervention. Such a fistula sometimes accompanies penetrating wounds.
A large fistula provokes increased cardiac output. When it takes a chronic form, heart failure is possible, in which the IOC reaches critically high levels.
Thyrotoxicosis is characterized by a rapid pulse and high blood pressure. In parallel with this, not only quantitative changes in the blood occur, but also qualitative ones. An increase in the level of thyraxine is promoted by an abnormal level of erythropatine and, as a consequence, a decreased erythrocyte mass. The result is increased cardiac output.
With anemia, blood viscosity decreases and the heart is able to pump more of it. This leads to increased blood flow and increased heart rate. Tissues receive more oxygen, and accordingly, cardiac output and IOC increase.
Vitamin B1 deficiency is the cause of many pathologies
Vitamin B1 is involved in blood formation and has a beneficial effect on blood microcirculation. Its action significantly affects the functioning of the heart muscles. A lack of this vitamin contributes to the development of beriberi disease, one of the symptoms of which is impaired blood flow. With active metabolism, tissues stop absorbing the nutrients they need. The body compensates for this process by dilating peripheral vessels. Under such conditions, cardiac output and venous return can exceed the norm by two or more times.
Patient with low left ventricular ejection fraction
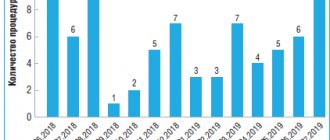
November 11, 2017 0
Introduction. Treatment of chronic heart failure (CHF) is one of the most socially significant problems in our country. According to epidemiological studies in Russia, there are more than 8 million people with symptoms of CHF. Decompensation of CHF causes hospitalization in hospitals, increasing cardiovascular mortality and disabling the working-age population. This clinical example shows the possibilities of modern methods of interventional treatment of CHF.
Description of the case. Patient I., 59 years old, was hospitalized with complaints of rapid irregular heartbeat, compressive pain and shortness of breath with minimal physical activity, swelling of the lower extremities, weakness, and decreased performance. At the age of 50, atrial fibrillation was diagnosed, and no attempts were made to restore sinus rhythm. On an outpatient basis he took cardiac glycosides, beta-blockers, and ACE inhibitors.
He was sent to the Federal Center for Agriculture (Astrakhan) to determine further tactics. According to ECHO-CS, dilatation of the left ventricle (LV) and left atrium (LA) was revealed: LA – 52 mm, LV EDV 297 ml, LV ESV 178 ml, LVEF 23%, diffuse LV hypokinesis, mitral regurgitation of the 2nd degree. The ECG shows AF, tachysystolic form with an average heart rate of 120 per minute. LBBB (QRS 158 ms).
Taking into account the pain syndrome, as well as to exclude the ischemic genesis of AF, a coronary angiography was performed: no coronary pathology was detected. Drug therapy was adjusted: rhythm-slowing therapy was intensified, diuretics and oral anticoagulants were added.
At a follow-up visit to the clinic after 3 months, against the background of recommended therapy, ECHO CS showed positive dynamics: LV EDV - 288 ml; LV ESV - 188 ml; LVEF - 35%, mitral regurgitation 2-2.5 degrees.
Considering the low LVEF and the presence of LBBB on the background of optimal drug therapy for three months, for the primary prevention of sudden cardiac death and treatment of CHF, implantation of a CRT with a cardioverter-defibrillator function was performed. The operation was uneventful; the left ventricular electrode was implanted into the lateral vein of the heart. After implantation, the patient was connected to a remote monitoring system, allowing him to remotely receive messages from the implanted device according to a programmed transmission schedule.
After 3 months, the device was tested - no malfunctions were detected, the percentage of biventricular stimulation (BVS) was 74%. Unmotivated shocks were delivered twice due to incorrect discrimination of AF with tachysystolic conduction to the ventricles. Subjectively, he notes an improvement in health (shortness of breath has decreased, swelling of the lower extremities has disappeared). On ECHO-CS, LV EDV is 208 ml; LV ESV - 123 ml; LVEF - 41%, mitral regurgitation grade 2.
Considering the need for 100% BVS, the occurrence of unmotivated shocks, and the tachysystolic form of AF, resistant to drug therapy, RFA of the AV junction was performed.
At discharge on the 4th day, during ECHO-CS, an increase in LVEF up to 50% and a decrease in LV size were noted - LV EDV - 203 ml, LV ESV - 101 ml.
Discussion. 15% of all patients with CHF have signs of electrical dyssynchrony (QRS complex duration more than 120 ms), which can be corrected by implantation of a cardiac resynchronization device. One of the important conditions for effective CRT is the presence of sinus rhythm in a patient with CHF and LBBB. The tactics of managing patients with CRT and atrial fibrillation (AF) in some cases is ambiguous and requires an individual assessment with the participation of a team of specialists (cardiologist, cardiac surgeon, electrophysiologist, functional diagnostics doctor).
To fully realize the effects of SRT, a BVS close to 100% is required. When the percentage of BVS decreases, regardless of the clinical effects of CRT, the cause of this condition should be verified. For drug-resistant types of often recurrent, persistent or permanent arrhythmias, in case of ineffective RFA of arrhythmia, the strategy of choice, which increases BVS to 100%, is the creation of artificial atrioventricular block.
Conclusion on use in clinical practice. Practicing physicians are often poorly informed about the possibilities of interventional treatment of CHF, and RFA of the AV junction is considered by many as a mutilating, unjustified procedure. This clinical case illustrates the high effectiveness of the interventional approach in cardiology, which, in combination with optimal drug therapy, can demonstrate significant clinical effects.
Cardiac output fraction and diagnosis
The concept of ejection fraction was introduced into medicine to determine the performance of the heart muscles at the time of contraction. It allows you to determine how much blood was pushed from the heart into the vessels. The unit of measurement is set to percentage.
The left ventricle is selected as the object of observation. Its direct connection with the systemic circulation makes it possible to accurately determine heart failure and identify pathology.
Ejection fraction is prescribed in the following cases:
- with constant complaints about heart function;
- chest pain;
- shortness of breath;
- frequent dizziness and fainting;
- low performance, rapid fatigue;
- swelling of the legs.
The initial analysis is carried out using ECG and ultrasound equipment.
What is an implantable defibrillator?
An implantable defibrillator is a device similar to a pacemaker (artificial pacemaker) that has been used since the early 90s. It is small in size - no larger than a pager - and is implanted under the skin of the upper chest. The device contains a battery and a microcomputer necessary to correct your rhythm. An implantable defibrillator is connected to the heart by thin, insulated wires called electrodes. If the device detects that your heart rhythm is abnormal, it sends electrical signals to restore it. Most implantable defibrillators last 5-7 years before needing to be replaced.
Fraction norm
During each systolic state, the heart of a person who is not experiencing increased physical and psycho-emotional stress throws up to 50% of the blood into the vessels. If this indicator begins to noticeably decrease, insufficiency is observed, which indicates the development of ischemia, heart disease, myocardial pathologies, etc.
A – normal fraction, B – 45% fraction
The ejection fraction norm is 55–70%. Its drop to 45% and below becomes critical. To prevent the negative consequences of such a decline, especially after 40 years, an annual visit to a cardiologist is necessary.
If the patient already has pathologies of the cardiovascular system, then in this case there is a need to determine an individual minimum threshold.
After conducting the study and comparing the data obtained with the norm, the doctor makes a diagnosis and prescribes appropriate therapy.
Ultrasound does not reveal the full picture of the pathology and, since the doctor is more interested in identifying the cause of this disease, most often it is necessary to resort to additional studies.
Cardiac ejection fraction on ultrasound
Treatment of low fraction level
Low cardiac output is usually accompanied by general malaise. To normalize health, the patient is prescribed outpatient treatment. During this period, constant monitoring of the functioning of the cardiovascular system is carried out, and the therapy itself involves taking medications.
In particularly critical cases, surgery may be performed. This procedure is preceded by the identification of a severe defect or serious disorders of the valve apparatus in the patient.
Surgery becomes inevitable when low cardiac output becomes life-threatening for the patient. In general, conventional therapy is sufficient.
Self-treatment and prevention of low ejection fraction
To normalize the ejection fraction, you must:
- Introduce control over the liquids taken, reduce their volume to 1.5–2 liters per day.
- Avoid salty and spicy foods.
- Switch to dietary foods.
- Reduce physical activity.
Preventive measures to avoid deviations from the normal cardiac ejection fraction include:
- rejection of bad habits;
- maintaining a daily routine;
- eating iron-containing foods;
- exercises and light gymnastics.
If there is the slightest malfunction of the heart or even suspicion of these manifestations, you must immediately see a cardiologist. Timely detection of pathology greatly simplifies and speeds up its elimination.
How does an implantable defibrillator work?
Depending on the programmed mode, the implantable defibrillator may initially send low-energy, painless electrical signals to restore rhythm. If they do not work, a stronger shock is sent. People describe this discharge as a sudden feeling of discomfort, sometimes even painful, but quickly passing. Often everything ends before you understand what actually happened. Another positive thing is that an implantable defibrillator protects you constantly, 24 hours a day.